- Submissions

Full Text
Novel Research in Sciences
Robotic Resection of a Retroperitoneal Ganglioneuroma
Marina Gabrielle Epstein1, Franco Milan Sapuppo2, Luis Roberto Manzione Nadal1, Gabriel Maccapani1, Marília Fernandes1 and Vladimir Schraibman1*
1General Gastric and Minimally Invasive Surgery, Brazil
2General Surgery Resident, Brazil
*Corresponding author:Vladimir Schraibman, General Gastric and Minimally Invasive Surgery, Brazil
Submission: April 16, 2021;Published: April 29, 2021
.jpg)
Volume7 Issue3April, 2021
Abstract
Ganglioneuromas (GN) belong to a group of neuroblastics tumors originated from the neural crest and are constituted by mature ganglion cells and Schwann cells. In most cases they are asymptomatic and when they trigger symptoms, they are due to the mass effect. The diagnosis is suggested by complementary imaging methods but needs histological confirmation.
Introduction
GN belong to the group of neuroblastic tumors, which originate from the neural crest and are composed of mature ganglion cells and Schwann cells. Most are asymptomatic and found accidentally. The treatment of retroperitoneal mass is complete surgical excision. In the literature, the number of retroperitoneal masses reported is quite limited. Careful dissection and preservation of these structures is capital, especially in case of benign retroperitoneal masses. We report a case of robotic excision of a retroperitoneal ganglioneuroma.
Case Report
Figure 1:MRI.
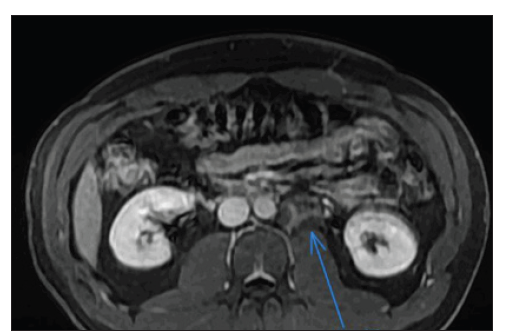
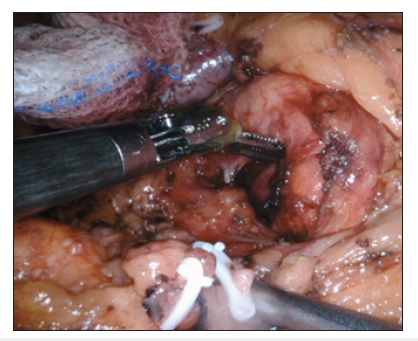
A 32-year-old male patient without comorbidities presented with sporadic abdominal pain. He had not undergone abdominal ultrasound due to SARS-COV-2 pandemic. In November he felt symptoms compatible with COVID-19, latter on confirmed with a PCR test. Patient underwent chest tomography and was found incidentally a retroperitoneal mass, left paraaortic, at the level of the renal hilum on this side, with approximately 3.4cm, appearing to contain internal fatty areas, partially included here. It was necessary to proceed with diagnostic investigation, preferably through MRI of the upper abdomen for further elucidation. In view of the findings, he performed an abdominal MRI scan (Figure 1) that identified: expansive heterogeneous and lobulated retroperitoneum para-aortic lesion on the left, just below the renal vessels on this side, measuring 5x5x3.5x3.2cm. It presented heterogeneous hypersignal in T2-weighted sequences, discreet and late enhancement and spots of micro and macroscopic fatty content. There was little insinuation of the lesion in the left anterior pre-vertebral space (level L1 / L2), without compromising the intervertebral foramen or adjacent organs. The possibility of injury to the mesenchymal lineage (mainly a liposarcoma) should be considered, admitting differential with injury of neural or paraganglionic origin. Computed tomography-guided lesion biopsy of the lesion suggested neuroblastic neoplasia with ganglioneuroma characteristics [1,2]. Due to the findings, the patient underwent retroperitoneal tumor resection and robotic retroperitoneal lymphadenectomy with the Da Vinci XI robot. Patient was positioned in a left flank position and five ports were introduced transperitoneally. Intraoperative ultrasound was performed for the precise identification of the lesion and cautious tumor dissection and resection was performed, which had minimal contact with the left renal vein (Figure 2). The procedure took about 150 minutes, with an estimated loss of 80mL of blood and the patient was discharged on the 3rd postoperative day. The anatomopathological examination revealed a maturing ganglioneuroma a peripheral neural sheath neoplasm consisting mainly of a schwannomatous component and mature and in-between maturation ganglion cells. Classification INPC (International Neuroblastoma Pathology Classification) - favorable histology [3,4].
Figure 2:Intra-operative image of the retroperitoneal mass.
Discussion
The reported incidence of GN is one per million in population. As a primary retroperitoneal tumor, it constitutes only a small percentage of 0.72% to 1.6%. The common sites of origin are retroperitoneal (32% to 52%), mediastinal (39% to 43%), or cervical (8% to 9%) region. Although ganglioneuromas usually develop in childhood, they are often detected in adults because they grow slowly. Two-thirds of patients are under the age of 20 years and ganglioneuromas are rarely observed over the age of 60 years. Most common sites of presentation are the posterior mediastinum, retroperitoneum, head and neck region. GN are usually asymptomatic found incidentally on abdominal imaging or having nonspecific symptoms related to mass effect and compression of surrounding organs. In rare cases, GN secretes sufficient quantities of vanillyl mandelic acid or homovanillic acid to manifest with flushing and other symptoms of catecholamine excess. Neuroblastoma and GN represent tumors of neural crest origin with a continuous spectrum of neuronal maturation. GN is composed of ganglion cells and mature Schwann cells (mature stroma). Cellular atypia, mitotic activity, and necrosis are not featuring of GN. GN averages 8cm in diameter and may appear encapsulated, although a true capsule is infrequent. The tumors are firm, white to yellow in color, and may appear trabeculated or whorled. The definitive diagnosis is made on histopathology. In our case, a CT scan guided biopsy was done prior to going in for surgical resection to confirm the diagnosis.
The treatment of retroperitoneal mass is complete surgical excision, which can become a limitation factor for complete excision of a tumor surrounding vital organs and blood vessels.
Conclusion
The application of robotic surgery for complete and safe resection of a rare retroperitoneal tumor such as GN is an acceptable approach with less sustained blood loss and shorter hospital stay.
References
- Geoerger B, Hero B, Harms D, Grebe J, Scheidhauer K, et al. (2001) Metabolic activity and clinical features of primary ganglioneuromas. Cancer 91(10): 1905-1913.
- Singh J, Priyadarshi VK, Pandey PK, Vijay MK, Pal DK (2013) Retroperitoneal ganglioneuroma. APSP J Case Rep 4: 8.
- Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, et al. (2018) The SCARE 2018 statement: updating consensus Surgical Case Report (SCARE) guidelines. Int J Surg 60: 132-136.
- Sneha P, Akther MJ, Satyam G, Sumanth M (2015) Retroperitoneal ganglioneuroma, a rare cause of abdominal pain. Saudi Surg J 3: 20-22.
© 2021 Vladimir Schraibman. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.








.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)







