- Submissions

Full Text
COJ Nursing & Healthcare
The Outcomes of Implementing Evidence-Based Practice on Diaper Dermatitis for Children Aged 0-14 Years Guided by the Iowa Model
Ma Ana Flor C Pascua1, Millie Obra2*, Jayaselvi John Joseph3,4, Estrella Bicoy Mendoza4, Yasser Sami Amer5,6,7, Jennifer Orbeso8, Sukila K D Isaac9, Reena Crystal Selvin4, Manal Mohammed Al Amri9,3, Melissa Padilla10, Maria Theresa Bote Rojas4 and Lima Matthew11
1Prince Sultan Cardiac Center, Riyadh City, Kingdom of Saudi Arabia
2College of Nursing, Shaqra University, Riyadh, Saudi Arabia
3Corporate Nursing Affairs, King Saud University Medical City, Riyadh, Saudi Arabia
4Pediatrics Department, King Khalid University Hospital, King Saud University Medical City, Riyadh, Kingdom of Saudi Arabia
5Clinical Practice Guidelines and Quality Research Unit, Corporate Quality Management Department, King Saud University Medical City, Riyadh, Kingdom of Saudi Arabia
6Research Chair for Evidence-Based Health Care and Knowledge Translation, Deanship of Scientific Research, King Saud University, Riyadh, Kingdom of Saudi Arabia
7Department of Internal Medicine, Ribeirão Preto Medical School, University of São Paulo (FMRP-USP), Ribeirão Preto, 9São Paulo, Brazil
8Boston Medical Health System, Boston, Massachusetts, USA
9Women’s Health, Ob Gyne Department, King Khalid University Hospital, King Saud University Medical City, Riyadh, Kingdom of Saudi Arabia
10Neonatal Intensive Care Unit (NICU), Pediatrics Department, King Khalid University Hospital, King Saud University Medical City, Riyadh, Kingdom of Saudi Arabia
11Pediatric Intensive Care Unit (PICU), Pediatrics Department, King Khalid University Hospital, King Saud University Medical City, Riyadh, Kingdom of Saudi Arabia
*Corresponding author: Millie Obra, College of Nursing, Shaqra University, Riyadh, Saudi Arabia
Submission: September 10, 2025;Published: October 28, 2025

ISSN: 2577-2007Volume9 Issue 4
Abstract
Diaper dermatitis poses a significant challenge for pediatric nurses, especially in hospitals. In 2021, 13 cases were reported across pediatric units in Riyadh, Saudi Arabia, highlighting the need for standardized assessment, management, and treatment. The team launched an Evidence-Based Practice (EBP) initiative aimed at reducing the severity of diaper dermatitis in children aged 0-14 years by adapting and implementing a skin care bundle, led by pediatric nurses, within the pediatric units of a tertiary teaching hospital in Saudi Arabia over a 36-month period. The EBP team reviewed and synthesized related literature from various online databases, resulting in 41 relevant articles. After reviewing and synthesizing these articles, four were selected based on their relevance and the strength of the evidence. Consequently, the practice change focused on risk identification and early detection, hygiene and diapering practices, treatment approaches, consultation and referral, nursing competence and documentation, and caregiver education. Data from staff questionnaires and patient documentation were used to pre- and post-evaluate the three-year practice change across pediatric units. Overall, implementing an evidence-based practice initiative improved pediatric nursing practices over a 36-month period. The initiative needs to be integrated and maintained across pediatric units.
