- Submissions

Full Text
Research in Pediatrics & Neonatology
Medical Education Vis-A-Vis National Medical Commission in India
Vithalrao Dandge*
Institute of Medical Sciences, India
*Corresponding author:Vithalrao Dandge, Institute of Medical Sciences, India
Submission: July 27, 2019; Published: August 09, 2019

ISSN: 2576-9200 Volume3 Issue4
Abstract
A 1-day-old neonate with 1.4kg birth weight, with left sided gastroschisis, complicated by complete dissociation at gastro-oesophageal junction was managed by primary anastomosis and ventral hernia creation. The patient had prolonged post-operative hospital stay in view of sepsis and delayed tolerance of parenteral feeds and doing well in follow up.
Case Report
A 1-day-old neonate with birth weight 1.4kg, born at 36 weeks of gestation, presented to us with left gastroschisis. At presentation, baby was dehydrated and had matted bowel protruding from left abdominal wall defect (Figure 1). After initial resuscitation, baby was taken for emergency operation. She had multiple attempts for difficult intubation. On extending defect of gastroschisis in midline, it revealed nasogastric tube was in peritoneal cavity and there was total dissociation of stomach and oesophagus at gastro-oesophageal junction (GEJ) (Figure 2). There was no other perforation or atresia noted in bowel after warm saline wash and wrapping of matted bowel in warm saline soaked mops. A full thickness primary anastomosis was contemplated, and ventral hernia was created with skin cover as closure of rectus muscles lead to high abdominal pressure (18mmHg). Baby was shifted to neonatal intensive care unit (NICU) and was weaned off ventilator support after two days. The post-operative period was stormy in view of Acinetobacter sepsis and prolonged naos-gastric aspirates. We were able to start slowly infusion feeds and parental nutrition was tapered. Baby was discharged from NICU at one month of age and has been in follow up for one month with present weight of 2.76kg.
Figure 1:
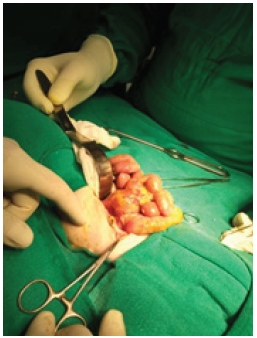
Figure 2:

Discussion
The defect of gastroschisis may be explained by various theories including abnormal involution of umbilical vein and vitelline artery and failure of mesoderm to form body wall. The defect spares the midline and does not involve the umbilicus. It is usually paramedian and is more common on the right side. The pathogenesis of leftsided gastroschisis may be explained by early regression of the left umbilical vein [1] proposed that slight mispositioning of the yolk stalk to the left of the midline in the setting of wall fold failure could lead to left-sided defects. This theory was appealing because it explained both right-and left-sided gastroschisis [1]. The work by [2] supported the concept of a multifactorial aetiology of gastroschisis, which involves both genetic issues and environmental factors [2] Complicated gastroschisis is known for its high morbidity and mortality. The index case had complete dissociation at GEJ, which may be due to multiple attempts at intubation leading to prolonged course on bag and mask ventilation in between and causing dissociation at GEJ [3] studied various factors that influenced length of hospital stay in a study on 49 neonates undergone primary repair of gastroschisis [3]. They showed that slower onset of full enteral feeding acted as a protective factor, decreasing length of hospital stay by 3.6% [4] studied 114 neonates with gastroschisis and found that birth weight, compromised bowel and sepsis are the main variables significantly influencing outcome in gastroschisis [4,5] did retrospective cohort study of 105 gastroschisis babies and cited significant factors for successful feeding including female gender, gestational age>36 weeks, age at surgery less than 10h and postoperative extubation time<4 days, all with P value<0.001) [2]. In the index case, female gender and early postoperative extubation were favorable factors but delayed presentation and stormy postoperative period acted as factors for delayed parenteral feeds. Parenteral nutrition is an important survival factor in early days of gastroschisis operated neonates.
Conclusion
We present this index case of left gastroschisis complicated by dissociation at gastro-oesophageal junction probably due to prolonged bag and mask ventilation for difficult intubation. We propose gentle handling of gastroschisis neonates at all levels of care, including anesthesia, surgery and intensive care.
References
© 2019 Vithalrao Dandge*. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






