- Submissions

Full Text
Open Access Biostatistics & Bioinformatics
Turning the Abundant Clinical Data into Something Usable is the Key to Achieve UHC by 2030 in India
Suresh Kishanrao*
Family Physician & Public Health Consultant, India
*Corresponding author: Suresh Kishanrao, Family Physician & Public Health Consultant, A 1102, Assetz Lumos, Bengaluru- 560022, India
Submitted: October 06, 2025; Published: January 22, 2026

ISSN: 2578-0247 Volume4 Issue 2
Abstract
In this study, bifurcation analysis and multi-objective nonlinear model predictive control is performed on a cholera disease model. Bifurcation analysis is a powerful mathematical tool used to deal with the nonlinear dynamics of any process. Several factors must be considered, and multiple objectives must be met simultaneously. The MATLAB program MATCONT was used to perform the bifurcation analysis. The MNLMPC calculations were performed using the optimization language PYOMO in conjunction with the state-of-the-art global optimization solvers IPOPT and BARON. The bifurcation analysis revealed the existence of a limit point. The MNLMC converged to the utopia solution. The limit point (which causes multiple steady-state solutions from a singular point) is very beneficial because it enables the multiobjective nonlinear model predictive control calculations to converge to the Utopia point (the best possible solution) in the model.
Keywords:Bifurcation; Optimization; Control; Cholera
Introduction
Introduction System’s (SRS) Statistical Report for 2023. SRS STATISTICAL REPORT provides data on i) the Total Fertility Rate (TFR) ii) Gross Reproductive Rate (GRR), iii) Proportion of Elderly and Average Life Expectancy (ALE) iv) Crude Birth Rate (CBR), v) crude death rate (CDR) and vi) infant mortality (IMR) rates at Natural Revenue Division, Provinces and National level [1]. A health information system is defined as “a mechanism for the collection, processing, analysis & transmission of information required for organizing and operating health services, and also for research and training”. Health information is an integral part of the national health system. National Digital Health Mission (NDHM) launched on 15 August 2022, aiming to build an integrated digital health ecosystem via unique health ID, secure EHR, telemedicine and e-pharmacy to revolutionize healthcare delivery [2]. Health Information is used i) To measure the health status of the people & to quantify their health problems & medical as well as health care needs ii) For local, national & international comparisons of health status iii) For planning, administration & effective management of health services & programs iv) For assessing whether health services are accomplishing their objectives in terms of their effectiveness & efficiency v) For assessing the attitudes & degree of Client satisfaction with the health services vi) For research into problems of health & diseases.
Accurate estimations of demographic trends are vital for planning. India has both a direct and an indirect system to count births and deaths. Estimates of the number of births and deaths in India every year come from two key sources: The Civil Registration System (CRS) which relies on registered events, & the Sample Registration System (SRS), which is a large demographic survey. For the time being the Sample Registration System (SRS) stands as India’s most reliable source for estimating birth rates, death rates, and other vital statistics since the 1960s. This comprehensive demographic surveillance system bridges critical data gaps in a country where civil registration systems have historically been incomplete. By combining continuous enumeration with halfyearly surveys across carefully selected sample units, SRS provides policy makers, researchers, & public health professional essential population indicators, for India’s vast and diverse landscape [3].
National CBR was 18.4/per 1000 population in 2023. While rural India registered a higher birth rate of 20.3/1000, in contrast to urban areas had an CBR of 14.9/1000 for the same period. National CDR was 6.4/1000 population with men recording a higher death rate (7.2) compared to women (5.7) both in rural and urban areas. While the rural India had a death rate of 6.8 and urban regions death rate of 5.7 respectively. National Infant Mortality Rate (IMR) has dropped to 25/1000 live births in 2023, from 129 deaths per 1,000 live births (in 1971). IMR in rural regions declined by 8 points from 36 (in 2018) to 28 (in 2023) and urban regions recorded a decline of 5 points, from 23 (in 2018) to 18 (in 2023) in last 5 years. This article is a review of the 2023 SRS data of three of the six indicators from the lens of Public Health professional & suggesting way forwards to achieve national commitment of Universal Health Care 2030 as India’s healthcare future hinges on data curation, standardization & responsible sharing, & use [4].
