- Submissions

Full Text
Novel Approaches in Cancer Study
Neuroblastom of the Bone Marrow in Young Adult Male Without Identifiable Primary
Basil Kadhim Abdullah1*, Zainab Basil Kadhim2, Ghada Basil Kadhim3 and Zena Jameeel Ahmed4
1Consultant subspecialty pediatric heamato-oncology, Iraq
2Medical student, School of medicine, Iraq
3Sixth stage student, freshta secondary School, Iraq
4Jwahery primary school, Iraq
*Corresponding author: Basil Kadhim Abdullah, Consultant subspecialty pediatric heamato-oncology, Sulemania, Iraq
Submission: October 22, 2020Published: December 15, 2020

ISSN:2637-773XVolume5 Issue4
Abstract
Neuroblastoma is the most common malignancy in infancy and the third most common cancer in pediatric, following the acute leukemia and central nervous system tumor, constituting approximately 7-10% of pediatric malignancy. The majority of the patients (approximately 90%) diagnosed before the age of 5 years, with peak incidence at the age of two years. However, the incidence of neuroblastoma decreasing with age and less than 5% from all cases diagnosed after the age of 10 years, its occurrence is rare during adulthood (one per 10 million cancer diagnoses per year). In addition, neuroblastoma is very rarely presented with Bone marrow involvement without identifiable primary site. We reported a young adult male patient with advanced neuroblastoma at the age of 21 with solely Bone marrow involvement without radiological identifiable primary tumor site who was died before starting him on chemotherapy treatment because of severe febrile neutropenia.
Keywords: Neuroblastoma; Young adult; Bone marrow involvement; Primary tumor; MYCN amplification
Abbreviations: g: gram; dl: deciliter; ml: milliliter; PT: Prothrobine Time; PTT: Partial Thromboblastine; CD: Cluster of Differentiation; CT: Computerized Tomography; mg: milligram; VMA: Vanillyl Mandelic Acid; HVA: Homo Vanillic Acid (HVA)
Introduction
Neuroblastoma arises from primitive sympathetic neural cells primarily in the adrenal medulla and also in the paraspinal sympathetic ganglia in the neck, chest, abdomen, or pelvis [1]. Although neuroblastoma currently represents 7% of all childhood malignancies or roughly 1 case per 100,000 children per year, only 1 case per 10 million adults per year is diagnosed in adulthood [2-4]. Because of the rarity of adult neuroblastoma, staging systems and risk assessment tools have been developed using primarily pediatric data [5]. Clinically relevant pediatric factors that influence survival in children include stage, age, histology, tumor grade, MYCN oncogene status, chromosome 11q status, and DNA ploidy. These factors are currently part of the international neuroblastoma risk assessment system [6]. Because of the rarity of this tumor in adult patients (over 20 years old) We reported an adult male patient pancytopenia who was diagnosed as a bone marrow involved MYCN positive neuroblastoma without any radiological evident primary tumor site who was unfortunately died before directed antitumor therapy because of the rapid progressive course of febrile neutropenia.
Case Report
A 21-year-old young adult male was referred to the hematology department because of pancytopenia for assessment and treatment. The patient was well until he suddenly developed intermittent fever and anorexia for the last 5 weeks which was temporarily responding to antipyretic, he received several courses of antibiotic treatment without any objective response, the fever was neither associated with rigor nor sweeting. He was fully vaccinated with no consanguinity of parents. Medical and surgical histories were uneventful, family history was negative with no similar condition. On examination,
he was febrile, ill looking, pallor, ecchymosis on both legs, neither
hepatomegaly nor lymphadenopathy. Laboratory investigations
reveal pancytopenia in complete blood picture with Hemoglobin
value of 8.4g/dl, the platelet count was 19,000/ml, and a leukocyte
count of 2,300/ml with 54 % neutrophils, 45% lymphocytes, 1%
monocytes, 0.5% basophils and 0% eosinophil, Blood film reveals
normochromic normocytic anemia with neither immature nor
abnormal cell, erythrocyte sedimentation rate 97mm in 1h.
Other laboratory investigations including liver function tests,
renal function tests, serum electrolytes (potassium, sodium, calcium,
phosphorus); serum uric acid and coagulation profile (PT and PTT),
all were normal. Bone marrow aspirate (BMA) morphologically
revealed that normal hemopoietic cells were almost entirely
(more than 90%) replaced with small blue round neoplastic cells.
