- Submissions

Full Text
Gastroenterology Medicine & Research
Modified Heller´s Esophageal Myotomy Associated with Dor’s Fundoplication A Surgical Alternative for the Treatment of Dolico Megaesophagus
Fernando Athayde Veloso Madureira*, Francisco Alberto Vela Cabrera, Vernaza Monsalve M, Moreno Cando J, Charuri Furtado L and Isis Wanderley De Sena Schramm
Department of General Surgery, Brazil
*Corresponding author: A. V. Madureira F, MsC, Phd. Americas Medical City Department of General Surgery, Full Professor of General Surgery At UNIRIO and PUC- Rio, Brazil
Submission: October 09, 2019;Published: October 24, 2019

ISSN 2637-7632Volume3 Issue5
The most performed surgery for the treatment of achalasia is Heller´s esophageal myotomy associated or no with anti-reflux fundoplication. We propose in cases of advanced megaesophagus, specifically in the dolico megaesophagus, a technical variation. The aim of this study was to describe Heller´s myotomy modified by Madureira associated with Dor´s fundoplication as an alternative for the treatment of dolico megaesophagus, assessing its effectiveness at through dysphagia scores and quality of life questionnaires.
Materials and methods: Technical Note describing the surgical procedure and presenting the results of three patients with advanced dolico megaesophagus, operated from 2014 to 2017. The technique proposes the dissection of the esophagus intrathoracic, with circumferential release of it, in the most extensive possible by trans hiatal route. Then the esophagus is retracted and fixed circumferentially in the pillars of the diaphragm with six or seven point. The goal is at least on the third part of the esophagus, to achieve its broad mobilization and rectification of it; then is added a traditional Heller myotomy.
Results: The mean dysphagia score in pre-op was 10points and in the post- op was 1.3 points (maximum of 10 points being observed each between the pre and postoperative 8.67 points, 86.7%) The mean hospitalization time was one day. There was no surgical mortality or conversion to open technique. The mean follow-up time was 30.6 months (24-38 months) (Table 1). Heller’s Cardio myotomy modified by Madureira, associated with Dor’s fundoplication is an option to be investigated for the treatment of the dolico megaesophagus.
Keywords: Megaesophagus; Esophageal myotomy; Heller’s myotomy; Dor’s fundoplication; Dysphagia
Summary
Esophageal achalasia is a rare pathology in the population incidence between 0.03 and 1per 100,000 individuals [1]. It doesn’t have age or gender preference. It’s the most common esophageal motility disorder diagnosed [2]. According to his etiology, it can be classified into idiopathic, chagasic, pseudo achalasia. Trimanoma cruzi infection, in the countries of South America (and Brazil), has a relevant impact and is known that about 5% of patients affected by Chagas disease, they turn on achalasia [3] and that the dilation of the esophagus appears to be greater in the chagasic etiology [4]. The pathophysiology of the disease is seen hypertension in the Lower Esophageal Sphincter (LES) and an inability to drive the esophageal content, for aperistalsis or uncoordinated peristaltic movements. Histologically there is destruction or decrease of the mioenteric plexus cells. The condition usually has insidious onset, and its main symptom is dysphagia. Patients are shown to have poor quality of life, are emaciate and are also limited to their work activities. The most commonly used test for diagnosis is the esophageal manometry that evaluates the motility of the esophagus and lower esophageal sphincter pressure (LESP).
Treatment varies depending on the degree of disease, and it can be medicated, endoscopic or surgical [5]. All modalities of treatment aim to decrease the LESP, so that the residual food in the esophagus can travel to the stomach by gravity. The grade IV megaesophagus and the dolico megaesophagus are the latest phases of the disease, specifically in cases of mega esophagus with tortuosity of the organ (dolico), there is no consensus on the best form of treatment [4,6,7]. Losing the vertical axis of the esophagus in an organ with aperistalsis makes it difficult to gravity emptying. The aim of this study was to describe Heller´s esophageal myotomy modified by Madureira associated with Dor´s fundoplication as a surgical alternative for dolico megaesophagus treatment.
