- Submissions

Full Text
Experimental Techniques in Urology & Nephrology
Predictors of 30-Day Complications after Radical Cystectomy
Atduev VA1,2, Gasrataliev VE2*, Ledyaev DS1,2, Belsky VA2, Lyubarskaya YuO1,2 and Mamedov HM1
1FGBOU VO “Nizhny Novgorod State Medical Academy“ of the Ministry of Health of Russia, Russia
2FBUZ “Privolzhsky District Medical Center“ of the Federal Medical and Biological Agency of Russia, Russia
*Corresponding author: Gasrataliev VE, FBUZ "Privolzhsky District Medical Center” of the Federal Medical and Biological Agency of Russia, Russia, 603001 Nizhny Novgorod, Nizhnevolzhskaya Embankment
Submission: December 12, 2017; Published: January 19, 2018

ISSN: 2578-0395 Volume1 Issue3
Abstract
The authors studied the influence of various predictors on the development of complications arising after radical cystectomy in 182 patients. Bacteriological monitoring demonstrated a high level of infection of the abdominal cavity after RC (54.4%). After RC in 98 (53.8%) patients, the development of various complications in the Clavien system was recorded. The most frequent categories of complications were gastrointestinal (26.9%) and infectious (25.8%). The development of complications is affected by anemia before surgery, body weight deficiency, intraoperative blood loss intraabdominal infection.
Keywords: Bladder cancer; Radical cystectomy; Complications
Abbreviations: RC: Radical Cystectomy; OR: Odds Ratio; BMI: Body Mass Index
Introduction
In the past decade, there has been clear progress in the surgical technique of radical cystectomy (RC), as well as in anesthesia and perioperative management of patients, which was manifested in a significant reduction in the number and severity of complications associated with this operation. However, the proportion of complications is still high, and develops in approximately 58% of patients and causes death in 1.6%-3.9% of cases within 30 days after surgery [1-10]. An analysis of the causes of their development and the search for effective ways to prevent them is topical.
Objective: To determine the most significant predictors of complications after RC.
Materials and Methods
The present study is retrospective and is based on an analysis of the results of treatment of 182 patients exposed to the RC from 2014 to 2016. The operations were performed in the Privolzhsky District Medical Center of the FMBA of Russia in Nizhny Novgorod. Preoperative preparation and postoperative management of patients did not differ. All operations were performed by one surgeon. To be included in the study, patients had to undergo RC for bladder cancer, other pelvic tumors with germination in the bladder and microcystis of various etiologies. For the purpose of bacteriological monitoring, a lavage liquid was taken from the abdominal cavity at the end of the operation for microbiological analysis. This condition was also mandatory for inclusion in the study. Those patients who did not undergo lavage fluid studies were excluded from the study. Patients were selected from 9 September 2014 to 31 December 2016. All patients operated on for malignant tumors of the pelvic organs performed an enlarged and in some cases super-dilated (up to renal vessels) retroperitoneal lymphadenectomy. Then the standard stages of radical cystectomy were performed. The next stage of the operation was the realization of the most favorable for the patient method of urine derivation. Then the final hemostasis was carried out. The abdominal cavity was washed with a sterile liquid with the evacuation of blood clots and fragments of adipose tissue. Twice lavage fluid from the abdominal cavity was performed for microbiological analysis (before washing and after evacuation). For the analysis and stratification of the results, RC used the classification of surgical complications in the Clavien system [11]. The statistical analysis of the material was carried out on a personal computer using the IBM SPSS Statistics Version 14.0.1 license package. The effect of different predictors on the incidence of complications in 30 days after the operation was analyzed. To identify independent predictors of complications in the postoperative period, we conducted a one-factor and multivariate regression analysis. The relationship between each quality of the indicator and its potential was analyzed with graphical and Kruskall- Wallis test. The odds ratio (OR) was estimated using regression analysis (logistic regression). The critical level of significance in testing statistical hypotheses was assumed to be 0.05.
