- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Biological Mystery and Public Health Implication of Twin Pregnancy and Delivery
Suresh Kishanrao*
Family Physician & Public Health Consultant, India
*Corresponding author:Suresh Kishanrao, Family Physician & Public Health Consultant, Bengaluru, India
Submission:October 21, 2025;Published: November 13, 2025

ISSN: 2577-2015 Volume5 Issue3
Abstract
Introduction: Twin births have always fascinated doctors, scientists and society, from their biological mystery to their public health implications. While carrying twins is exciting, demands extra care, a lot to learn, cope up and prepare for delivering, 4-6 weeks in advance of normal 40 weeks. Over the past few decades, the world has seen a quiet & significant rise in twin births. Most of this increase comes from fraternal twins, which are shaped by maternal age and medical interventions and not from identical twins, which remain steady at around 3-4 per 1,000 births. This article is an analysis of two such twin pregnancies in 2025, one from paternal side another from maternal side of the author over the past century. Both were from current couples from paternal side genetic history and with history using oral contraceptives for spacing after the first girls were born and second paras after 6-8 years. Author hypothesizing that first few cycles after stopping oral contraceptive pills is an additional risk for twin pregnancies “The frequency of multiple births has increased by about 33% since the 1980s, largely due to assisted reproductive technologies such as In-Vitro Fertilization (IVF), during which, multiple eggs can be used at the same time to maximize the chances of a successful pregnancy, leading to twin births. Other reasons are i) age at birth >30 years ii) familial trend or genetics and iii) Oral contraceptives known to prevent pregnancy, as there would be a high chance of conceiving twins due to numerous hormonal changes in the body during the first couple of cycle after stopping. The global twin birth rate is about 12-16 per 1,000 live births. The proportion of twin births in India rose from 0.9% in 1993 to 1.5% in 2021. Fraternal twins account for about 70% of all twin pregnancies whereas Identical twins account for 20-25% and multiple pregnancies to rest. Identical twins occur roughly 3 to 4 per 1,000 births worldwide.
Materials & methods: This article is prompted by two twin pregnancies, among nearly 100 couples followed by this author in the last one year supported by literature search.
Outcome: While the first case had age and contraceptive use as trigger factors, delivered in May 2025 and kids doing well. The second case has family history of twins, age and non-ART medicinal treatment for ovulation who is expected to deliver in January 2026.
Keywords:Twins; Dizygotic twins; Fraternal twins; Identical twins, Monozygotic twins; Chorionicity; Amnion city; Anemia; Blood transfusions; Pre-term delivery; Congenital anomalies
Abbreviations: LMP: Last Menstrual Period; TBR: Twin Birth Rate; IUGR: Intrauterine Growth Retardation; HDP: Hypertensive Disorders of Pregnancy; PPH: Post-Partum Hemorrhage; LBW: Low Birth Weight
Introduction
A twin pregnancy is a condition where a woman has two babies at the same time. Twin births have always fascinated doctors, scientists and society, from their biological mystery to their public health implications. While carrying twins is exciting but it demands extra care, as woman’s body is working double-time and makes the couple thrilled and wife nervous. She needs to learn, to cope and prepare for delivering,4-6 weeks in advance of normal gestation [1]. The global Twin Birth Rate (TBR) is about 12-16 per 1,000 live births. Fraternal twins account for about 70% of all twin pregnancies Identical twins occur roughly 3 to 4 per 1,000 births worldwide. Over the past few decades, the world has seen a quiet but significant rise in frequency of multiple births, by about 33% since the 1980s globally, largely due to assisted reproductive technologies. The proportion of twin births in India rose from 0.9% in 1993 to 1.5% in 2021. It is projected that by 2050, most countries would see TBR climb by more than 60% [2]. Twin Pregnancy occurs when two embryos develop in the uterus simultaneously. There are two primary types: identical twins, which are formed because of a splitting fertilized egg, & fraternal twins, where two different ova are fertilized by two different sperm. Identical twins share the same genes and typically resemble each other, whereas fraternal twins are like siblings born at the same time; they may not resemble each other and can be of the same or opposite sex. One of the early signs of a twin pregnancy is feeling unusually tired, more than in a normal single pregnancy. Most women also have worse morning sickness & feel stomachs expanding at a more rapid pace. Laboratory test of blood may detect elevated levels of the hCG hormone.
