- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Reverse Vertebral Column Decancellation (RVCD): A New Technique for Correction of The Rigid Thoracic Lordoscoliosis and Literature Review
Luis E Carelli, Fabio Fagundes, Alderico Girão and Silvia M Flores Taracena*
Department of Spine Surgery, National Institute of Orthopedics and Traumatology (INTO), Brazil
*Corresponding author:Silvia M Flores Taracena, Department of Spine Surgery, National Institute of Orthopedics and Traumatology (INTO), Avenida Brazil 500, Caju, RJ, 20940-070, Rio de Janeiro, Brazil
Submission: November 05, 2025;Published: November 14, 2025

ISSN 2637-7748
Volume6 Issue1
Abstract
Introduction: Rigid lordoscoliosis is uncommon and challenging to treat. Patients can develop
respiratory impairment as well as sagittal and coronal imbalance, leading to low health-related quality
of life. The surgical management of this type of deformity is not well defined in literature. We describe
a new technique we call “Reverse Vertebral Column Decancellation” (RVCD) for the treatment of rigid
hyper lordosis.
Methods: Case report of a 15-year-old female patient diagnosed with early-onset scoliosis, who
had undergone several surgical procedures, developing a rigid lordotic deformity. The preoperative
radiographic findings were a thoracic hyper lordosis (-7.3°) with positive sagittal imbalance with a
sagittal vertical axis (+29.5 mm) and a negative Pelvic Tilt (PT) of -39°. Surgical treatment using the
RVCD technique was chosen. RVCD entails complete resection of the posterior elements followed by a
horizontal linear osteotomy of the posterior half of the vertebral body and a wedge decancellation of
the anterior base of the lateral and anterior cortical bone of the latter, resulting in a Y-shaped osteotomy.
Anterior closure is performed by posterior distraction to increase kyphosis.
Results: The patient had a postoperative correction of 51.5°, resulting in a thoracic kyphosis of +44.2°.
There was a change in PI (pre: 19.7°, post: 14.4°) and a reduced but persistent negative pelvic tilt (-35.6°).
Computed tomography scan six months after the procedure showed bone fusion. No neurological and
infectious complications were reported during three years of follow-up.
Conclusion: The RVCD proved to be an effective and safe option for the treatment of rigid hyperlordotic
deformity.
Keywords: Hyper lordosis; Lordoscoliosis; Spinal osteotomies; Vertebral column decancellation
Introduction
Rigid lordoscoliosis is an uncommon deformity and is challenging to treat. It causes respiratory impairment more frequently than kyphoscoliosis and therefore must be treated early to avoid cardiopulmonary complications [1]. Patients often develop sagittal and coronal imbalance, leading to low measures of health-Related Quality of Life (H-RQL) [2]. In surgical cases these deformities can be addressed by combined (anterior and posterior) access or by a solely posterior approach. The combined access includes a first stage of anterior release, which may or may not contemplate traction and a second stage of posterior instrumentation and fusion [3-6]. There are authors who advocate the “posterior only” approach using pedicle screws. They claim they achieve the same correction without the anterior approach and avoid the complications associated with it [7-9]. Vertebral Column Resection (VCR) is a surgical option for the management of rigid hyperlordosis due to deformities in the coronal and sagittal planes with good outcomes. However, it has a high rate of complications, including significant blood loss, instability and neurological deficits [10]. In order to avoid the complications associated with VCR and by analogy to the management of rigid kyphotic deformities using another technique called “Vertebral Column Decancellation (VCD)”[11] we applied the same principle to the treatment of rigid hyperlordosis in a novel surgical technique that we call “Reverse Vertebral Column Decancellation” (RVCD), using an exclusively posterior approach.
Methods
Case presentation
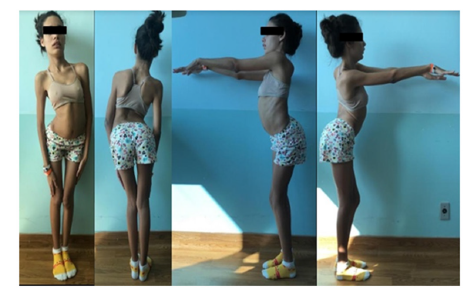
This is a case report of a 15 years-old female patient with earlyonset idiopathic scoliosis who presented with a thoracolumbar deformity. She had undergone correction by the Shilla growth guidance procedure at age 6 [12]. Two years after that first surgery, she developed proximal junctional kyphosis, requiring extension of the fusion to T2. At age 10, she presented persistent infection in the surgical site, requiring the removal of all the instrumentation. Subsequently she developed a progressive increase in thoracic lordosis. As seen in Figure 1, the physical examination revealed a significant anterior trunk deviation, as well as compensatory mechanisms in the knee and hip joints.