Results
The study included 182 operated patients. 152 patients (83.5%) males and 30 (16.5%) females with a mean age of 62.3 years (range, 31-84 years) were enrolled in this study. Indications for the performance of RC in 169 (92.8%) cases were bladder cancer: 38 (20.9%)-non-invasive muscle cancer, 131 (72%)-muscle-invasive cancer (T2a-33 (18.1%), T2b-42 (23.1%), T3a-11 (6%), T3b-16 (8.8%), T4a-29 (16%). In 9 (4.9%) patients, the bladder was removed for other pelvic tumors with bladder germination. 4 (2.2%) patients underwent surgery for microcystis of different etiology. External urinary diversion was used in 43 (23.65%) patients: Briker operation-38, ureterocutaneostomy-3, heterotopic reservoir with "dry" urostoma-1. Urine discharge into the sigmorectal reservoir in Mainz-spider II was performed in 1 (0, 55%) of the case. Most patients have an orthotopic urinary diversion-138 (75.8%): Studer-73, Y-shaped reservoir-45, from ileocecal angle in various modifications-11, VIP-7, Camey II -1, Reddy-1. In connection with the prevalence of patients of the older age group, the proportion of concomitant pathology associated with age was quite high. The most frequent were cardiovascular diseases-69.8%, gastrointestinal tract-34%, chronic obstructive pulmonary disease-18.1%, obesity-24.7%, diabetes mellitus-13.7%. Various types of nutritional status disorders by the body mass index (BMI) were recorded in 113 (62%) patients. We performed preoperative correction of the revealed concomitant pathology of these patients together with profile specialists as concomitant diseases are important factors which influence the development of complications of RC. Patients with the highest values on the ASA scale and the Charlson Comorbidity Index were prepared for the operation even in the pre-hospital stage together with an anesthesiologist and resuscitator.
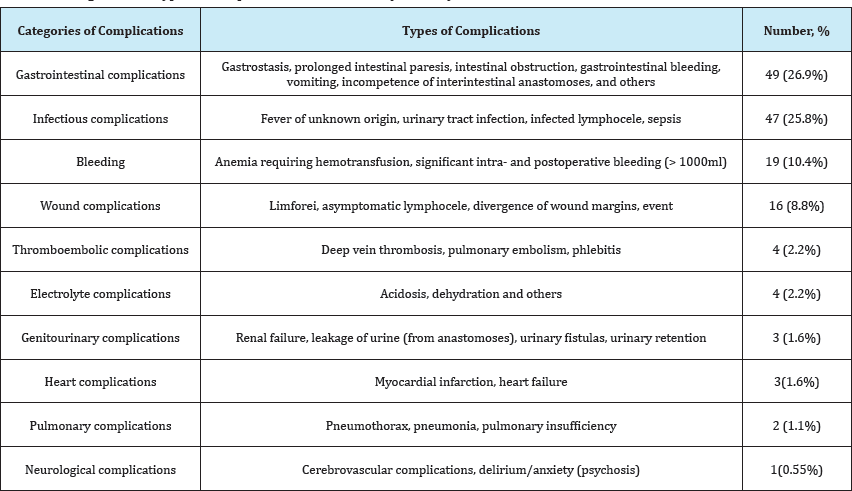
In microbiological analysis of fluid culture from the abdominal cavity revealed the presence of infection in 54.4% of patients. The most frequent agents in cultures from the abdominal cavity were Esherichia coli-42.4%, Enterobacter spp.-21,2%, Enterococcus spp.-26.3%. Extended-spectrum beta-lactamases produced 2% of bacteria. MRSA in 1% of cases, Pseudomonas aeruginosa-in 3%. Washing of the abdominal cavity with a sterile liquid significantly reduced the titer of microbial contamination of 45.1% of infected patients (t=3.975, p<0.001). The high level of infection abdominal cavity, indicates that RC refers to contaminated and sometimes "dirty" operations. In our study, 84 (46.2%) patients had no complications in the 30-day period after RC. The rest 98 (53.8%) patients recorded the development of various undesirable deviations in the postoperative period. The most frequent categories of complications were gastrointestinal and infectious (Table 1).