Methodology
Surgical technique
The most performed surgery for the treatment of megaesophagus is Heller´s esophageal myotomy associated or not with anti-reflux fundoplication performed by laparoscopic or robotic [8]. The technique consists of the dissection of the gastric esophagus junction, opening of the freno-esophageal membrane, Isolate the esophagus with cardiac tape or Pen rose drain (there are technical variants that advocate not dissecting the posterior portion of the esophagus) [9]. Heller’s esophageal myotomy is then performed: the muscle fibers in the longitudinal and circular layers of the lower esophagus and proximal stomach are broadly and carefully sectioned by a six to eight cm extension in the esophagus and two to three cm in the stomach. The submucosa remains exposed and the fibers of the esophageal sphincter sectioned, there are technical variants such as the Pinotti technique, that resect a band of esophageal musculature [10,11].
Figure 1: Pinotti’s maneuver, transhiatal dissection and mobilization of inferior esophagus.

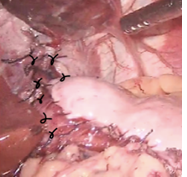
After performing the esophageal myotomy, it is confectioned an anti-reflux fundoplication, some authors recommend not making the valve. It is made a 180 degrees anterior fundoplication, Dor’s Fundoplication, or 270 degrees in anterolateral position, Toupet or Pinotti valves [11,12]. We propose in cases of grade IV megaesophagus, specifically in the dolico megaesophagus, a technical variation. We propose to isolate the esophagus as described with cardiac tape, then dissect the intrathoracic esophagus with circumferential release of it. Performing the dissection more extensively as possible throw the hiatus. When necessary, can be sectioned the anterior fibers of diaphragmatic pillar to increase the surgical field [11] (Figure 1). After the extensive mobilization of the organ, we add the traditional Heller´s esophageal myotomy. Once the myotomy is done and using the repair tape, the esophagus is retracted and we perform its fixation in circumferential fashion on the diaphragm pillars, with six or seven separate sutures. The goal is at least on the third part of the esophagus, to achieve its broad mobilization and rectification of it (Figure 2). After that is performed an anterior, 180 degrees fundoplication (Dor’s). A routine section of short gastric vessels is not made, only if Dor’s valve is retract to the spleen at the end of the procedure (Figure 3).
Figure 2:Traction and fixation of the esophagus to the diaphragmatic pillars.
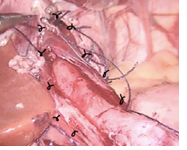
Figure 3:Final view of modified Heller-Dor procedure.
Methods
Where studied patients with Grade IV megaesophagus disease with dolico megaesophagus (Rezende classification), operated between 2014 to 2017, from the Post Graduate Course of Surgery of Catholic Pontifical University PUC-Rio and UNIRIO, Rio de Janeiro. Patients included signed freely consent by agreeing to participate in the study and was submitted and approved by institution ethics and research committee. Diagnosing achalasia was performed through clinical, manometric, endoscope and radiological. The surgical procedure was indicated in patients with grade IV megaesophagus with dolico megaesophagus. It was recorded: clinical history, physical examination, specific exams, recent pre- and postoperative assessment and late, quality of life questionnaires and dysphagia scores.
Quality of life rating
Two questionnaires were used to estimate the quality of life in the pre and postoperative. The questionary applied [13,14] evaluates the combination of frequency and intensity of dysphagia, through punctuation. The 10 points score was measured before and after the surgical intervention. The questionnaires were conducted through interview of patients at the office. The second questionnaire was conducted through a direct interview with the patients, who were asked to graduate in their own words the intensity of improvement in dysphagia grading from zero to 10.
Results
Were studied three patients with dolico megaesophagus operated by modified Heller-Dor, from 2014 to 2017, two patients were men, and one was woman. The three patients studied had negative serology for Chagas disease. Dysphagia was the most common symptom, occurring in 100% of individuals and of severe intensity. Dysphagia for solids and liquids was present 100% of cases. The mean time for dysphagia was 48 months (12 to 120 months). The regurgitation of ingested foods occurred in all cases. They refer to weight loss in 100% of patients, with average loss of weight of 13 kg (10-20 kg). Clinical malnutrition was not reported. Applied the dysphagia score, was found a mean pre op of 5-point for dysphagia frequency and 5-point for intensity. The mean total of the score in the preoperative period was 10 points (maximum of 10 points). None of the patients studied were not subjected to endoscopic pneumatic dilation on pre op.
Table 1:Results and follow up.