Keywords:Diaper dermatitis; Diaper dermatitis management and treatment; Evidence-based practice; Iowa model; Buckley scale; Algorithm of diaper dermatitis
Introduction
Severe diaper dermatitis is a skin condition in infants who wear diapers that compromises skin integrity, but it is preventable. Approximately 50% to 65% of babies will experience diaper rash, which typically peaks between nine and twelve months of age. Germany (14.9%) has the highest prevalence rate, followed by the United States (8.7%) and China (1.3%), although it occurs relatively infrequently [1]. Diaper dermatitis is a common condition among infants in Saudi Arabia, with prevalence rates differing by region. Studies show a high prevalence of 80.8% in Al-Qunfudhah and a lower rate of 39.3% in Al-Baha, particularly affecting children aged 19-24 months and occurring more frequently in females. In Jazan, while prevalence was not directly measured, over 90% of mothers were aware of diaper dermatitis, indicating widespread awareness. Overall, the condition affects a significant proportion of infants nationwide, with rates ranging from approximately 39% to 81% [2].
Diaper Dermatitis (DD) is generally not a severe medical condition; however, if left untreated, it can progress and result in secondary infections. Also known as diaper rash, diaper dermatitis affects the perianal region of an infant’s skin, presenting with ulcers, scales, and disrupted skin integrity, as well as papules, edema in the rash area, and spotty or continuous redness [3]. When this clinical manifestation occurs, the baby becomes increasingly irritable, experiences changes in sleep patterns, and feels pain and discomfort in the diaper area. Consequently, the parent or caregiver may feel guilty about their perineal care practices. However, maintaining healthy skin and preventing atopic dermatitis were the most frequently cited care goals among caregivers [4].
Nurses play a crucial role in preventing and managing Diaper Dermatitis (DD) by conducting early assessments, providing standardized care, and educating caregivers. Recent research indicates that proper care for the diaper area involves (1) regular diaper changes, (2) using effective but gentle cleansers, and, if needed, (3) applying topical products that restore barriers [5]. Moreover, nurses also educate parents about hygiene practices and early symptom recognition, which enhances adherence and decreases the likelihood of symptom recurrence. These interventions underscore the crucial role of nursing in promoting infant comfort and maintaining skin integrity [6].
On the other hand, nurses face challenges in caring for diaper dermatitis when practitioners demonstrate varied clinical approaches and delay the application of new evidence. Expanding the skin care protocol to all neonates in the NICU and nursery could help maintain skin integrity and reduce diaper dermatitis in the NICU [4]. Similarly, with the development of new algorithms, assessment tools, and proper education for nurses, there is potential for significant improvement in diaper dermatitis care, reducing stress, pain, and discomfort for both the child and the parents [7].
Purpose
This evidence-based practice initiative aims to reduce the severity of diaper dermatitis in children aged 0-14 years by adapting and implementing a skin care bundle, led by pediatric nurses, within the pediatric units of a tertiary teaching hospital in Saudi Arabia within 36 months.
Evidence-Based Practice Process
The Iowa model revised: Evidence-based practice to promote excellence in health care guided the EBP process accurately, effectively, and precisely in selecting implementation strategies for adopting and maintaining Evidence-BASED PRACTICE (EBP) recommendations, thereby improving processes and outcomes [8].
Identified triggering issues/opportunities for EBP. An incident report in one of the pediatric units described an 11-month-old infant admitted with a chief complaint of persistent diarrhoea, occurring 11 times a day for one week. The infant was evaluated in the pediatric emergency department and later diagnosed with COVID-19. She exhibited an unusual red, tender-looking rash in the diaper area with bleeding around the buttocks and genitals. Additionally, she cried when the diaper area was washed or touched after urination or stool passage. While in the COVID ward, supportive care was provided for her diarrhoea. The infant was discharged on the fourth day after testing negative for COVID-19, achieving optimal nutritional status, and having her diarrhoea controlled. The physician prescribed topical treatments for diaper dermatitis, including fusidic acid twice daily, 1% hydrocortisone cream twice daily, zinc oxide cream, and Vaseline, but there was no improvement. For this reason, an EBP initiator reviewed the incidence of DD and found 13 cases across the pediatric units between October and December 2021.