Table 1: Categories and types of complications after radical cystectomy.
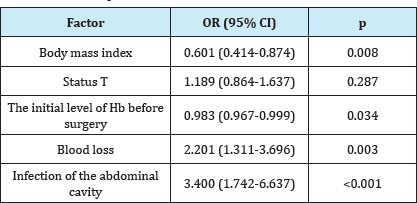
To find the most significant predictors of complications in the 30-day period after the operation, one- and multifactorial regression analysis was performed (Tables 2 & 3). It has been established that the incidence of complications after RC is affected by the body mass index (p=0.008), anemia before surgery (Hb<90g/l), (p=0.034), blood loss (>600ml.) (P=0.003) and infection of the abdominal cavity (p<0.001).
Table 2: Single-factor regression analysis of predictors of the incidence of complications after RC.
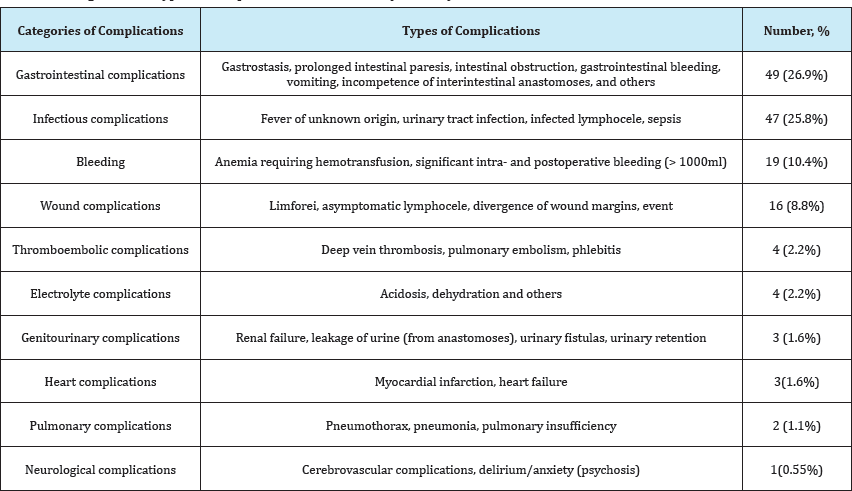
Table 3: Multivariate regression analysis of predictors of the incidence of complications after RC.
Predictors of development of the intestinal paresis were male sex (p=0.019) and infection of the abdominal cavity (p=0.004). In men, the chance of developing an intestinal paresis was 5.8 times higher than that of women (OR=5,888). Intestinal paresis in patients with a positive lavage culture flush is almost 3 times higher than in patients whose flushes were sterile (OR=2.96). The presence of intra-abdominal infection, proved by bacteriological analysis (positive flushing), is a significant independent predictor of the development of infectious complications in the postoperative period (p=0.001) (Table 4). The development of infectious complications in patients who have a "positive" flush is 3.7 times greater than in patients whose flushes were sterile (OR=3.773). There was also a tendency (0.05<- 0.06) that anesthesia time (p=0.059) and operation time (p=0.056) may be predictors of the development of infectious complications.
Table 4: Predictors of the development of infectious complications (single-factor regression analysis).

Discussion
Complications associated with RC can be directly related to both concomitant diseases of the patient, and to the peculiarities of surgical intervention and methods of urine diversion. [12,13]. According to the literature, adverse events of any degree occur in approximately 58% of patients and lethality reaches 3.9% within 30 days after surgery [1-10, 14-18]. The results of our study correspond to these data. In our study, complications were recorded in 53.8% of cases, the lethality was 1.64%. The number and severity of postoperative complications of RC are influenced by the experience of the surgeon and the institution where these operations are performed [9,15]. This is confirmed by the analysis of the results of an earlier series of our RC, carried out in the period from 2008 to 2011. Of the 174 patients in the 30-day period after the operation, complications were recorded in 71.8% of patients, the 30-day mortality was 6.3% [2].