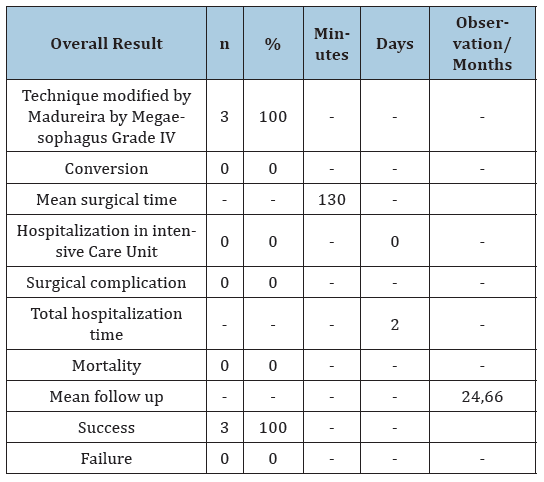
Endoscopy showed achalasia in 100% of cases; the esophagomanometry revealed aperistalsis in 100% of patients. All were classified as Grade IV (Rezende classification) and dolico megaesophagus [15]. The surgical procedure was Heller’s esophageal myotomy modified by Madureira associated with Dor anterior fundoplication in 100% of cases, 2 patients operated on by laparoscopy and 1 by robotic surgery. There were no conversions. The mean operating time was 130 minutes (120-150 minutes). The mean length of esophageal myotomy on esophagus was 7cm and on stomach was 3cm. There was no perforation of the mucosa of the Esophagus. In one patient, was sectioned the short gastric vessels.
Post-operative
The onset of the diet occurred on the first day of the postoperative in all cases. Hospital discharge on the second day (in 24 hours) in 100% of patients. Was considered as a successful treatment on three of the three patients. Applying the dysphagia score in the post-op, we find mean for dysphagia frequency 0.3 points, mean for dysphagia intensity 1 point and a global mean of 1.3 points. The global mean falls between the pre and postoperative dysphagia score, was 8.67 points, which represents a decline of 86.7%. The patient’s assessment of improvement in quality of life with their his own words revealed an average improvement of 93.33%, with 1 of the patients showed a 100% improvement in quality of life and the other two cases showed 90% improvements in quality of life. There was no clinically relevant gastroesophageal reflux. The mean follow-up time was 30.6 months (24-38 months). There was no long-term morbidity (Figure 4).
Figure 4:Radiological evidence of rectification of the esophagus.

Discussion
This study is a technical note that aims to describe heller esophageal myotomy modified by Madureira associated with Dor’s anterior fundoplication as a surgical alternative for the treatment of dolico megaesophagus, it is an initial and prospective series. Esophageal achalasia is a disease that has a negative impact on quality of life, the treatment options seek to reduce the LESP, so that the residual food in the lumen of the esophagus may slip into the stomach by gravity. The Heller-Dor in the control of achalasia, has excellent and good results 78-93%[16-19], is a safe surgery, with short length of stay on hospital, high tax of clinical success, with a significant impact on improving dysphagia and almost no mortality [13,14,17,20-25]. The Heller-Dor is well established as option to control this disease and with studies that showed good results over several years [4,6,17,26,27]. Promising results have been described in endoscope myotomy or POEM mode [28]. The megaesophagus grade IV and the dolico megaesophagus, but specifically cases of megaesophagus with organ tortuosity (dolico), has worse surgical outcome and has no surgical consensus treatment [4,6,26]. The loss of the vertical axis of the esophagus in an organ with aperistalsis, makes it difficult to empty by gravity. Treatment options are the Heller Dor, esophagectomy [6,7,16], and less done Serra Doria Surgery and Thal Hatafuku surgery. The procedure with less morbidity is the laparoscopic Heller-Dor. Many actors choose to indicate the esophagectomy for the dolico megaesophagus that would have the theoretical advantage of resect the esophagus, but which has greater morbidity, longer hospitalization time and does not always improve quality of life for patients. Esophagectomy, according to a review of 301 cases made by Ximenes, for this begin disease, shows mortality of 24% and mortality of 3.97% [29,30]. We propose in cases of grade IV megaesophagus, specifically in the dolico megaesophagus, a variation of technique. We propose the trans hiatal dissection of the intrathoracic esophagus on a circumferential basis, in addition to the traditional Heller´s myotomy. So, the esophagus is retracted, and we perform it fixation on its circumference on the diaphragm pillars with six or seven sutures. The goal is: at least in the third portion of esophagus, to achieve its wide mobilization and rectification of it. Understanding that in cases of already tortuous esophagus, the loss of the vertical axis is largely responsible for the difficulty of emptying and therefore the non-improvement of the dysphagia and quality of life; we propose the rectification (even partial) of it, which can be made through his release into the mediastinal with traction and fixation of the organ on the pillars. The use of Heller associated with antireflux valve, has been defined as an option in the treatment of grade IV megaesophagus. Having reserved esophagectomy for failures of less invasive treatment (Figure 5).