Entire course of the pregnancy, woman feels heavier & requires more sleep. A woman’s chances of having twins go up due to i) familial trend, ii) women over 30 are more likely to release more than one egg during ovulation, increasing the chance of fraternal twins iii) Fertility treatments like IVF and non-ART fertility treatments lead to a twin pregnancy iv) First few cycles after stopping oral contraceptive pills [3]. Twin pregnancies carry a greater risk of adverse outcomes, especially perinatal mortality and neonatal morbidity. Twin pregnancies increase preterm delivery, low birth weights, congenital anomalies and SNCU admission. Complications include IUGR, HDP, anemia, PPH and blood transfusions. This article is prompted by two such twin pregnancies, in last 4 generations of authors family tree of nearly 100 couples, in 2025. Their experiences, family members excitement, extra care during pregnancy and postnatal period of one of them are captured and compared with what literature search for twin pregnancies & parturition reports.
Case Reports
Case 1
Australian residents: Itidaa a 31-year-old computer engineer by education married to another software engineer working in Australia, had stopped working after the first daughter’s birth. She had used oral contraceptives for about 4 years after the elder daughter. She got pregnant again when the elder daughter was 6 years old and the first scan around 10 weeks confirmed twins-both girls. A DNA test had determined zygosity of same-sex twin pairs as dizygotic [3]. Her paternal grand aunt and uncle were twin about 100 years ago. In India zygosity is known only at the birth by the placentas & fetal membranes. Having known the sex of the fetuses the couple made a well-informed choice to continue the pregnancy. Psychologically she was balanced and gender of the twins didn’t bother the couple. She delivered it to her maternal home by cesarean on 3 November 2024, & this author saw the girls on 8th November 2024 and was able to differentiate who was younger (by few minutes only) by growth. The family, especially two elder married working sisters, took leave around perinatal period for a month and gave solid support. First few weeks, it was a challenge understanding the schedules of newborns which were different continues to be so even now. When one is awake the other is sleeping. One is calm and her existence comes to notice when hungry and the other naughty keeps everybody alert with her shouts and plays. The children’s father gave excellent support working from home for nearly 3 months looking after the first daughter’s requirement of schoolwork etc. and newborns’ born care. The girls are now about 6 months old and doing well. The younger one is better built with lots of hair on scalp whereas the older one has scanty hair. There is a family history of her paternal grandfather and grand aunt being twins (Figure 1).
Figure 1: Example of viewing the original image (first line) in RGB (second line), HSV (third line) and LAB (fourth line).
Case 2
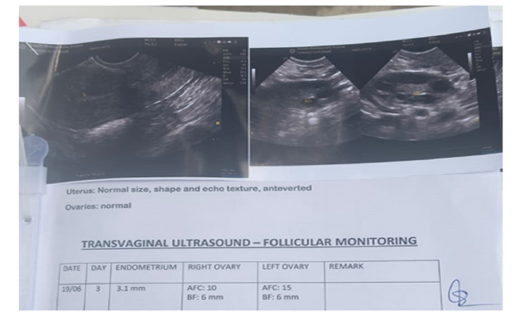
Indian case: Ms. Ivagrahb & Yaniv couple married 9 years
ago had the first daughter after 18 months of marriage. After that
the lady used oral and injectable contraceptives for about 3 years.
Started trying for the second child in 2022, stopping contraceptives.
In the meantime, the husband was diagnosed as diabetic and, in a
year, had erectile deficiency, which not only limited sexual activity
but also increased sexual satisfaction. The lady was investigated
and was put on oral contraceptives for 4 cycles. In May 2025 both
were investigated. Husband had low proportion of normal sperms.