Figure 1:Preoperative clinical photos showing anterior trunk deviation with thoracic hyperlordosis, knee flexion and pelvic anteversion.
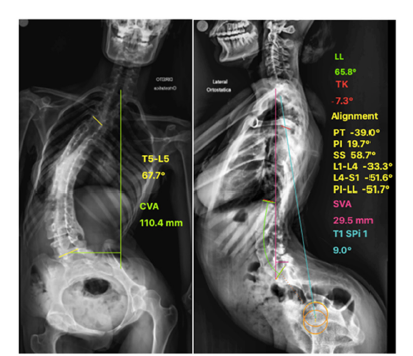
Radiographic findings
Using a full-length standing spine radiograph, preoperative spinopelvic alignment measurements were performed with Surgimap® software. The measurements were: anterior deviation of the sagittal vertical axis (SVA: +29.5mm); a negative pelvic tilt (PT: -39°), as the femoral heads were posterior to the midpoint of the sacral dome; increased lumbar lordosis (LL: -65.8°); pelvic incidence (PI: +19.7°) and the thoracic spine was in lordosis (CT -7.3°) (Figure 2).
Figure 2:a) Preoperative anteroposterior full-length standing spine radiograph shows significant posterior fusion bone mass and parameters of coronal alignment b) Lateral radiograph with the parameters of sagittal alignment. Note the anterior deviation of the sagittal vertical axis and the negative pelvic tilt, as the femoral heads are posterior to the midpoint of the sacral dome.
Surgical technique
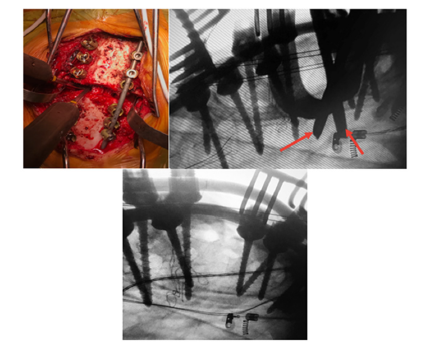
A standard midline skin incision with subperiosteal dissection to expose the bony structures of the posterior elements. All pedicle screws are then inserted using a freehand placement technique [13]. After that, the Reverse Vertebral Column Decancellation technique itself begins with resection of the posterior elements, including the lamina and pedicles and the insertion of a temporary rod in one side to avoid spine translation, followed by a linear horizontal osteotomy of the posterior half of the vertebral body (Figure 3A & 4A). With the aid of intraoperative fluoroscopy, two osteotomes were positioned obliquely (Figures 3B & 4B) to mark the appropriate location for decancellation, (Figure 3C) if needed, the surgeon can tilt the surgical table before doing the osteotomy for better visualization. This is performed in a wedge shape, with its base anterior, resulting in a “Y”-shaped osteotomy, the vertebral osteotomy was realized on the contralateral side of the temporary rod. Next, we repeated the same steps on the other side, always leaving a temporary rod contralateral to maintain stability. Anterior vertebral decancellation was done with reverse angle curette and Ribbon malleable retractors. Next, anterior closure of the wedge is performed through posterior distraction to increase the kyphosis (Figure 3D), which is confirmed by intraoperative fluoroscopy (Figure 4C). This technique has the same concept of the VCD osteotomy and V-Y osteotomy doing the hinge of the correction in the middle column to avoid stretching the neurovascular structures. [11,14] If there is a gap of more than 5 mm, a structural bone graft can be placed to increase the fusion area (Figure 3E). In the case described, a fibular allograft from a tissue bank was used.
Figure 3:Illustration showing the steps in the Reverse Vertebral Column Decancellation. a) Wide resection of posterior elements including the pedicles of the level to be osteotomized, with linear osteotomy of the posterior half of the vertebral body. b) Oblique positioning of the osteotomes at the desired angle for correction. c) Wedge decancellation of the anterior half of the vertebral body. d) Closing the wedge-shaped osteotomy of the anterior base by posterior distraction, with consequent formation of an opening wedge in the posterior half of the vertebral body. e) If there is a gap of more than 5 mm, a structural bone graft can be placed.