These were mainly cells with a high nucleocytoplasmic ratio and
moderately basophilic cytoplasm; tumor cells appear arranged in
a rosette (Figure 1A & 1B).Bone marrow trephine biopsy (BMB)
confirmed the diagnoses of poorly differentiated neuroblastoma
by morphology that showed infiltration with non-hematological
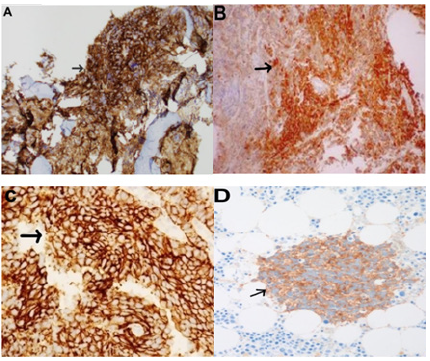
malignant small round cell (Figure 2), and immunohistochemistry
revealed positive staining for synaptophysin, Neuron Specific
Enolase (NSE), CD56, and neuronal marker PGP9.5 (Figure 3). Real
time polymers chain reaction (PCR) analysis for the tumor cells was
positive. Radiological evaluations including abdominal ultrasound,
chest x-ray, C.T. scan of chest and abdomen all were normal and failed
to find an apparent primary site. 24 hours urine vanillylmandelic
acid (VMA) was elevated with a value of 53mg/24 hours (normally
less than 9mg/24 hours); 24 hours urine homovanillic Acid
(HVA) was also elevated with a value of 61mg/day (normal level
of less than 15mg/day). Based on the bone marrow morphology,
immunohistochemistry staining and elevated 24 hours urine for
both VMA a HVA the diagnosis of stage IV neuroblastoma was
confirmed. The patient clinical condition was critical because of
febrile neutropenia and blood culture was positive for pseudomonas
aeruginosa which was sensitive to meropenem, he deteriorated
rapidly and unfortunately died because of severe sepsis before
starting chemotherapy or other-directed therapy for his underlying
malignancy. His critical, rapidly deteriorated clinical condition did
not allow us to do neither Positron emission tomography (PET),
metaiodobenzylguanidine (MIBG) nor Bone scan.
Figure 1:BMA shows normal hemopoietic cells replaced by small blue round neoplastic cells; tumor cells appear
arranged in a rosette (black arrow) by Giemsa Stain.
A. (original magnification 200X) and B. (original magnification 1000X).
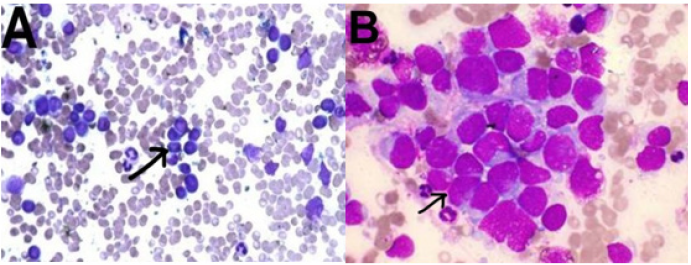
Figure 2:Bone marrow trephine biopsy shows infiltration with non-hematological small round cells malignancy
(black arrow).
A. (H&E, X100) and B.(H&E, X400).
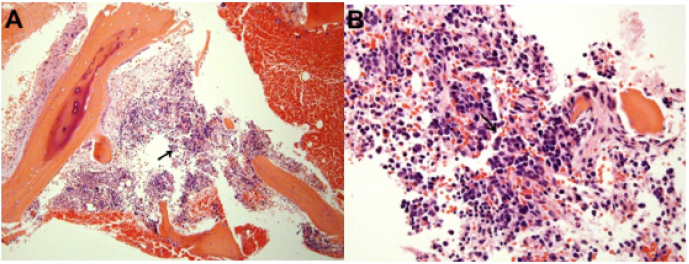
Figure 3:Bone marrow trephine biopsy immunohistochimestry reveals positive staining (black arrow) for
synaptophysin.
A. Neuron Specific Enolase (NSE)
B. CD56
C. and pgp9.5
D. (original magnification 200X).
Discussion
Neuroblastoma is the most commonly occurring extracranial
solid tumor diagnosed in the pediatric population [7]. Ninety
percent of diagnoses occur in patients less than 4 years of age [8,9].
Furthermore, outcomes in adults are significantly worse than those
in children. However, this diagnosis is extremely rare in adults, with
less than 100 cases reported in the literature; moreover, adults with
metastatic neuroblastoma typically have a very poor prognosis [10].
Disease presentation is often similar in adults and children, though
several differences have been described. Disease progression is
often more indolent in adults compared with children. A significant
minority has a slowly progressive disease or recurrent relapses
over a period of years. Tumors are of the sympathetic nerve chain
and thus locations of primary tumors occur similarly in adults and
children [11]. Notably, MYCN amplification is common in the highrisk
pediatric population but appears very rarely in adults [12]. We
reported this adult male with neuroblastoma for two reasons; first
because of the rarity of neuroblatoma in adult (defined as older
than 20 years) with less than 100 cases reported in the literature)
[10]; and second because of this disease occasionally presented
with solely bone marrow infiltration without identifiable primary
site, in a series of 25 adult/adolescent patients, 16% had disease
occurring in the pelvis, while 68% arose in the retroperitoneum or
adrenal glands [12].