Is this topic a priority? Nurses face challenges in caring for DD when practitioners demonstrate varied clinical approaches and delay the application of new evidence. In this case, diaper dermatitis was a priority topic for the pediatric units because there was no algorithm, assessment tool, or proper education available for nurses when the team started the EBP initiative. Diaper dermatitis causes stress, pain, and discomfort to a child and their parents [7]. Form a Team. The DD team comprises nursing service managers, nurse educators, head nurses, clinical resource nurses, and staff nurses from various departments, including neonatal intensive care, pediatric intensive care, pediatric emergency, pediatric outpatient clinic, pediatric inpatient care, pediatric isolation, pediatric oncology, and the postnatal unit.
Synthesis of evidence
Based on the Population (P), Intervention (I), Comparison (C), Outcome (O), and Time (T) components, the nurse researcher assisted in the searching of articles from a wide range of online databases, including PubMed, CINAHL, ScienceDirect, DynaMed, and the Saudi Digital Library, for relevant material. The PICOT question, “Does the use of a skincare bundle (I) reduce the severity of DD (O) for children aged 0-14 years with DD (P) within 36 months (T)?” was the topic of a systematic search conducted to collect the best evidence over the last five years (2018-2022) that was written in English. Wipes, petrolatum, zinc oxide, practice guidelines, prevention, protective film barrier, diaper rash, nappy rash, atopic dermatitis, dermatitis scale, and skin barrier were among the search terms used. A comprehensive literature search yielded 41 articles for review.
Following the review and synthesis of the articles, four articles were selected based on their relevance and the high strength of evidence. First, the Evidence-Based CPG: Neonatal Skin Care, 4th Edition [9] applies to all neonatal healthcare settings and other healthcare facilities that provide care related to skin assessment, skin injury, bathing, cord care, diaper dermatitis and diaper wipes, emollient use for dry skin and atopic dermatitis, and parent education. Second, the Dynamed [10] guideline recommendations for management and prevention associated with the increased incidence of diaper dermatitis in children. Third, a systematic review of the ABCDE approach as an effective alternative intervention recommended for nonpharmacological interventions in neonates and children with DD and impaired skin integrity [11]. Lastly, the new Buckley Scale assessment tool was included in the practice recommendation because it is a validated, easy-to-use, reliable, and effective tool for determining scores for the overall severity of DD and for detecting changes in severity [7].
The EBP team decided to appraise the quality of the selected Evidence-Based CPG critically: Neonatal Skin Care, 4th Edition, using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) instrument [12]. After the AGREE II appraisal, the domain scores were used to select high-quality guidelines as the source material for adaptation, endorsement, or implementation. Several published AGREE II appraisal reviews proposed cutoff points for quality classification of guidelines, even though the AGREE Enterprise did not mandate them.
The DD team established quality threshold criteria as high (>70%), moderate (50-70%), low (30-50%), and insufficient (<30%). The results indicated that three domains received highquality scores: Domain 4 (Clarity of Presentation) at 100%, Domain 3 (Rigour of Development) at 81%, and Domain 6 (Editorial Independence) at 75%. Domains 2 and 5 were categorized as moderate, while Domain 1 was rated low. Overall, the assessment by the two appraisers recommended the use of the guideline.
Practice Change
Diaper Dermatitis (DD) is one of the most common skin conditions in infants, affecting up to 25% within the first month of life. The condition can range from mild redness and scaling to painful sores and ulcerated lesions if left untreated. Evidence-based guidelines highlight that prevention is the most effective approach, supported by standardized clinical pathways that promote consistent nursing care. Based on the evidence in the literature, the summary of recommendations for the DD practice protocol is briefly described below.
Risk Identification and Early Prevention
A key part of effective DD management is identifying risk factors early. Infants with frequent loose stools, often caused by gastrointestinal issues or infectious diarrhoea, are at higher risk. Antibiotic use, opiate withdrawal, abnormal rectal sphincter tone, and food allergies also make infants more prone to DD. Supporting and encouraging breastfeeding throughout infancy provides protective benefits and reduces the risk of skin breakdown. Nurses are essential in performing focused skin assessments, such as using the Buckley Scale, as shown in Table 1, to evaluate the perineal area and identify early changes systematically.