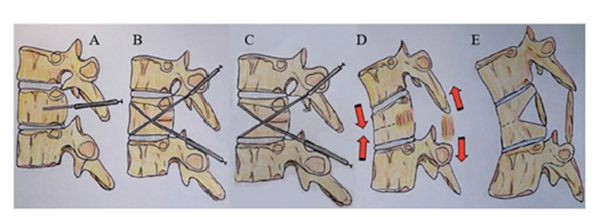
Figure 4:a) Intraoperative photograph b) Fluoroscopy image showing divergent positioning of the osteotomes (red arrows) at the desired angle for correction. Then, posterior distraction is performed to increase the kyphosis. c) Closure of the anterior wedge confirmed by fluoroscopy.
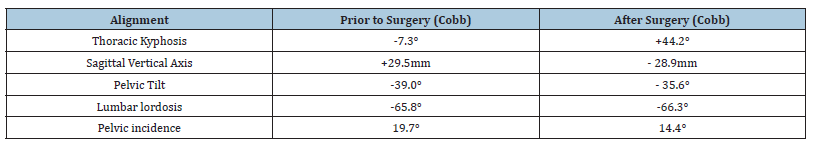
Results
There were no intraoperative or post-operative complications. Operative time was 415 minutes; blood loss was 450cc. The patient spent the first forty-eight post-operative hours in the surgical ICU and was discharged from the hospital after 8 days. The patient was followed for two years. Computed Tomography (CT) performed 6 months after the procedure showed bone fusion. Clinically, the trunk alignment was correct with a consequent improvement in the compensatory mechanisms of the hip and knee (Figure 5). The radiographic parameters of sagittal alignment in the pre- and postoperative period are presented in Table 1 and are illustrated in Figure 6, with improvement of sagittal alignment. Figure 6 shows the radiographic parameters of three years follow up.
Figure 5:One-year postoperative clinical photographs showing significant improvement in trunk balance and compensatory mechanisms of the hips and knees.
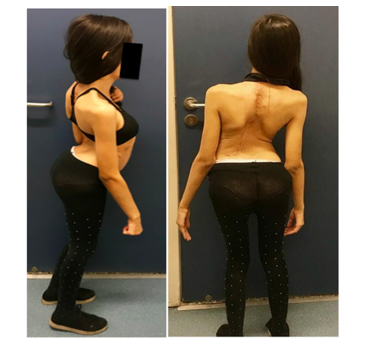
Figure 6:a) Anteroposterior. b) Lateral postoperative full-length standing spine radiographs showing significant improvement of the sagittal alignment and spinopelvic parameters. c) Six-month postoperative sagittal and coronal CT reconstruction showing osteotomy healing.
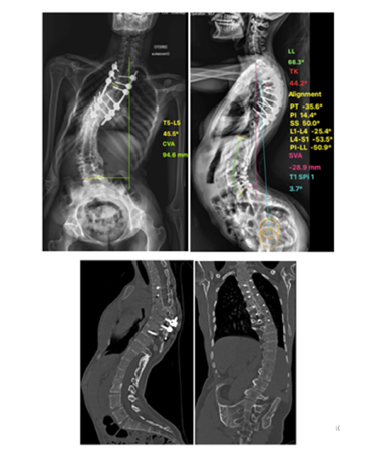
Table 1:Radiographic Analysis
Discussion
Surgical treatment of lordoscoliosis can be performed using several techniques that include a combined anterior and posterior access or a posterior only approach. In cases with a more flexible deformity, the Posterior Column Osteotomy (PCO) is used in the treatment of hyperkyphosis. Through mobilization and posterior thoracic distraction, the PCO technique is used to correct the hyperlordosis [15]. However, we know that the increase in kyphosis by using an exclusively posterior approach with PCO is not easily achieved, as demonstrated in the literature about the treatment of idiopathic scoliosis in adolescents with hypokyphosis [16]. It is also important to emphasize that this correction needs to be carefully controlled because excessive posterior distraction can result in damage to the spinal cord and increase the risk of pseudarthrosis [17]. For the treatment of flexible hyperlordosis, in addition to the Ponte technique, [18] Winter et al and Bradford et al described a combined approach for thoracolumbar hyperlordosis. A procedure with ribosteotomies is performed to create an unstable chest combined with resections of anterior wedges of the vertebral bodies, followed by posterior instrumentation. Winter had an average correction in his series of 51°, [4] and Bradford had an average correction of 65° [5]. Song et al described a two-stage procedure for these deformities, where the first surgery included anterior discectomy, release and fusion of T8 to the sacrum, followed by transfemoral traction with the hip and knee flexed at 90º for two weeks to decrease lordosis. The second operative phase consisted of posterior instrumentation and fusion of T2 to the pelvis using the Luque and Galveston technique, achieving a correction of the hyperlordosis of 32°. With the dual approach there is a negative impact on pulmonary function, which can be deleterious to the patient, especially with this type of deformity. Other authors also performed double approach using anterior spinal osteotomy followed by posterior fusion for treatment of rigid hyperlordosis [19]. Despite our patient did not have any clinical signs or complains of pulmonary malfunction, lordoscoliosis needed to be corrected to also improve lung volumes and vital capacity and we planned a posterior osteotomy also to avoid any disturbance in pulmonary function [6,20].