Both were put on non-ART fertility medications and asked to
continue normal sexual activity for next 3 months. A Transvaginal
ultrasound on 19 June 2025 for monitoring follicular phases,
showed endometrial thickness of 3.1mm, Right ovary-AFC10, BF:
6mm and Left Ovary AFC-15mm and BF:6mm. Surprisingly the
lady had her LMP on 18 June 2025. An Obstetric for first trimester
(TVS) scan on 25 July 2025 confirmed the following: This couple
was highly excited for the “double Dhamaka”. Her mother-in-law
had twin pregnancies which didn’t survive. (Table 1) The couple
was highly excited for the “double Dhamaka” outcome initially,
thanking almighty for the gift. Excitement did not last long for the
lady as she got worried about how she would take care of two kids,
which depressed her often and triggered her migraines often. In
late September, she even thought and consulted the author for the
termination of the pregnancy which needed lot of counselling &
even threatening that no medical professional would venture doing
at that stage (Figure 2). Similar depressive symptoms erupted
around 10th October 2025 and counselled again. The Scan report
of 18 October 25:
A. Twin live intrauterine Pregnancy
a. Twin A of GA 17 Wks. & 5 days
b. Twin B of GA 17 Wks. &
B. Liquor adequate in both the twins
Table 1:
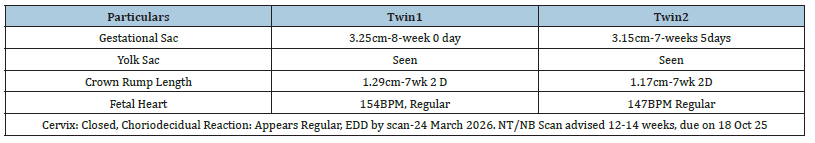
Figure 2:
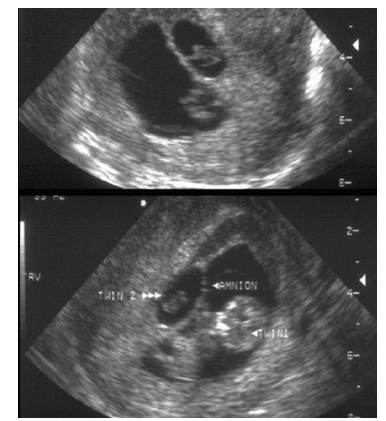
Technical limitation: Limited acoustic window due to thick maternal abdominal wall, suboptimal visualization. Poor acoustic beam penetration even on THI imaging. High frequency sound produces better image resolution but penetration to deeper tissues is limited when using a high frequency transducer (THI). As sound travels through tissue, it will lose energy. Several interactions contribute to this process of attenuation including reflection, scattering and absorption. This results in an exponential decrease in the energy of the pulse, therefore producing weaker echo signals, the deeper it travels into the patient. There is always a compromise between resolution and penetration (Figure 3).
BPD: Biparietal Diameter, HC: Head Circumference, AC: Abdominal Circumference & FL: Femur Length
Figure 3:
Discussion
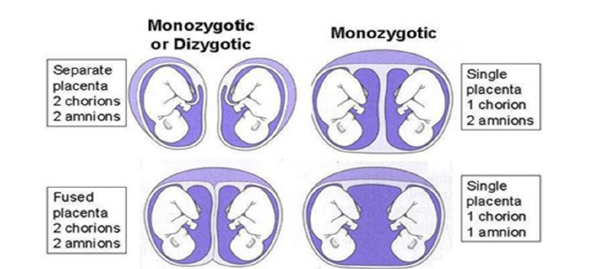
A twin pregnancy is a condition where a woman has two babies at the same time. Twin pregnancies are classified by zygosity, chorionicity (and amniocity), as they have important implications on pregnancy & infant outcome. Zygosity & chorionicity aren’t overlapping concepts. Zygosity refers to the type of conception and the genetic makeup of the twins, while chorionicity refers to the type of placentation [4]. many fertilized eggs (zygotes) they develop from. The twins There are two types of twins by zygosity. Being identical or not depends on the babies’ zygosity, that is how can arise from one (monozygotic) or two fertilized eggs (dizygotic). Chorionicity refers to the number of external membranes that surround the fetus in a multiple pregnancy and corresponding placentation (monochorionic or dichorionic) Amnion city refers to the presence or absence of amniotic membranes between the twin, the number of amniotic sacs (i.e. monoamniotic or diamniotic).
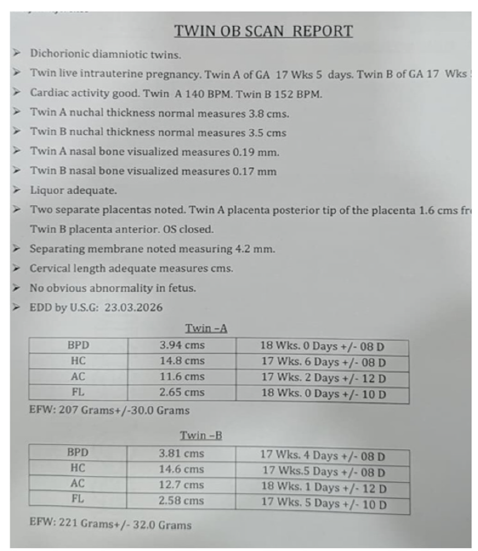
Mono-zygotic twins (MZT or identical twins)
MZT originate from one ovum fertilized by one sperm. However, the fertilized egg (zygote) splits into two, or very rarely three or more) during the early stages of mitosis which results in separate identical multiple embryos. About 30% or 1 in 3 sets of twins are identical. MZ twins share the same DNA and have identical genetic makeup. They are always the same sex and they have the same genetic characteristics, like same skin, hair & eye color. They look very similar. Hereditary factors do not play a role in their development. About one third of all twins are identical. Their rates are constant all over the world: 3-5/1000 births. In MZ twins the type of placenta and number of amniotic sacs depend on the time of division of the zygote. It determines whether MZ twins have a common or separate placenta and whether they will develop in the same or different amniotic sacs. An egg which divides within the first 72 hours (0-3 days) will result in twins who each have their own placenta and own amniotic sac. This accounts for around 20%-30% of identical twins. Division at 4-8 days (around 60%- 70% of identical twins) will typically result in twins sharing a placenta but each with their own amniotic sac. An egg dividing at 9-12 days will result in identical babies that will grow together in a single amniotic sac and share a placenta. Twinning beyond 8 days is rare and represents about 1% of all twins. Twinning occurring beyond 12 days could lead to conjoined twins, where babies share, to varying degrees, parts of their bodies. Conjoined twins are very rare: (1/50,000-1/100,000 live births). Monochorionic twins are always identical, but around 30% of MZ twins have dichorionic (separated or fused) placentas. If there is only one placenta, the pair is monozygotic.