Table 1:Buckley Scale-Scoring System for Diaper Dermatitis.
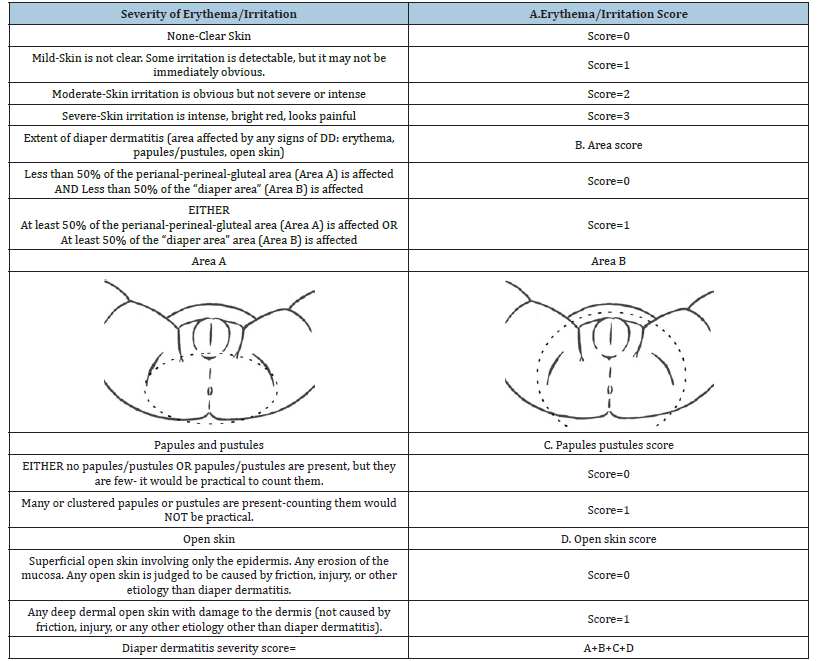
Note: Adopted with permission from Buckley et al. [7].
Description of the Buckley Scale
1. Using the scale, an overall DD severity score is calculated by adding together scores for four dimensions:
The severity of erythema or irritation
Score for the severity of erythema in the most severely affected area is assigned according to the guidance presented in Table.
Color words have been avoided in most descriptions because different severities may present as different colors in children with differing skin tones.
Color is referred to only in severe erythema, which was observed as bright red in all skin tones.
Extent of DD
A score for the area with any signs of DD (erythema, papules or
pustules, open skin) is determined using the guidance in Table after
visual estimates have been made of the proportion affected by two
general areas:
A. The perianal–perineal–gluteal region (Fig. 1A)
B. The wider “diaper area” (the perianal–perineal–gluteal region,
inguinal region, upper thighs, or skin folds enclosed by the
diaper) (Fig. 1B)
Papules or pustules
The scale adopts a practical approach to determining whether there are many papules or pustules, only a few, or none. Then, a score is determined using the guidance in Appendix 2.
Open skin
A score of 1 is given for the presence of any deep dermal open skin that involves damage to the dermis.
When only superficial open skin is observed, a score of 0 is given (Table 1).
Assessing a high score because of the presence of only
superficial open skin tended to lead to a poor reflection of the
overall healing of DD.
2. If the score is 0-3, care management is according to independent
nursing practice or nursing intervention.
3. If the score is 4-6, refer to the physician for further treatment
recommendations in Appendix 2.
4. Assessment is conducted with the child in a lithotomy position,
revealing the most commonly affected areas.
5. Irritation, abrasions, open skin, or other wounds judged to
result from friction (as a result of over-vigorous cleaning), acid
burn, or other causes should not be included in the assessment
of DD severity.
Hygiene and Diapering Practices
Routine diaper changes are essential for preventing infections. For healthy infants, diapers should be changed every 2-3 hours, after each passage of stool, and without harsh scrubbing. Using commercially prepared wipes, especially those free of alcohol, fragrances, and irritants, is recommended over plain water because they help maintain skin integrity and lower microbial exposure. Superabsorbent disposable diapers are preferred, especially for infants showing signs of dermatitis. Dye-free options should also be considered for infants with known allergies. Cleaning using gentle methods, such as warm water, damp cloths, or non-irritating wipes, to avoid harsh scrubbing that could damage the skin barrier.