Cases with greater curve rigidity require larger osteotomies. One surgical option is the “Reverse Smith Petersen Osteotomy” (RSPO). In this combined approach, an anterior base and apex (center of rotation) wedge in the posterior wall is resected. Next, the spine is flexed by posterior distraction, causing an increase in kyphosis in an area with hypokyphosis or lordosis [21]. In our case, the osteotomy apex is in the middle column of vertebral body, closer to the center of rotation of the vertebra avoiding excessive distraction of the posterior aspect, decreasing neurologic risk. In this regard, to make the correction more gradual, Kee-Yonh Ha et al described the “Posterior Multilevel Vertebral Osteotomy (PMVO)”, which consists of a transverse osteotomy of the vertebral body performed posteriorly at multiple levels. The authors argue that PMVO can increase flexibility even in a rigid spine with a fusion mass, allowing the degree of correction to be distributed across the osteotomized area [8,9]. Finally, VCR is a plausible option in these cases, due to adequate decompression and the possibility of major corrections of the coronal and sagittal balance. However, it causes considerable instability, great blood loss and entails considerable risk of a neurological deficit [10]..
Table 2:Sagittal Correction of the Lordotic Deformities Obtained with Different Techniques A/P = Anterior-Posterior Approach, RSPO=Reverse Smith Peterson Osteotomy, PMVO = Posterior Multilevel Vertebral Osteotomy, RVCD=Reverse Vertebral Column Decancellation
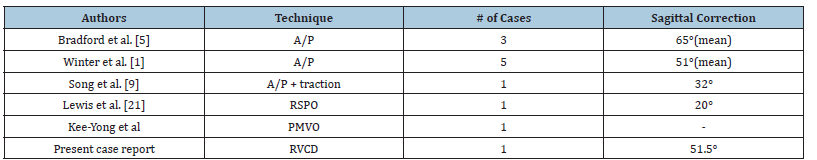
Following this principle for our patient with a rigid hyperlordosis and scoliosis-hers likely the crankshaft phenomenon [22] a consequence of the posterior fusion of the spine at an early age-we proposed a novel three-column osteotomy (3CO) technique for these cases of rigid thoracic lordosis, which we named “Reverse Vertebral Column Decancellation” (RVCD). With a single level 3CO we obtained 51.5° of correction, which is superior to the results of most of the previous case and series reports using other techniques (summarized in Table 2). Moreover, the technique yielded reciprocal sagittal alignment changes improving the global sagittal alignment with a postoperative SVA of -28.9 mm [23]. When compared to the VCR, we believe that RVCD-with its controlled shortening of the anterior column-entails less neurological and vascular risk during the correction. RVCD also has the advantage of promoting greater bone contact in the osteotomized area, improving the chances for consolidation [11]. We recommend that this technique should be selected carefully and be performed with neuromonitoring to avoid possible neurological compromise.
Surprisingly, Pelvic Incidence (PI), considered a morphological parameter, was changed from 19.7° preoperatively to 14.4° postoperatively. Similarly, Raphael Vialle et al. reported 15 cases of neuromuscular lumbar hyperlordosis in which the pelvic incidence was significantly modified [22]. Another parameter that has atypical behavior is pelvic tilt, because in hyperlordosis the psoas muscle has its function altered by its abnormal course between the spine and the proximal end of the femur, which in this case was located posterior to the center of the sacral dome. Instead of acting as a hip flexor, it becomes a lumbar spine extensor. In most cases in the series by Vialle et al, lumbar hyperlordosis is responsible for the pelvic “anteversion” and on the lateral radiographs the pelvic tilt appeared inverted, with a negative value,[24] a phenomenon similar to that which occurred in our patient. In the case described in this study, the patient showed an improvement in the pelvic tilt, though it continued to be negative.
Conclusion
Reverse Vertebral Column Decancellation (RVCD) proved to be a safe and effective treatment for this unusual case and may be a useful option for other rigid thoracic hyperlordotic deformities.