Key Findings of SRS 2023 Report [1,3]
Crude birth rate: National CBR was 18.4/1000 population
CBR variations by states: The birth rate of Bihar stood highest at 25.8 in 2023, among all States/Union Territories (UTs); followed by Uttar Pradesh (UP) (23.6), Rajasthan (22.9), Madhya Pradesh (MP) (22.5) and Chhattisgarh (22.3), while, Andaman & Nicobar Islands registered the lowest CBR of 10.1, followed by Kerala (12.3); Tamil Nadu (TN) (12.0), Punjab (13.8) and Maharashtra & West Bengal (WB) (14.0) each.
Rural and urban difference: While rural India registered a higher birth rate of 20.3, in contrast urban areas had a CBR of 14.9 for the same period.
Crude death rate: National CDR was 6.4/1000 population.
CDR variations by states: Chhattisgarh had the highest death rate at 8.3, followed by Odisha (7.7), Kerala (7.2), Punjab (7.3) Andhra Pradesh (AP) (6.9) and Karnataka (6.8) while Chandigarh registered lowest CDR of 4.0, followed by Delhi/Manipur (4.5) each, Jammu & Kashmir (5.6). At national level, men recorded a higher death rate (7.2) compared to women (5.7) both in rural and urban areas of the country. CDR in Rural and Urban regions was at 6.8 and 5.7, respectively.
IMR: National Infant Mortality Rate (IMR) has dropped to record low to 25 in 2023, from 32 infant deaths per 1,000 live births (in 2018). IMR in rural regions decreased by 8 points from 36 to 28 (in 2023) and urban regions recorded a decline of 5 points, from 23 to 18 in last 5 years. Among the sates Chhattisgarh, UP and MP registered the highest IMR i.e. at 37 each; followed by Odisha and Assam (30); and Jharkhand & Rajasthan (29), whereas Manipur recorded a lowest IMR, at 3, followed by UT Ladakh (4), Kerala (5), Goa/Sikkim (6) each, UTs Chandigarh (7) and Puducherry (7).
Life expectancy: According to the United Nations (UN), in 2023 life expectancy in India was 72.00 years (70.52 for male, 73.60 for female). From 1960 to 2023, Life Expectancy changed by +26.4 years. It improved to current level from lowest level of 45.6 years in 1965. From SRS 2023 Expectation of life at birth for India has been estimated at 70.3 years for the period 2019-23, exhibiting increase of 0.4 years from 2018-22. The life expectancy at birth varies from 64.6 in Chhattisgarh to 75.1 in Kerala. The expectation of life at birth is 69.1 years in rural areas and 73.1 years in urban areas for 2019-23, which amounts to an increase of 0.5 years for rural & by 0.2 years in urban areas as compared to 2018-22. At the national level, the life expectancy at birth for males has been estimated at 68.5 years and that for females, at 72.5 years.
Life expectancy: According to the United Nations (UN), in 2023 life expectancy in India was 72.00 years (70.52 for male, 73.60 for female). From 1960 to 2023, Life Expectancy changed by +26.4 years. It improved to current level from lowest level of 45.6 years in 1965. From SRS 2023 Expectation of life at birth for India has been estimated at 70.3 years for the period 2019-23, exhibiting increase of 0.4 years from 2018-22. The life expectancy at birth varies from 64.6 in Chhattisgarh to 75.1 in Kerala. The expectation of life at birth is 69.1 years in rural areas and 73.1 years in urban areas for 2019-23, which amounts to an increase of 0.5 years for rural & by 0.2 years in urban areas as compared to 2018-22. At the national level, the life expectancy at birth for males has been estimated at 68.5 years and that for females, at 72.5 years.