In the structure of complications of RC, according to various authors, gastrointestinal and infectious complications prevail [1,1921]. Paresis ofthe stomach and intestine occurs in 22.7% of patients, intestinal obstruction occurs in 8.7% of cases [1]. Complications of infectious nature range from 20.5 to 33% [1,19,22-25]. According to Haraz AM et al. [24] Among 1000 analyzed patients who underwent RC, one of the most frequent complications was urinary tract infection, intestinal obstruction [24]. Even after laparoscopic and robot-assisted cystectomy complications of an infectious nature can reach up to 41% [20,21]. These data coincide with the results of this study. Gastrointestinal and infectious complications were most frequent and amounted to 26.9% and 25.8%, respectively.
In multivariate analysis, we proved that the development of complications in the 30-day period after the RC is influenced by factors such as the presence before the operation of anemia (less than 90g/L), body weight loss, intraoperative Blood loss (more than 600ml) of intraoperative infection of the abdominal cavity 3). All these factors are interrelated: in patients with locally advanced tumors, hemorrhage (haematuria) is observed for a long time before the operation, which leads to anemia in patients. RC in this category of patients is associated with intraoperative blood loss. As a result, malnutrition (body weight deficiency) and anemia lead to deficiency of lymphocytes, hypoalbuminemia, hypercatabolism, negative energy balance, the barrier function of the intestinal mucosa is also lost, motor-evacuator function is slowed down, immune defenses decrease. These data coincide with the results of recent studies in which it is reported that low BMI, hypoalbuminemia [26,27], bleeding [28] and patient infection [22,23] are predictors of complications in the postoperative period [29].
Conclusion
RC is associated with a high risk of developing various complications in the early stages after the operation. In this study, the main causes of complications were anemia before surgery, weight loss, intraoperative blood loss, intra-abdominal infection. Research in the field of etiology and prevention of complications in the RC should continue.
References
- Shabsigh A, Korets R, Vora KC, Brooks CM, Cronin AM, et al. (2009) Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol 55(1): 164-176.
- Atduev VA, Mamedov HM (2011) Ranevyie oslozhneniya posle radikalnoy tsistektomii. Urologiya 5: 89-91.
- Perepechay VA, Vasilev ON, Spitsyin IM, Kogan MI (2016) Prediktoryi morbidnosti radikalnoy tsistektomii i razlichnyih variantov uroderivatsii: 20-letniy opyit odnogo hirurgicheskogo tsentra. Onkourologiya 1: 42-57.
- Novara G, De Marco V, Aragona M, Boscolo-BR, Cavalleri S, et al. (2009) Complications and mortality after radical cystectomy for bladder transitional cell cancer. J Urol 182(3): 914-921.
- Hautmann RE, de Petriconi RC, Volkmer BG (2010) Lessons learned from 1,000 neobladders: the 90-day complication rate. J Urol 184(3): 990-994.
- Svatek RS, Fisher MB, Matin SF, Kamat AM, Grossman HB, et al. (2010) Risk factor analysis in a contemporary cystectomy cohort using standardized reporting methodology and adverse event criteria. J Urol 183(3): 929-934.
- Lawrentschuk N, Colombo R, Hakenberg OW, Lerner SP, Mansson W, et al. (2010) Prevention and management of complications following radical cystectomy for bladder cancer. Eur Uro 57(6): 983-1001.
- Bostrom PJ, Kossi J, Laato M, Nurmi M (2009) Risk factors for mortality and morbidity related to radical cystectomy. BJU Int 103(2): 191-196.
- Waingankar N, Mallin K, Smaldone M, Egleston BL, Higgins A, et al. (2017) Influence of Hospital and Surgeon Volume on Short-Term Mortality After Radical Cystectomy. BJU Int 120(2): 239-245.
- Morgan TM, Keegan KA, Barocas DA, Ruhotina N, Phillips SE, et al. (2011) Predicting the Probability of 90-day Survival in Elderly Bladder Cancer Patients Treated with Radical Cystectomy. J Urol 186(3): 829-834.
- Dindo D, Demartines N, Clavien PA (2004) Classification of Surgical Complications. A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg 240(2): 205-213.