References
- Winter RB, Lovell WW, Moe JH (1975) Excessive thoracic lordosis and loss of pulmonary function in patients with idiopathic scoliosis. J Bone Joint Surg Am 57: 972-977.
- Glassman SD, Berven S, Bridwell K, Harton W, Diman JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30: 682-688.
- Yamin S, Li L, Xing W, Tianjun G, Yupeng Z (2008) Staged surgical treatment for severe and rigid scoliosis. J Orthop Surg Res 3: 26.
- Winter RB (1992) Surgical correction of rigid thoracic lordoscoliosis. J Spinal Disord 5(1): 108-111.
- Bradford DS, Blatt JM, Rasp FL (1983) Surgical management of severe thoracic lordosis. A new technique to restore normal kyphosis. Spine 8(4): 420-428.
- Song, EW, Lenke LG, Schoenecker PL (2000) Isolated thoracolumbar and lumbar hyperlordosis in a patient with cerebral palsy. J Spinal Disord 13(5): 455-460.
- Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH (2006) Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine 31(20): 2386-2391.
- Ha KY, Suh SW, Kim YH, Kim SI (2017) Long-term management of congenital lordoscoliosis of the thoracic spine. Eur Spine J 26(1): 47-52.
- Suh SW, Modi HN, Yang J, Song HR, Jang KM (2009) Posterior multilevel vertebral osteotomy for correction of severe and rigid neuromuscular scoliosis: A preliminary study. Spine 34(12): 1315-1320.
- Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, et al. (2002) Posterior vertebral column resection for severe spinal deformities. Spine 27(21): 2374-2382.
- Wang Y, Lenke LG (2011) Vertebral column decancellation for the management of sharp angular spinal deformity. Eur Spine J 20(10): 1703-1710.
- McCarthy RE, Luhmann S, Lenke L, McCullough FL (2014) The Shilla growth guidance technique for early-onset spinal deformities at 2-year follow-up: a preliminary report. J Pediatr Orthop 34(1): 1-7.
- Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD (2004) Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine 29(3): 333-342.
- Mehdian H, Arun R, Aresti NA (2015) V-Y vertebral body osteotomy for the treatment of fixed sagittal plane spinal deformity. Spine J 15(4): 771-776.
- Ponte A, Vero B, Siccardi GL (1984) Surgical treatment of scheuermann’s hyperkyphosis. In: Winter RB (Editor). Progress in spinal pathology: Kyphosis. Auto Gaggi, pp. 75-80.
- Floccari LV, Poppino K, Greenhill DA, Sucato DJ (2021) Ponte osteotomies in a matched series of large AIS curves increase surgical risk without improving outcomes. Spine Deform 9(5): 1411-1418.
- Pizones J, Sánchez-Marisca F, Zúñiga L, Izquierdo E (2015) Ponte osteotomies to treat major thoracic adolescent idiopathic scoliosis curves allow more effective corrective maneuvers. Eur Spine J 24(7): 1540-1546.
- Shah SA, Dhawale AA, Oda JE, Yorgova P, Neiss GI, et al. (2013) Ponte osteotomies with pedicle screw instrumentation in the treatment of adolescent idiopathic scoliosis. Spine Deform 1(3): 196-204.
- McMaster MJ, Carey RP (1985) The lumbar theco-peritoneal shunt syndrome and its surgical management. J Bone Joint Surg Br 67(2): 198-203.
- Filatov EY, Ryabykh SO, Savin DM, Naumov DG, Simonovich AE (2022) Congenital lordosis and lordoscoliosis: State of the problem (literature review). Genij Ortopedii 28(5): 720-725.
- Lewis SJ, Gray R, David K, Kopka M, Magana S (2010) Technique of Reverse Smith Petersen Osteotomy (RSPO) in a patient with fixed lumbar hyperlordosis and negative sagittal imbalance. Spine 35(15): E721-E725.
- Dubousset J, Herring JA, Shufflebarger H (1989) The crankshaft phenomenon. J Pediatr Orthop 9(5): 541-550.
- Blondel B, Lafage V, Schwab F, Farcy JP, Bollini G, et al. (2012) Reciprocal sagittal alignment changes after posterior fusion in the setting of adolescent idiopathic scoliosis. Eur Spine J 21(10): 1964-1971.
- Vialle R, Khouri N, Glorion C, Lechevallier J, Morin C (2007) Lumbar hyperlordosis of neuromuscular origin: Pathophysiology and surgical strategy for correction. Int Orthop 31(4): 513-523.
© 2025 Silvia M Flores Taracena. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