Treatment Approaches
Management of DD is guided by severity scoring, which evaluates erythema, lesion extent, papules or pustules, and skin integrity, as shown in Table 2. Scores range from 0 (clear skin) to 6 (severe involvement). For mild cases (scores 0-3), nursing interventions such as barrier creams and the ABCDE approach are sufficient, as shown in Table 2. Severe cases (scores 4-6) require physician-directed treatment, which may include topical antifungal or anti-inflammatory therapies. This stratified approach ensures that care is both efficient and appropriately escalated.
Table 2:Management and Treatment for Diaper Dermatitis (DD).
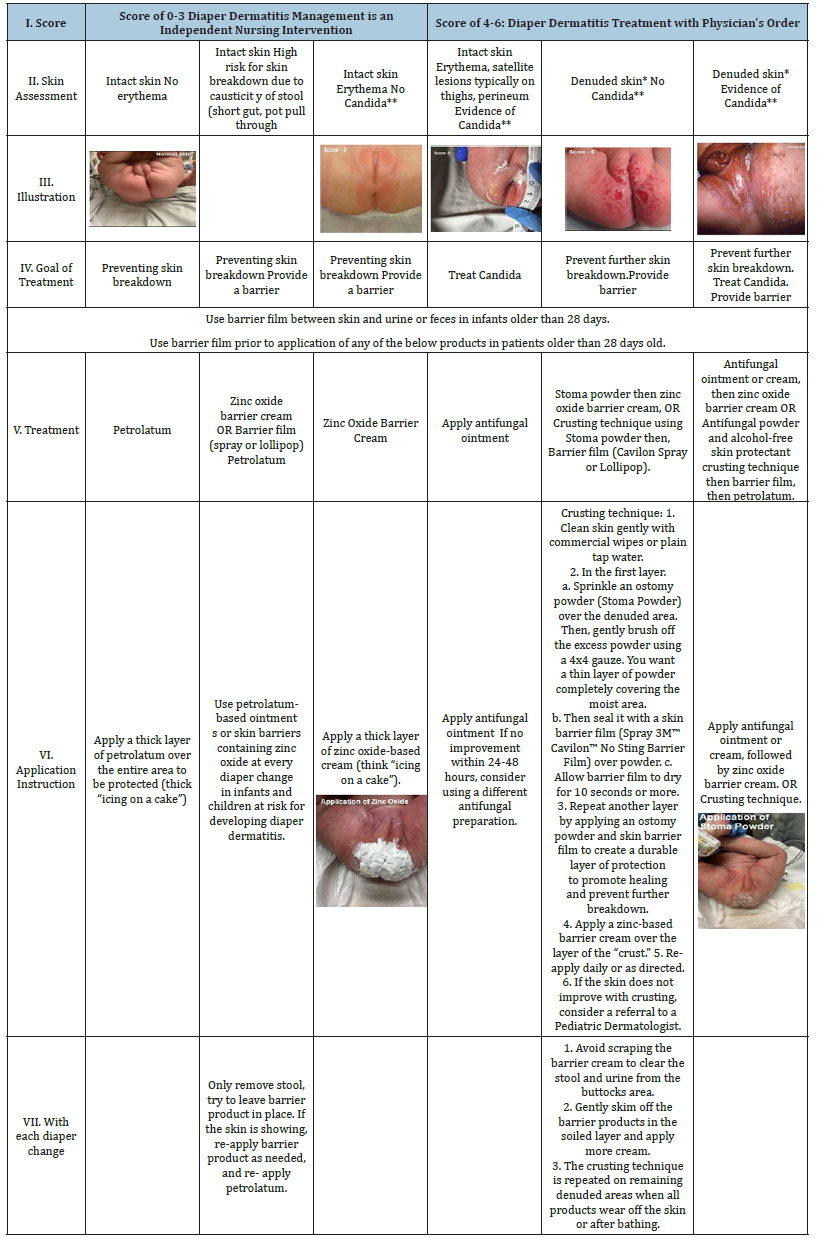
Note: Adapted from Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) Neonatal Skin Care
EBG, 4th edn. (Brandon et al. [9]).