Dizygotic twins
(DZT or fraternal twins) develop from two separate eggs fertilized by two separate sperms. Oocytes may be released from two different follicles (superovulation) or from a single follicle (polyovular follicle) in the same cycle. The two eggs can originate from either one or both ovaries during simultaneous ovulation and are fertilized at almost the same time. Dizygotic twins are as much like as ordinary siblings born as singletons, with everyone inheriting a random half of each parent’s genes. Due to their near simultaneous conception, they share intrauterine development and simultaneous birthing. On average, DZT are approximately half as genetic as one another as monozygotic twins. Hereditary factors may play a role in their development. About two thirds of all twins are non-identical. Rates vary widely and are affected by maternal age, race, nutrition, geographical location and Assisted Reproduction Technique (ART) currently global rates range from 7 to 12/1000births. If a pair is dizygotic, each twin will have its own placenta, outer membrane (chorion) and inner membrane (amnion) (Figure 4). This is the case for one-third of MZ pairs; therefore, the appearance of two placentas and two sets of membranes do not enable a definitive assessment to be made regarding twin type [4,5].
Figure 4:
DNA Prenatal Testing (DNAPNT)
DNAPNT is a genetic test to confirm the relationship between
the fetus and its parents during pregnancy and has been increasingly
gaining attention recently. In United States, the United Kingdom,
Germany and Japan and Australia to determine the zygosity of
same-sex twin pairs [4]. DNA prenatal paternity testing includes
two methods [5]:
Non-Invasive Prenatal Genetic Testing (NIPT): NIPT is a
method of extracting fetal DNA from maternal blood to confirm
parent-child relationships, which has low risk to the mother &
fetus. Since only a blood test is required, the procedure is safe, and
results can be obtained early.
Invasive Prenatal Testing (IPT): IPT testing includes two
main methods:
i. Chorionic Villus Sampling (CVS): Chorionic villi are extracted
from the placenta in early pregnancy for genetic analysis. It is
highly accurate, but there is a small risk of miscarriage.
ii. Amniocentesis: Amniotic fluid is collected in the second
trimester of pregnancy for genetic testing. It can accurately
analyze the fetus’ genetic makeup. It too carries the risk of
miscarriage. Despite the risks, these methods are to detect
genetic disorders that NIPT cannot [5].
Half-identical or polar body twins
If an egg splits before fertilization and two different sperms can create separate embryos. For these ‘half-identical’ or ‘polar body twins’ DNA match would be closer to 75%, as they inherit different genes from their father but share their mother’s. These babies have separate placentas as the egg has already split before fertilization. Half-identical twins would not be as similar as monozygotic twins but share more similarities than dizygotic (fraternal) twins [6].
Multiple twins
Multiple twins are defined as several twins greater than twotriplets, quadruplets, quintuplets, etc. which is common with fertility treatments. During the use of In Vitro Fertilization (IVF)- multiple births primarily result from transfer of more than one embryo during the procedure. Non-ART fertility treatments include oral medications or injections used to boost ovulation among women who do not ovulate or to stimulate the development of multiple eggs among women who have trouble getting pregnant. Many of these treatments also result in multiple births. Although some infertility patients may prefer to have twins, all multiple births, including twin births, have higher risks for both mother and infants [7]. In multiple twins, monozygosity and Di-zygosity can occur in any combination. More discussion on this issue is not required in this article [7].