Total Infertility Rate (TFR): India’s TFR was 1.9 (in 2023), down from 2.0 (in 2022) & 5.2 in 1971. A total of 18 states &UTs now have TFR below the replacement level.
TFR variations by States: Bihar recorded the highest TFR among all Indian states i.e. at 2.8; followed by UP (2.6), MP (2.5), Rajasthan (2.3), and Chhattisgarh (2.2). On the other hand, Delhi recorded the lowest TFR of 1.2; followed by WB & TN (1.3), Maharashtra (1.4), Kerala & AP (1.5).
Proportion of elderly people: The proportion of the elderly people in India (60+), has increased by 0.7% percentage points annually, to form 9.7% of the population. Kerala (15%) has the largest proportion of elderly followed by Assam (7.6%) and Delhi (7.7%).
Gross Reproductive Rate (GRR): It is an indicator for fertility that accounts for future mothers and measures the average number of female children a woman is expected to give birth during her entire reproductive span. GRR for 2023 is projected at 0.9. while GRR for major states/UTs range from 0.6 (Delhi, WB, and TN) to 1.3 (Bihar).
Discussion
India spends 1.3% of its GDP on public healthcare, compared to the global average of 6%. (World Bank, 2024) and people spend 63% of healthcare costs from their Pockets, which disproportionately affects low-income families. Most health care workforce shortage is reflected in 1 doctor per 1,456 people, against the WHO recommendation of 1:1,000. The Sources of health information in India include a) Census done once a decade b) Registration of vital events c) Sample registration system d) Notification of diseases e) Hospital Records constitute tip of Iceberg f) Disease Registers- A register is a permanent record for each case that can be followedup e.g., Tuberculosis Register, Leprosy Register, Filariasis Register etc. g) IDSP-integrated disease surveillance project, lunched in November 2004 h) Cancer Registry to collect, store and manage data on persons with Cancer since 1982. i) Epidemiological surveillance system for endemic diseases like, Malaria, Filaria j) Other Health Service Records like Records of hospitals OPD • Primary Health Centers • Private practitioners • Maternal & Child Health Centers • School health records • NCD clinics. K) Health Manpower Statistics • State Medical/ dental / Nursing Council can provide information of the respective health manpower. L) NFHS a large-scale, multi-round survey conducted in a representative sample of households throughout India. Five rounds of the survey have been conducted since - NFHS -1 (1992 - 93) - NFHS -2 (1998 - 99) - NFHS -3 (2005 - 06) - NFHS -4 (2014 - 15) - NFHS -5 (2019 -20). M) Environmental Health Data of Air, water & noise pollution, Industrial intoxicants, Harmful food activities, Inadequate waste disposal. N) Ayushman Bharat (AB) provides health coverage to over 500 million beneficiaries, offering free secondary and tertiary care to millions. Though AB Largest government healthcare scheme globally, it is still beyond the reach of most needy remote Rural Tribal and Urban poor population [4].
Accurate estimations of demographic trends are vital for planning. India has both a direct and an indirect system to count births and deaths. Estimates of the number of births and deaths in India every year come from two key sources: the Civil Registration System (CRS) which relies on registered events, & the Sample Registration System (SRS), which is a large demographic survey. In 2000, the system was revamped to enhance data quality and streamline reporting. The Registration of Births and Deaths (Amendment) Act, 2023, made the birth certificate the sole official document for proof of date and place of birth. The amendment also mandated the digitization of CRS records and integration with national databases such as Aadhaar, electoral rolls, and the population register. As of 2025 The registration level of births for the country has gone up to 92.7% in 2024 from 82.4% in 2011, and the registration level of deaths during 2024 has increased to 92.0% from 66.4% in 2011. The goal of 100% universal registration remains unmet [5].
Figure 1:Key features of SRS.