Figure 5:Total score of dysphagie at the postoperative.
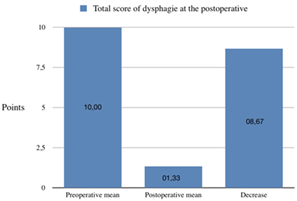
The initial results were encouraging, the surgical impact is of the type of minimally invasive surgery, precocious mobilization, diet return and early discharge of hospital. Null morbid-mortality and in these first cases no complications. Based on dysphagia, we have the improvement in quality of life in 100% of the patients studied. In this study, it was applied the dysphagia score [13,14], based on the frequency and intensity of this, measured in the pre and post-operative period. The mean global fall in the score was 8.67 points representing the 86.7% drop. In this small series the minimal invasive Heller modified by Madureira with Dor fundoplication was capable of interfering with quality and life in a significant way, modifying the symptom dysphagia [31]. There was no gastroesophageal reflux clinically relevant. The importance of publishing this technical variation is for other groups investigate whether these results we found for the treatment of dolico megaesophagus are reproducible and may be a surgical option to be recommended.
Conclusion
Heller’s cardio myotomy modified by Madureira, associated with Dor’s fundoplication is an option to be investigated for the treatment of the dolico megaesophagus.
References
- Boeckxstaens GE, Jonge WD, Vanden Wijngaard RM, Benninga MA (2005) Achalasia: From new insights in pathophysiology to treatment. J Pediatr Gastroenterol Nutr 41(1): 36-37.
- Mayberry JF (2001) Epidemiology and demographics of achalasia. Gastrointest Endosc Clin N Am 11(2): 235-248.
- Dantas RO (2017) Comparison between idiopathic achalasia and chagasic achalasia. Mini-invasive Surg 1: 117-120.
- Herbella FA, Patti MG (2015) Laparoscopic heller myotomy and fundoplication in patients with end-stage achalasia. World Journal of Surgery 39(7): 1631-1633.
- Torresan F, Ioannou A, Azzaroli F, Bazzoli F (2015) Treatment of achalasia in the era of high-resolution manometry. Ann Gastroenterol 28(3): 301-308.
- Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, et al. (2012) Guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26(2): 296-311.
- Alberto A, Emanuele A, Carlo GR, Luigi B (2018) Esophagectomy for stage IV achalasia: Case series and literature review. European Surgery 50(208): 58-64.
- Lopes LR, Braga Nda S, Oliveira GC, Coelho Neto Jde S, Camargo MA, et al. (2011) Results of the surgical treatment of non-advanced megaesophagus using heller-pinotti's surgery: Laparotomy vs. laparoscopy. Clinics 66(1): 41-46.
- Simić AP, Radovanović NS, Skrobić OM, Raznatović ZJ, Pesko PM, et al. (2010) Significance of limited hiatal dissection in surgery for achalasia. J Gastrointest Surg 14(4): 587-593.
- Pinotti HW, Domene CE, Nasi A, Santo MA, Libanori HT, et al. (1995) Video-assisted laparoscopy for the treatment of acalasia. In: Peters JH & DeMeester TR (Eds.), Minimally invasive surgery of the foregut. Quality Medical Publishing, USA, pp. 03-09.
- Pinotti HW, Gama-Rodrigues JJ, Ellenbogen G, Arab-Fadul R, Raia A, et al. (1974) New basis for the surgical treatment of megaesophagus: Esophagocardiomyotomy with esophagus-fundus-gastropexy. Rev Assoc Med Bras 20(9): 331-334.