What All Can Increase the Chances of Twin Pregnancy
i. Family history/genetics: A family history of twins, then there is a high chance that a lady might conceive twins, because of the genetic predisposition. If wife or husband are a twin themselves, then they are more likely to give birth to twin babies. However, it is likely a maternal thing and does not hold any relation to the father’s family history [5].
ii. Height/weight: It might seem shocking, but lady’s height and weight play a decisive role in the conception of twins. According to a study by the American college of obstetrics and gynecology [6], women who have a BMI of 30 or above have a high chance of conceiving twins, especially true only for fraternal (dizygotic) twins. Moreover, it is also reported that taller woman has a high chance to conceive twins.
iii. Maternal age: While it is a known fact that with age the chances of getting pregnant decrease, but few studies have proved that the chances of having twins increases as female age, because, the production of Follicle Stimulating Hormone (FSH), which plays a key role in the release of eggs from ovaries for ovulation, increases. As the number of eggs released increases, the chances of conceiving twins increase [7].
iv. Oral contraceptives: Although oral contraceptives are to prevent pregnancy, there is a high chance that one can conceive twins, because, when the lady stop taking pills, there are numerous hormonal changes that take place in the body during the first couple of cycles.
v. Previous twin pregnancy/already have a set of twins: If a woman already has twins, the chances of getting pregnant with twins the next time is also high. Even if a woman had been pregnant with twins not necessarily ending in live birth before and conceives for the second time, it is more likelihood to conceive twins again.
vi. IVF (in-vitro fertilization): Chances of getting pregnant with twins is high if a woman opts for in-vitro fertilization as in this procedure, ova are fertilized outside the body and then transferred to the uterus. In this procedure the obstetrician introduces more than one ovum to achieve higher success rate, sperms unite & form more zygotes simultaneously.
Assisted reproductive technology has resulted in a progressive rise in the incidence of twin pregnancies, which affect both mother and child in terms of antepartum complications. In a public sector medical college hospital, in Odisha during the period from 2013 to 2015 all mothers having twin pregnancies (with 28 weeks of completed gestation) admitted to the Antenatal (ANC) ward and labor room were studied. Out of a total of 150 cases 98 cases (65.33%) were dichorionic diamniotic, 50 cases (33.33%) were monochorionic diamniotic, and 2 cases (1.33%) were monochorionic and monoamniotic pregnancies. The majority (66%) of twin pregnancies were between 35-38 wks. of gestational age at the onset of labor. It was observed that macerated births, stillbirths and neonatal deaths are higher in mono-chorionic twins as compared to dichorionic twins [8].
Trends in twin pregnancies
The global twin birth rate is about 12-16 per 1,000 live births. Fraternal twins account for about 70% of all twin pregnancies and identical twins occur roughly 3 to 4 per 1,000 births worldwide over decades. Over the past few decades, the world has seen a quiet but significant rise in frequency of multiple births, by 33% since the 1980s globally, which is largely attributed to assisted reproductive technologies. The proportion of twin births in India rose from 0.9% in 1993 to 1.5% in 2021. Most of this increase comes but from fraternal twins, which are shaped by maternal age and medical interventions and not from identical twins, which remained steady for decades. It is projected that by 2050, most countries would see twin birth rates climb by more than 60%, and by 2100, it will be as high as 79% [2,8].
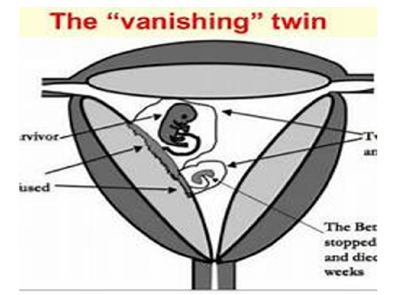
Vanishing twins
Beginning around 1945, doctors realized that some single
births were originally twin pregnancies. One baby was miscarried
during the pregnancy without the mothers or doctors knowing.
Doctors call these cases vanishing twins or vanishing twin
syndrome. It is a type of miscarriage that occurs when one or more
embryos in a multiple pregnancy die or are reabsorbed in the
uterus. A scanning observation demonstrates the fetal surface of
the placenta as an empty and flattened sac, as pathological evidence
of the disappearing twin. One can find a small area containing 30ml
of dark brown blood in the pathological specimen of abortion. The
appearance of a hemorrhagic second sac seen on ultrasonography
may make the patient opt for elective abortion, but if the pregnancy
ends in abortion, the results are that the product of conception is
commonly fragmented. On the contrary, if the pregnancy continues
to full-term, the subsequent sac may have been removed or
expelled, resorbed or fragmented or may persevere as a little atretic
section neglected considerably even after careful examination of
the placenta and the membranes. Some studies report that about
36% of twin or multiple pregnancies experience twin syndrome
vanishing. The vanishing twin may have the following physiological
outcomes [9]:
Resorption: Even though resorption is the most likely
physiologic explanation for the vanishing of the specific proportion
of the gestational sac, the valid incidence of resorption is still
unknown. Resorption is observed from as early as the seventh
week to as late as the twelfth week of gestations. It is evident in any
case that resorption of gestational sacs during pregnancy happens
without affecting the co-twin which has an excellent chance of
survival as resorption mostly occurs in the first trimester (Figure
5).