In 1964-65, the Office of the Registrar General of India initiated sample registration schemes in a few rural areas to test methodologies for collecting reliable birth and death statistics, which got established in 1969-70 on a full scale, covering rural areas of all states & union territories, almost coterminous with this author’s joining Rural health Services in India from 9 July 1968. By 1970s, SRS expanded to urban samples, creating a truly representative nationwide system [1] (Figure 1). The cornerstone of the Sample Registration System’s reliability lies in its innovative dual recording approach. This methodology combines two independent data collection streams to capture vital events with greater accuracy. The first component of the dual reporting system involves continuous enumeration by a resident part-time enumerator, typically a local teacher or health worker who maintains a record of all births and deaths occurring within their assigned sample unit through regular household visits. When a birth or death occurs, the enumerator records details in a prescribed form, capturing demographic information, circumstances of birth/death, and other relevant details year-round, providing an ongoing record of vital events as they occur. The second component involves independent surveys conducted by supervisors who visit each household in the sample units twice a year and independently collect information on births & deaths that occurred during the preceding six months, using a separate set of forms after an interview household member. Crucially, the supervisors collect this information without reference to the continuous records maintained by local enumerators.
The power of the dual reporting system emerges in the reconciliation process. The births and deaths recorded through continuous enumeration are matched against those recorded in the half-yearly surveys. For events that appear in only one of the two sources, a field verification is conducted to determine whether the event occurred. This dual-record method effectively addresses the common problem of event omission in demographic data collection and produces a final, reconciled list of events that forms the basis for calculating vital rates [3]. A major strength of the SRS is its ability to provide disaggregated data across following dimensions i) Geographic disaggregation: Data is available at national, state, and rural/urban levels ii) Gender-specific indicators: Many metrics are calculated separately for males and females iii) Age-specific rates: Fertility and mortality data is broken down by age groups, allowing for more nuanced demographic analysis.
Publication and dissemination
The Office of the RGI shares SRS findings through i) SRS Bulletins-released bi-annually with key indicators and preliminary estimates ii) SRS Statistical Reports, the one being discussed in this article is a comprehensive annual publication containing detailed tables & analysis iii) Special reports cover focused analyses on specific demographic issues such as maternal mortality or fertility transitions.
Limitation of SRS Data: The major concern, even in 2025, is despite digital development and computing technologies, analysis and reports take nearly 18 months.
Key take aways from 2023 SRS statistical report: In this article the author analyses only key indicators of CBR, CDR and IMR.
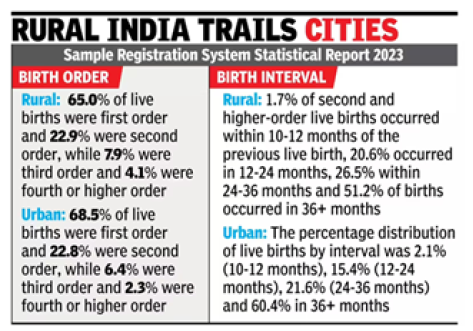
Crude birth rate: The national crude birth rate was 18.4/1000 in 2023. India has an estimated population of 1,463,865,525 people in mid-year 2025. Applying the BR of 2025 (16.55/1000) we expect around 24.2 million births in 2025. The Rural and Urban Difference points to a higher birth rate of 20.3, about 36% higher compared to urban India of 14.9 for the same period. The birth interval is critical information on spacing of children and level of fertility (Figure 2). They are also important factors for the wellbeing of a mother and her children. The data for 2023 showed that 66% (64%) of current live births were first-order births, 22.9% (23%) secondorder births, 7.5% (8.3%) third-order births and 3.6% (4.7%) fourth or higher-order births. This spacing data is encouraging as research or studies like NFHS % (2019-21) had drawn attention to the urgent need for spacing methods to improve health outcomes and highlighted that Inter-Pregnancy Intervals (IPI) shorter than 12 months are a risk factor for stunting and underweight among under-5 children in India (Figure 3).
Figure 2:Key features of SRS.