- Sood A, Kachroo N, Abdollah F, Sammon JD, Loppenberg B, et al. (2017) An Evaluation of the Timing of Surgical Complications Following Radical Cystectomy: Data From the American College of Surgeons National Surgical Quality Improvement Program. Urology 103: 91-98.
- Abe T, Takada N, Kikuchi H, Matsumoto R, Osawa T, et al. (2017) erioperative morbidity and mortality of octogenarians treated by radical cystectomy-a multi-institutional retrospective study in Japan. Jpn J Clin Oncol 47(8): 755-761.
- Nieuwenhuijzen JA, de Vries RR, Bex A, van der Poel HG, Meinhardt W, et al. (2008) Urinary diversions after cystectomy: the association of clinical factors, complications and functional results of four different diversions. Eur Urol 53(4): 834-844.
- Hollenbeck BK, Daignault S, Dunn Rl, Gilbert S, Weizer AZ, et al. (2007) Getting under the hood of the volume-outcome relationship for radical cystectomy. J Urol 177(6): 2095-2099.
- Stimson CJ, Chang SS, Barocas DA, Humphrey JE, Patel SG, et al. (2010) Early and late perioperative outcomes following radical cystectomy: 90- day readmissions, morbidity and mortality in a contemporary series. J Urol 184(4): 1296-1300.
- Lowrance WT, Rumohr JA, Chang SS, Clark PE, Smith Jr JA, et al. (2008) Contemporary open radical cystectomy: analysis of perioperative outcomes. J Urol 179(4): 1313-1318.
- Novotny V, Hakenberg OW, Wiessner D, Heberling U, Litz RJ, et al. (2007) Perioperative complications of radical cystectomy in a contemporary series. Eur Urol 51(2): 397-402.
- Hara N, Kitamura Y, Saito T, Komatsubara S, Nishiyama T, et al. (2008) Perioperative antibiotics in radical cystectomy with ileal conduit urinary diversion: efficacy and risk of antimicrobial prophylaxis on the operation day alone. Int J Urol 15(6): 511-515.
- Wittig Kristina (2016) Critical Analysis of Hospital Readmission and Cost Burden After Robot-Assisted Radical Cystectomy. Journal of Endourology 30(1): 83-91.
- Khan MS, Elhage O, Challacombe B, Rimington P, Murphy D, et al. (2011) Analysis of early complications of robotic-assisted radical cystectomy using a standardized reporting system. Urology 77(2): 357-362.
- Takeyama K, Matsukawa M, Kunishima Y, Takahashi S, Hotta H, et al. (2005) Incidence and risk factors for surgical site infection in patients with radical cystectomy with urinary diversion. J Infect Chemother 11(4): 177-181.
- Yamamoto S, Kunushima Y, Kanamaru S, Ito N, Kinoshita H, et al. (2004) A multi-center prospective study for antibiotic prophylaxis to prevent perioperative infections in urologic surgery. Hiniokika Kiyo 50(10): 673683.
- Harraz AM, Osman Y, El-HS, Laymon M, Mosbah A, et al. (2015) Risk factors of hospital readmission after radical cystectomy and urinary diversion: analysis of a large contemporary series. BJU International 115(1): 94-100.
- Osawa T, Ambani S, Olugbade JrK, Skolarus TA, Weizer AZ, et al. (2017) Potential Implications of Shortening Length of Stay Following Radical Cystectomy in a Pre-ERAS Population. Urology 102: 92-99.
- Matthew JY, Muhammad E, Philip W, Mohantha D (2017) Radical cystectomy in the elderly-Is this a safe treatment option? Arab J Urol 15(4): 360-365.
- David CJ, Stephen BR, Matthew EN, Jonathan EM, Woods ME, et al. (2015) Nutritional Predictors of Complications Following Radical Cystectomy. World J Urol 33(8): 1129-1137.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of Surgical Site Infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20(4): 250-278.
- Health Protection Agency (2006) Surveillance of Surgical Site Infection in England: October 1997 - September p. 123.
© 2018 Atduev VA, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