Figure 5:
Blighted ovum: By definition, a blighted ovum is the gestational sacs inside which no embryo can be visualized via ultrasonography. Most of the pregnancies that end up with the vanishing of a fetus are anembryonic pregnancy co-existing with normal pregnancy. The result could be in the form of vaginal bleeding in the first trimester, indicating the expulsion of the anembryonic sac (Figure 6). It is advisable, therefore, to undergo a thorough ultrasonographic examination before opting for dilation and curettage, as the process of dilation and curettage may end up in the accidental abortion of the other surviving twin.
Figure 6:
Fetus papyraceous: Fetus papyraceous is a mummified, compressed or flattened fetus associated with the other viable fetus. This is very rare and most commonly occurs in multiple gestations. The deceased fetus gets flattened in between the membranes of the other viable fetus and the uterine wall. The demise of the fetus usually occurs right off in the early second trimester. The early demise of the twin may result in complete resorption, but as the pregnancy continues to term, the twin may become macerated and may affect the other viable twin as well, as the pregnancy continues. This course of events is observed via regular ultrasonographic examinations.
Fact small hat may increase the likelihood of vanishing twin syndrome include: i) Advanced maternal age (over 35), ii) Chromosomal abnormalities in the vanished twin iii) Use of assisted reproductive techniques iv) Small placenta or other placental abnormalities v) Genetics and teratogenic factors vi) Increase the incidence of multiple gestations [9].
Antenatal Care Best Practices
Proactive prenatal care is critical for managing twin births &
maternal health include [10,11]:
i. Caloric intake: Twin pregnancies require 300-500 extra
calories daily.
ii. Folic acid supplementation: 1mg/day (vs. 0.4mg for singletons)
reduces neural tube defects.
iii. Iron supplements: Prevent anemia with 30mg/day as being
given to our second case.
iv. Frequent monitoring through biweekly ultrasounds to track
growth discordance and placental health.
v. Cervical length checks to identify preterm labor risks early.
vi. Low-impact activities like swimming or prenatal yoga improve
circulation without overexertion. Avoid high-impact workouts
after 20 weeks.
Psychology and Psychotherapy of Women Pregnant with Twins
Women with twin pregnancies experience significantly higher anxiety levels and a higher rate of severe anxiety, with over 50% scoring in the severe anxiety range as is in our second case. Their mean cognitive function scores are also significantly lower compared to women with singleton pregnancies. However, depression scores were similar between the two groups. These differences in anxiety and cognitive function remained significant after adjusting for maternal age, BMI, use of psychiatric medications, education level, nulliparity, pregnancy complications and multifetal gestation despite increased anxiety, depression rates were similar in twin and singleton pregnancies. Assisted reproduction may contribute to higher anxiety in twin pregnancies. More research is needed to explore the long-term effects of these outcomes and to develop interventions aimed at improving mental health and cognitive function to improve mental well-being in twin pregnancies.
Challenges of twin delivery
Most women carrying twins are concerned about how and when her babies come into the world? It mostly depends on how her pregnancy progresses and on her health condition. If there are no health concerns and there are no complications involved, she can expect to deliver her twin babies any time after 37 to 38 weeks of pregnancy. The risk of stillbirth may increase if the babies are born later than 38 weeks, as the placentas in twin pregnancy may not support the babies later than that. Therefore, Obstetricians induce labour or advice a caesarean section for the delivery of twins.
Technically Caesarean section is required if:
a. The placenta is covering the opening of the cervix or patient
has placenta is previa
b. She has had caesarean delivery before
c. Her babies are smaller closer to the date of delivery
As majority of the women may have to undergo an emergency
c-section, under the following circumstances
i. If she has high blood pressure or preeclampsia
ii. If her labour gets complicated
iii. If one or both the babies become distressed during the labour
iv. If the umbilical cord falls into the birth canal
v. If her labour is not progressing or is slow
While doctors must help to decide what the best-suited delivery option for each one, in the case of monochorionic twins, they advise going for c-section if there are any complications. The possibility of having a normal delivery may increase if one of your twins is in a head-down position. Caesarean delivery is preferred if the first baby is in a breech position, or if the twins are in a transverse position or if there are some complications. The c-section of twins is the same as the c-section of a single baby. However, off-late most obstetricians in India prefer doing elective caesarean section in India, with a pre-planned date for the surgery, and in case woman goes into labour before that, she will undergo the caesarean delivery on that day itself. If normal delivery is advised, giving birth to twin babies is like giving birth to a single baby. The only difference is that in twin delivery you will be pushing two babies out, but the first stage labour or dilation of your cervix will happen only once. Twin babies are born pre-term in most cases; women go into labour before 38 weeks of their pregnancy. The second baby is born soon after (15-20 minutes on an average) the first one. If the second baby is in the breech position, the doctor may either turn the baby externally or internally.