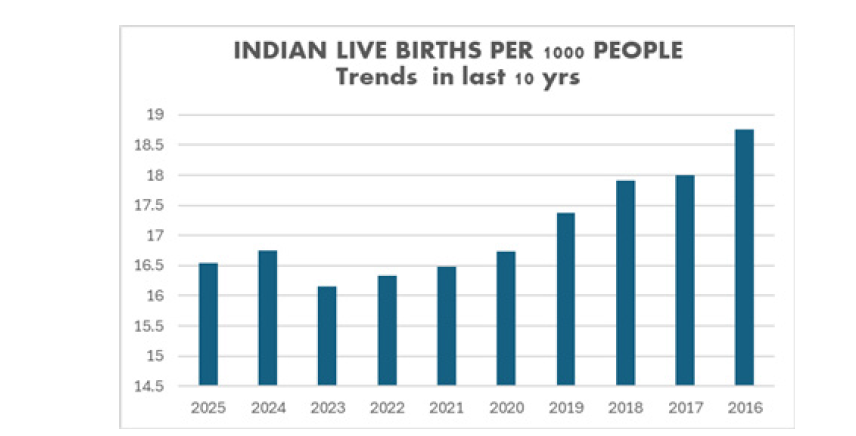
Figure 3:Rural India trails cities.
India birth rate for 2025 is estimated around 16.55, a 1.19% decline from 2024. For 2024 it was 16.75, for 2023 it was 16.15, for 2022 was 16.34, and 16.24 for 2021. Inter-sate variations point that Top 5 States/UTs that the birth rate of Bihar stood at 25/1000 the highest among all States/Union Territories (UTs); followed by Uttar Pradesh (UP) (23.6), Rajasthan (22.9), Madhya Pradesh (MP) (22.5) and Chhattisgarh (22.3), a higher rate by 40- 21.2 % compared national average. In contrast 5 Bottom 5 States/UTs like- Andaman & Nicobar Islands registered the lowest birth rate 10.1, followed by Tamil Nadu (TN) (12.0), Kerala (12.3); Punjab (13.8) and Maharashtra/West Bengal (WB) (14.0) each, a 45.1% to 23.1% lower than national average. In contrast Chandigarh registered lowest birth rate in 2023 i.e. at 4.0. It is followed by Delhi/Manipur (4.5) each, and Jammu & Kashmir (J&K) (5.6).
Figure 3a:Clustered column of CDR trends in last decade in India.
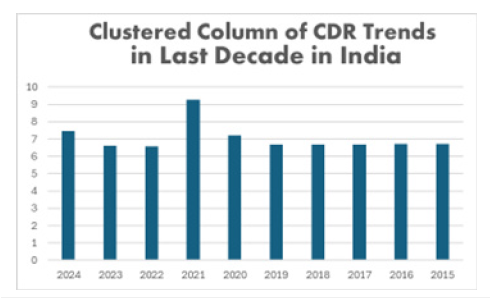
Crude death rate: National CDR was 6.4/1000 population, based on this at least 9.7 million deaths are expected in 2025. Of the people dying this year, 5,281,348 will be male and 4,435,799 females. This amounts to 13,356,121 fewer deaths than births or an addition to the population in 2025. India’s upward trend in deaths is set to increase even further in the future. At national level, men recorded a higher death rate (7.2) compared to women (5.7) both in rural and urban areas of the country. The report showed that rural and urban regions of the country registered death rates at 6.8 and 5.7, respectively reflecting the paucity of healthcare in Rural India. While Chhattisgarh had the highest death rate at 8.3 followed by Odisha (7.7), Kerala (7.2), Punjab (7.3) Andhra Pradesh (AP) (6.9) and Karnataka (6.8). On the other hand, among all States/UTs, Chandigarh registered lowest death rate of 4.0. followed by Delhi/ Manipur (4.5) each, &Jammu & Kashmir (J&K) (5.6). in 2023 [1.8] (Figure 3a).