- Toupet A (1963) Technic of esophago-gastroplasty with phrenogastropexy used in radical treatment of hiatal hernias as a supplement to Heller's operation in cardiospasms. Mem Acad Chir 89: 384-389.
- Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, et al. (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: A prospective randomized double-blind clinical trial. Ann Surg 240(3): 405-412.
- Torquati A, Richards WO, Holzman MD, Sharp KW (2006) Laparoscopic myotomy for achalasia: Predictors of successful outcome after 200 cases. Ann Surg 243(5): 587-591.
- De Rezende J, Lauar KM, De Oliveira A (1960) Clinical and radiological aspects of aperistalsis of the esophagus. Rev Bras Gastroenterol 12: 247-262.
- Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, et al. (2002) Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann surg 235(2): 186-192.
- Bonatti H, Hinder RA, Klocker J, Neuhauser B, Klaus A, et al. (2005) Long-term results of laparoscopic Heller myotomy with partial fundoplication for the treatment of achalasia. Am J surg 190(6): 874-878.
- Oliveira GC, Lopes LR, Andreollo NA, Braga Nda S, Coelho N, et al. (2009) Surgical treatment of megaesophagus at UNICAMP hospital of clinics - associated factors with better and worse results. Rev Col Bras Cir 36(4): 300-306.
- Onopriev V, Durleshter VM, Ryabchun VV (2005) Comparative pre- and postoperative results analysis of functional state of the esophagus assessment in patients with various stages of achalasia. Eur J Cardio Thoracic Surg 28(1): 1-6.
- Gupta R, Sample C, Bamehriz F, Birch D, Anvari M, et al. (2005) Long-term outcomes of laparoscopic heller cardiomyotomy without an anti-reflux procedure. Surg Laparosc Endosc Percutan Tech 15(3): 129-132.
- Pinotti HV (1999) Access to the thoracic esophagus by median transection of the diaphragm. Sao Paulo, Brazil.
- Corcione F, Cristinzio G, Cimmino V, La Manna S, Maresca M, et al. (1997) Surgical laparoscopy with intraoperative manometry in the treatment of esophageal achalasia. Surg Laparosc Endosc 7(3): 232-235.
- Rossetti G, Brusciano L, Amato G, Maffettone V, Napolitano V, et al. (2005) A total fundoplication is not an obstacle to esophageal emptying after Heller myotomy for achalasia: Results of a long-term follow up. Ann Surg 24(4): 614-621.
- Arain MA, Peters JH, Tamhankar AP, Portale G, Almogy G, et al. (2004) Preoperative lower esophageal sphincter pressure affects outcome of laparoscopic esophageal myotomy for achalasia. J Gastrointest Surg 8(3): 328-334.
- Dang Y, Mercer D (2006) Treatment of esophageal achalasia with heller myotomy: Retrospective evaluation of patient satisfaction and disease-specific quality of life. Can J Surg 49(4): 267-271.
- Eduardo RZC, Fernando AVM, Delta M, Renato MS, Antonio CRGI, et al. (2017) Late evaluation of dysphagia after heller esophageal myotomy with dor fundoplication for achalasia. Circulation Bras 30(3): 182-184.
- Costantini M, Salvador R, Capovilla G, Vallese L, Costantini A, et al. (2019) A thousand and one laparoscopic heller myotomies for esophageal achalasia: A 25-year experience at a single tertiary center. J Gastrointest Surg 23(1): 23-35.
- Hernández MOV, Solórzano POM, González MMA, Blancas VJM, Caballero LC, et al. (2019) Peroral endoscopic myotomy for the treatment of achalasia and other motor disorders of the esophagus: Short- and medium-term results at a Mexican tertiary care center. Rev Gastroenterol Mex 84(1): 1-10.
- Ximenes NM (1991) Megaesophagus: Current review of techniques and results. Rev Saude Dist Fed 2: 207-236.
- Devaney EJ, Lannettoni MD, Orringer MB, Marshall B (2001) Esophagectomy for achalasia: Patient selection and clinical experience. Ann Thorac Surg 72(3): 854-858.
- Torresan F, Ioannou A, Azzaroli F, Bazzoli F (2015) Treatment of achalasia in the era of high-resolution manometry. Ann Gastroenterol 28(3): 301-308.
© 2019 Athayde Madureira F. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