One can minimize the chances of caesarean delivery by
i) Staying active in pregnancy which improves your chances of
having a normal delivery, despite staying active in the later
months of pregnancy with twins can be quite challenging
ii) It is imperative to stay healthy in each pregnancy, more so
if you are carrying twins, maintaining a healthy lifestyle by
eating healthy food and regularly exercising
iii) Try positioning the babies in a head-down position towards
the end of pregnancy
iv) Support from her partner, family members and even the doctor,
may reduce chances of having an unplanned or an emergency
c-section
Recovery from twin delivery
Whether it’s vaginal or c-section, twin delivery is the same as it is from a single delivery. However, one may lose more blood during delivery. Woman’s back, knees and hips may feel achy for a while as they have borne so much of weight in the last trimester. Her breasts and belly may take a little longer to come back to their shape. She may experience more postpartum blood or lochia compared to a woman who has given birth to a single baby. She would have gained more weight with twin babies. Twin deliveries (vaginal or C-section) require 8-12 weeks of recovery vs. 6 weeks for singletons. The simple mantra is to keep calm and be patient with one’s own body. After about six weeks or so, start doing some mild exercises. More twin moms benefit from rehabilitating abdominal separation and incontinence through pelvic floor therapy. Breastfeeding is the best way to come back to shape and lose all that pregnancy fat, as it not only releases the hormone oxytocin, but it will also help her lose pregnancy fat much faster compared to the mothers delivering single babies. As 25% of twin mothers experience depression twin-specific counselling would be beneficial. For tandem feeding or managing low milk supply mother must maintain 500+ extra calories daily to support milk production [12].
Parental psychosis
Levels of anxiety are higher in the antenatal period among women who are expecting multiples than those who are expecting singletons as was in our second case especially when they have a girl and expected at least one of the twins to be male baby. If the parent knew the sex of the babies and accepted during ANC as was in our first case may not affect their rates of probable anxiety disorders among women as was in or first case. Literature review indicates that at 18 weeks gestation, one thirds of women who conceived via IVF or non-ART treatment would have a probable anxiety disorder versus 19% among women who conceived singletons via IVF and 13% who conceived singletons naturally. At 28 weeks gestation, rates were still higher in the multiples group, but not significantly so. More studies report higher postpartum and early parenthood anxiety among mothers of twins in the early postpartum period (0-12 weeks) and experienced high levels of anxiety at 3 times the rate of mothers of singletons. Mothers of multiples were more likely to report severe parenting stress than mothers of singletons conceived via IVF or non-ART medical treatment. Primiparous mothers of twins may experience more postpartum parenting stress than mothers of twins who already have older child/children as in both of our cases. All studies that compare fathers of multiples and singletons indicate worse mental health outcomes in the postpartum and early parenthood periods in fathers of multiples [13].
Recent Breakthroughs Revolutionizing Outcomes in Twin Births & Maternal Health
Advances in obstetrics and neonatal care are transforming twin pregnancies from high-risk journeys into safer, more manageable experiences through i) Weekly progesterone injections reduce preterm birth risk by 40% in twin pregnancies, as it stabilizes the cervix, extending gestation closer to 37 weeks ii) Laser Surgery for Twin-to-Twin Transfusion Syndrome (TTTS), a Minimally invasive fetoscopic laser surgery corrects uneven blood flow in TTTS, improving survival rates to 85-90% for both twins iv) CPAP machines to support underdeveloped lungs v) Temperaturecontrolled incubators mimicking the womb vi) Neuroprotective care to prevent brain damage in preemies as 95% survival rates for twins born at 28+ weeks [14].
Remaining challenges
Despite immense progress in handling twin pregnancies
several key areas where evidence is limited and additional research
is needed. They are:
Pre-Term Birth (PTB): is the leading cause of neonatal
mortality and morbidity in twin pregnancies. There has been
relatively little progress about the screening & prevention of PTB
in twin pregnancies.
Fetal Growth Restriction (FGR): the main question is of the
diagnosis of FGR in twin pregnancies based on twin-specific charts
or the standard charts used in singleton pregnancies, given that up
to 30% of twin fetuses will be diagnosed with FGR using singleton
charts. Recent data suggest that the slower growth of twin fetuses
may be the result of adaptive mechanisms rather than pathologic
placenta-mediated FGR and that twin-specific charts should,
therefore, be preferred to avoid overdiagnosis of FGR.