Overall non-communicable diseases are the leading causes of deaths in the country, constituting 56.7% of all deaths followed by Communicable, maternal, perinatal and nutritional conditions which constitute another 23.4% of deaths. Proportion of male deaths in total deaths was higher for non-communicable diseases and injuries whereas for symptoms, signs and ill-defined conditions and Communicable, maternal, perinatal and nutritional conditions, proportion of female deaths was higher than male deaths. The deaths due to Symptoms, signs and ill-defined conditions were higher in female (13.4%) than male (8.5%) [6-8]. Most deaths in year 2021-2023 occurred in old age (70+ years). Rate of mortality was increasing with age. The contribution of female deaths (4.6%) in infants is higher than male deaths (4.3%), and the deaths of females in age group 1-4 years (0.4%) are like male deaths (0.4%). In age group 5-14 and 70+: Share of female deaths is more than male deaths. While 1-4-year-olds deaths were around 0.4%, in both genders followed by 5-14 yrs (M=0.9%, F=1%) and 30-34 yrs old contributed 2.6% (M=3.2% F=1.7%) deaths. For other age groups, the share of male deaths is more than female deaths (Figure 3b).
Figure 3b:Clustered column of CDR trends in last decade in India.

Infant mortality rate
The Infant Mortality Rate (IMR), which is widely accepted as a crude indicator of the overall health scenario of a country or a region. It is defined as the infant deaths (less than one year) per thousand live births in each time and for a given region. The present level of IMR (25 infant deaths/1000 live births, for the year 2023 is less than one-fifth as compared to 1971 (129 infant deaths per 1000 live births). Despite the decline in IMR over the last decades, one in every 40 infants die within first year of their life in the country. In the last ten years, IMR has witnessed a decline of about 37.5%. While IMR at all India level has declined from 40 to 25 in the last decade, with corresponding decline in rural areas from 44 to 28, and for urban areas from 27 to 18, exhibiting about 36% and 33% decadal decline respectively (Figure 4).
Figure 4:Clustered column of CDR trends in last decade in India.

IMR provides crucial insights into maternal health, socioeconomic conditions, and healthcare accessibility. Neonatal versus postneonatal mortality is the key component of IMR. Changing patterns in infant mortality reflect on factors influencing infant mortality rates, maternal factors, healthcare factors, socioeconomic factors, geographic and environmental factors & a country’s strategies for reducing infant mortality rates, strengthening maternal healthcare, expanding immunization coverage, improving Water, Sanitation, And Hygiene (WASH), strengthening healthcare systems and addressing social determinants like traitorous, beliefs and practices.
The neonatal period is further divided into 1) Early neonatal period: First week of life (days 0-6), when the risk of death is highest 2) Late neonatal period: Second, third, and fourth weeks of life (days 7-28). Primary causes of neonatal deaths include- Preterm birth complications like respiratory distress syndrome, intraventricular hemorrhage, and necrotizing enterocolitis, Birth asphyxia and trauma, Oxygen deprivation during birth leading to brain damage, Congenital anomalies: Structural or functional abnormalities present at birth, Neonatal infections: Including sepsis, pneumonia, tetanus, and meningitis, Low birth weight: Often associated with maternal malnutrition and inadequate prenatal care. Neonatal mortality is closely linked to maternal health conditions, quality of prenatal care, and the availability of skilled birth attendants. Improvements in obstetric care and neonatal intensive care units have significantly reduced neonatal mortality rates in developed countries.
Post-neonatal mortality encompasses deaths occurring between 29 days and one year of age. Primary causes of post-neonatal deaths include Infectious diseases like Pneumonia, diarrheal diseases, malaria, and measles, Sudden Infant Death Syndrome (SIDS) Unexplained death during sleep, Accidents and injuries including suffocation, drowning, and falls, Malnutrition, often compounding other health issues, Long-term complications of preterm birth or congenital anomalies. Post-neonatal mortality is more strongly associated with environmental factors, socioeconomic conditions, and parental education. Improving living conditions, nutrition, immunization coverage, and access to primary healthcare services effectively reduces post-neonatal deaths.