*Denuded skin: Skin that is moist, open, and has oozing ulceration.
**Candida infections: Beefy red skin with oval/dotty lesions scattered at edges (satellite lesions), usually involve skin
folds, skin may or may not be denuded [9].
Developed by: Evidence-based Diaper Dermatitis Working Group 2022 / KSUMC-KKUH
Consultation and Referral
Referral to a pediatric dermatologist is warranted for atypical presentations or cases unresponsive to first-line management. Skin biopsy may be indicated to exclude alternative or coexisting dermatological conditions. Establishing a timely referral system enhances patient outcomes and prevents unnecessary progression of skin damage.
Nursing Competence and Documentation
Figure 1:Algorithm of diaper dermatitis care. Developed by: Evidence-based Diaper Dermatitis Working Group 2022 /KSUMC-KKUH
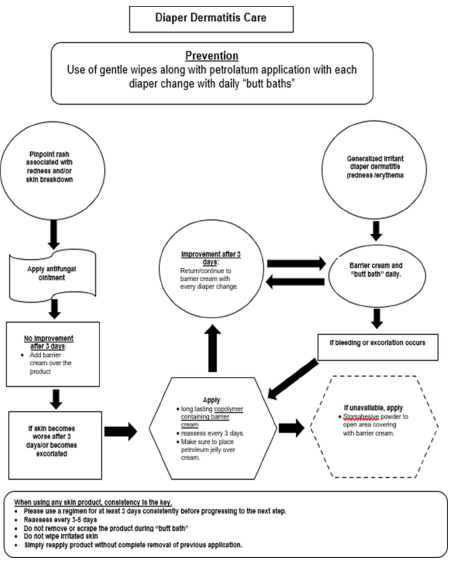
The successful implementation of EBP protocols depends heavily on the competence and adherence of staff nurses to standardized algorithms, as shown in Figure 1. Nurses must demonstrate proficiency in managing DD by completing competency assessments and maintaining up-to-date knowledge of institutional protocols and procedures. Accurate documentation within electronic systems, such as the Esihi System, ensures continuity of care and facilitates quality monitoring. Moreover, nurses serve as EBP resource persons, contributing to a reduction in the incidence of DD and an increase in compliance with practice protocols.
Caregiver Education
Family and caregiver engagement is essential in sustaining preventive strategies. Providing caregivers with brochures and educational materials empowers them with the knowledge to implement proper diapering and hygiene practices at home. Such education reinforces the healthcare team’s efforts, creating a collaborative approach to preventing and managing DD. This new DD nursing protocol emphasizes the importance of prevention, early risk identification, and consistent nursing care in managing diaper dermatitis. By integrating systematic assessment tools, individualized treatment plans, timely referrals, and robust caregiver education, healthcare providers can significantly reduce the burden of DD, improving both infant comfort and overall quality of care.
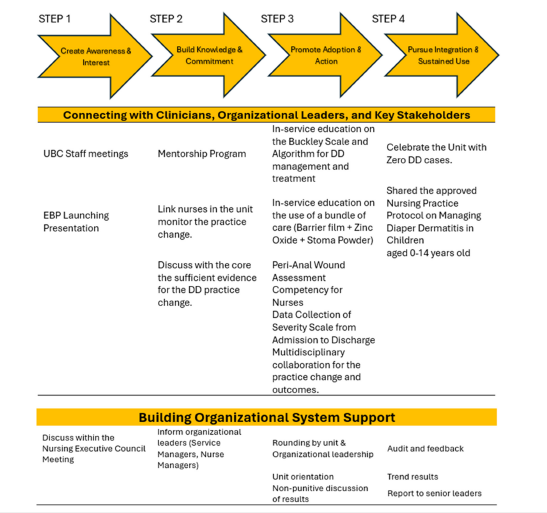
Implementation Strategies
The EBP team applied the four steps of the Iowa Model implementation strategies for practice change, as shown in Figure 2. These strategies were mentored by an international subject matter expert, ensuring the effectiveness of care and management for newborn skincare.