Gestational Diabetes (GDM): GDM is more common in twin
than in singleton pregnancies, however, many cases of mild GDM
in twin pregnancies are likely the result of the greater transient
physiologic increase in insulin resistance in twin compared to
singleton pregnancies due to the larger placental mass and not due
to underlying maternal beta-cell dysfunction as in cases of GDM
in singleton pregnancies. More importantly, many of the typical
complications of GDM, such as macrosomia and shoulder dystocia,
are less relevant in twin pregnancies, given that twins grow slower
during the third trimester and are born earlier than singletons.
Adequate maternal Gestational Weight Gain (GWG) in twin
pregnancies is difficult as the nutritional demands are greater and
inadequate GWG has been associated with an increased risk of
preterm birth & fetal growth restriction in twin pregnancies.
Mode and timing of delivery: The optimal mode of delivery
in twin pregnancies is a topic of significant debate. According to
the largest trial the twin birth study, a) The first twin in cephalic
presentation, planned cesarean delivery and planned vaginal
delivery are associated with a similar risk of perinatal mortality
and severe morbidity. A recent secondary analysis of this trial,
a planned CD was associated with a lower rate of less severe
outcomes like intraventricular hemorrhage stage 1-2, low apgar
scores, cord pH <7.0, and need for assisted ventilation at birth than
a planned vaginal delivery. Recently a calculator based on data
from the twin birth study has been developed to facilitate patient
counselling based on their individualized risk of intrapartum CD.
Currently available data regarding the optimal timing of delivery
are largely based on gestational-week-specific estimates of the risk
of stillbirth & neonatal death [14].
Conclusion
Twin Pregnancy occurs when two embryos develop in the uterus simultaneously. Two types of twins are described i) Identical twins, which are formed because of a splitting fertilized egg, & ii) Fraternal twins, where two different ova are fertilized by two different sperm. Identical twins share the same genes and typically resemble each other, whereas fraternal twins are like siblings born at the same time; they may not resemble each other and can be of the same or opposite sex. Twin pregnancies apart from taxing to the woman and the family to take care during entire pregnancy, carry a greater risk of adverse complications like increased preterm delivery, low birth weights, congenital anomalies, and SNCU admission, IUGR, HDP, anemia, PPH, and need for blood transfusions. Even outcomes, especially perinatal mortality and neonatal morbidity increase. Twin delivery is not as easy as a single delivery, gynecologists advocating planned cesarean sections, newborn twin babies may have to spend a few days in the neonatal unit or be in special care for a while. Mental health outcomes in the postpartum and early childhood periods are worse for parents of multiples than parents of singletons and much worse in the cases of higher-order multiples versus twins. However, if proper care and caution are exercised during pregnancy, there are minimal chances of complications. Given the current “epidemic of multiple pregnancies” it is time to examine perinatal physical & mental health closely not only among mothers but both parents of multiples. It is better to consult a specialist and to opt for normal delivery or caesarean delivery, as advised after explaining the pros & cons of both.
References
- (2025) India-to-see-a-million-more-twin-births-by-2100. Mumbai Mirror, India
- Surbhi Pathak (2025) Why experts call for national registry of rising twin births in India, Why Is It Important.
- How-to-determine-zygosity types-of Twins. Twins Research Australia, Australia.
- Zygosity-and-chorionicity-of-twins.
- Hoekstra C, Willemsen G, Nicholas GM, Boomsma DI, Montgomery GW, et al. (2008) Dizygotic twinning. Hum Reprod Update 14(1): 37-47.
- (2015) What are half-identical twins? Washington State Twin Registry, USA.
- Allison KR, How-to-get-pregnant-with-twins.
- Uma MR, Branum AM, Klebanoff MA (2005) Relationship of maternal body mass index and height to twinning. Obstet Gynecol 105(3): 593-597.
- Madhura J, Piyush J (2025) Vanishing twin syndrome: A comprehensive review. International Journal of Innovative Research in Technology 11(4): 447-455.
- Dua M, Prakash V, Sonia M, Bhatia V (2013) ART outcome in young women with premature ovarian aging. J Midlife Health 4(4): 230-232.
- https://www.cdc.gov/art/key-findings/multiple-births.html
- Kishore RK, Usha BR (2022) Multiple pregnancy: Boon or bane-An Indian perspective. Multiple Pregnancy-New Insights.
- Susan JW, Cynthia LB, Katherine MT (2014) Raising multiples: Mental health of mothers and fathers in early parenthood. Arch Women’s Ment Health 18(2): 163-176.
- (2025) Twin-births-maternal-health-risks-advances. Spo_oky.
© 2025 Suresh Kishanrao. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