ICD 11 implementation in India
The International Classification of Diseases (ICD) serves as the global standard for categorizing health conditions, diseases, and causes of death. Despite its significance, India faces unique challenges in implementing ICD across its vast and diverse healthcare landscape, from sophisticated urban hospitals to resource-constrained rural facilities. Currently, Tertiary care centers like major medical institutions and teaching hospitals have robust ICD implementation, often integrated with Electronic Medical Records (EMRs). Secondary care facilities like District hospitals show moderate adoption, but majority have inconsistent application. Most Primary health center have limited implementation, with many still using simplified classification systems or basic diagnosis recording. In private sector corporate hospital chains have sophisticated systems while smaller private facilities often have poor recording systems. Most importantly even the available data is hardly analyzed and put into action.
The net outcome is our morbidity data is only about outbreaks
through IDSP. An WHO Expert Committee identified the following
requirements to be satisfied by the health information systems:
1) The system should be population-based.
2) The system should avoid the unnecessary agglomeration
of data.
3) The system should be problem-oriented.
4) The system should employ functional and operational
terms.
5) The system should express information briefly and
imaginatively.
6) The system should make provision for the feedback of
data.
Conclusion
The National Ayushman Bharat Digital Mission (ABDM) with components like Ayushman Bharat Health Account Number (ABHAN), Health Facility Registry (HFR), Healthcare Professionals Registry (HCPR), United Health Interface (UHI), National Health Claims Exchange (NHCE) and ABHA App, will have hassle-free method of accessing and sharing individual health records digitally. It aims to digitize health records and streamline service delivery to develop the backbone necessary to support the integrated digital health infrastructure of the country. It will bridge the existing gap between the different stakeholders of healthcare ecosystem through digital highways. It is expected to enable NHM interaction with participating healthcare providers, and allows NHM to receive digital lab reports, prescriptions and diagnosis seamlessly from verified healthcare professionals and health service providers. Data from the ABDM dashboard reveals notable progress in beneficiary registration. As of 1 October 2025 81,76,89,418 ABH Accounts have been created and 74,31,79,440 health records linkage achieved. Registrations of over 4,28,486 health facilities and 7,12,882 health care professionals have been verified by ABDM. Inter-state variation in progress is significant, particularly in health facilities and health professional registration and useful data is yet to be made available [2].
The next step is digitizing unstructured clinical data and creating longitudinal health records. Digital enablement across providers on a common infrastructure is the critical first step, requiring joint effort from technology companies & healthcare providers. If healthcare is the car of the future, data is the fuel, foundation models are the engine, still need steering & navigation. Data, particularly longitudinal and multimodal, acts as fuel, while foundation including multimodal AI systems that integrate lab results, treatment charts, and ICU signals - serve as the engine. Steering ensures clinical safety through human oversight, while navigation describes new AI systems that sequence and execute tasks responsibly [4]. Developing a foundation model, including multimodal AI systems to integrate service reports, lab results, treatment charts, and ICU signals to serve as the engine. Steering ensures clinical safety through human oversight, while navigation describes new AI systems that sequence and execute tasks responsibly are critical to achieve universal healthcare access & innovation. India may not be as data rich as it should be for its size, but its healthcare odyssey will be defined not by the amount we generate but by how effectively that data is cleaned, curated, & used.
References
- (2023) SRS-Statistical Report, India.
- (2020) National Digital Health Mission (NDHM)_Strategy Overview.
- SRS-estimating-birth-death-rates-India.
- Suresh K (2019) Can-india-achieve-universal-healthcare-by-2030? Journal of Quality in Health Care & Economics 2(2): 000119.
- Global metrics/India/birth-rate. Macro Trends.
- 2023-saw-66-first borns-birth-gap-improved.
- (2025) India’s birth & death rates drop by half over 50 years.
- (2021) Causes of Death-Statistics. RGI &Census Commissioner of India.
© 2026 Suresh Kishanrao. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