Our case report, we presented 21 years old young adult male
presented with fever and pancytopenia, no hepatosplenomegaly,
neither lymphadenopathy nor palpable mass, complete blood
picture and blood film showed anemia, thrombocytopenia and
neutropenia without any abnormal immature cells. BMA showed
infiltration by malignant small blue round cells which replaced
almost all hemopoietic components, immunohistochemical staining
of the bone marrow trephine biopsy together with elevated tumor
marker (24-hour urine VMA and HVA) confirmed the diagnosis of
neuroblastoma which is categorized according to the international
neuroblastoma staging system (INSS) as stage 4 (due to the bone
marrow involvement).
Radiological evaluation by abdominal ultrasound, chest x-ray,
CT scan of chest and abdomen; all failed to identify an apparent
primary site. Unfortunately, the patient died because of severe sepsis
due to febrile neutropenia before further radiological assessments
by Positron emission tomography (PET), metaiodobenzylguanidine
(MIBG) and Bone scan.
Conclusion
This case represents the presentation of a common disease in an uncommon patient population with uncommon presenting scenario. Due to the rarity of the neuroblastoma in adult and due to the fact that pancytopenia without primary mass; The majority of adult hematologists and oncologists will not put neuroblastoma in the differential diagnosis of neuroblastoma in an adult patient with pancytopenia; however, this diagnosis should at least be considered in certain cases. Neuroblastoma should be considered particularly in patients of adolescent age and possible cause of pancytopenia even in adults. Furthermore, due to the rarity of these diseases, diagnostic evaluation by an experienced pathologist is warranted to distinguish between neuroendocrine tumors and the rare case of adult neuroblastoma. Due to the rapidly progressive course of our patient and due to the MYCN amplification in our patient; we also concluded that neuroblastoma in adult patients is possible to behave more aggressive in adult patients than in pediatric patients.
Consent
Written informed consent was obtained from patient’s parent for this case report.
Acknowledgment
We gratefully acknowledge both patient and his family for allowing us to publish their case report.
Authors’ Contributions
Consultant Dr. Basil Kadhim Abdallah Al odda has been involved in clinical diagnostic evaluations and management.
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethical Consideration
Ethical approval for this case report was obtained from NCI ethical committee. Because of the retrospective nature of this case report, the ethical committee waived the requirement of informed consent.
References
- Brodeur GM (2003) Neuroblastoma: Biological insights into a clinical enigma. Nature Reviews Cancer 3(3): 203-216.
- Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA: A Cancer Journal for Clinicians 62(1): 10-29.
- Hsieh MH, Meng MV, Walsh TJ, Matthay KK, Baskin LS (2009) Increasing incidence of neuroblastoma and potentially higher associated mortality of children from nonmetropolitan areas: Analysis of the surveillance, epidemiology, and end results database. Journal of Pediatric Hematology/Oncology 31(12): 942-946.
- Esiashvili N, Goodman M, Ward K, Marcus RB, Johnstone PA (2007) Neuroblastoma in adults: Incidence and survival analysis based on SEER data. Pediatric Blood and Cancer 49(1): 41-46.
- Monclair T, Brodeur GM, Ambros PF, Brisse HJ, Giovanni, et al. (2009) The international neuroblastoma risk group (INRG) staging system: An INRG task force report. Journal of Clinical Oncology 27(2): 298-303.
- Cohn SL, Pearson AD, London WB, Tom M, Ambors PF, et al. (2009) The international neuroblastoma risk group (INRG) classification system: An INRG task force report. Journal of Clinical Oncology 27(2): 289-297.
- Castleberry RP (1997) Neuroblastoma. European Journal of Cancer 33(9): 1430-1437.
- Maris JM (2010) Recent advances in neuroblastoma. The New England Journal of Medicine 362(23): 2202-2211.
- Hiyama E, Iehara T, Sugimoto T, Masahiro F, Yutaka H, et al. (2008) Effectiveness of screening for neuroblastoma at 6 months of age: A retrospective population-based cohort study. The Lancet 371(9619): 1173-1180.
- Franks M, Bollen A, Seeger RC, Stram DO, Matthay KK (1997) Neuroblastoma in adults and adolescents: An indolent course with poor survival. Cancer 79(10): 2028-2035.
- Kaye JA, Warhol MJ, Kretschmar C, Landsberg L, Frei III E (1986) Neuroblastoma in adults. Three case reports and a review of the literature. Cancer 58(5): 1149-1157.
- Kushner BH, Kramer K, LaQuaglia MP, Modak S, Cheung KV (2003) Neuroblastoma in adolescents and adults: The Memorial Sloan-Kettering experience. Medical and Pediatric Oncology 41(6): 508-515.
© 2020. Basil Kadhim Abdullah. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