Figure 2:Implementation strategy for evidence-based diaper dermatitis care and management (IOWA MODEL).
Evaluation
This EBP initiative measures both processes and outcomes to ensure practice changes are adopted. The team adapted the EBP Evaluation Framework to evaluate the EBP practice and local data for informed decision-making [8]. This framework evaluates the Process (Nurses’ knowledge and attitude) during the pilot period. The goal of evaluating the process is to identify the clinician’s training needs and guide the implementation of new practice recommendations.
A convenience sample of pediatric nurses (n=269) was surveyed before the pilot implementation of the skin care bundle. Participation was voluntary, and the identifiers were not tracked, so individual follow-up was not possible. Most respondents scored highly on understanding the definition of DD, contributing factors, the total Buckley score, the ABCDE practical approach, the best patient position, the patient consent protocol, the Buckley Scale Assessment Tool, the optimal measurement method, and the frequency of assessing infants with DD. However, the study revealed that among the 269 pediatric nurses who participated, many (19.7%) were not competent in determining the highest score for severe skin irritation using the Buckley Assessment tool. In contrast to Buckley’s study, Buckley et al. [7] found that the newly developed scale is user-friendly, reliable, and effective for evaluating overall DD severity and detecting variations in severity. The EBP process is iterative, adaptable, and context-specific, allowing ample time for improvement. It must also be flexible enough to adapt to real-world settings.
Accordingly, using a four-point Likert scale, the team assessed nurses’ perceptions and attitudes toward DD care. The results showed that nurses’ perceptions and attitudes across different variables led to about half of the respondents documenting the Buckley scale assessment every shift (47%), reporting every nappy change (52%), following treatment and prevention goals (47%), using gentle wipes and applying petrolatum (48%), providing education for caregivers and family (57%), managing dermatitis with algorithms (49%), utilizing referral systems (46%), and managing dermatitis independently (52%).
Despite published evidence showing the benefits of using certain over-the-counter products, such as herbal and traditional medicines, as complementary treatment for DD, there remains a lack of substantial evidence to support strong recommendations [13,14]. Likewise, an ongoing study explores DD-associated factors in low- and middle-income countries [15].
Patient evaluation
The EBP team assesses the initiative’s success by measuring its impact on patient care through the daily census of admitted patients. This includes information on the origin of DD, a visual evaluation of the affected area, and a Buckley score assessment conducted both before and after implementing the skin care bundle. The data collection process lasted over three years to ensure lasting practice change [16-18].
Accordingly, document review was performed from October 2021 to August 2024 to evaluate the effectiveness of implementing the skin care bundle. A descriptive analysis was used through Microsoft Excel and stored on the organization’s research computer, which is password-protected. This Excel file compiled data on admitted cases of 0-14-year-olds with diaper dermatitis. It records the Buckley Scale Score (both before and after intervention), the total number of days of intervention, and the reason for discontinuing the intervention. It analyses descriptive statistics, including case frequency, percentage, and the mean. The results showed that among the 88 DD patients, 49% were home-acquired, while 51% were hospital-acquired. Ninety-six percent of cases involved the diapering area, while four percent affected the perianal area. Implementing the skin care bundle over three years resulted in a reduction in the severity scores of diaper dermatitis patients from three to zero across pediatric units within four days of intervention.
Next Steps
The results demonstrated a consistent effort by pediatric nurses to achieve desirable patient outcomes over three years. Some recommendations to sustain the EBP change include (1) Every two-year reassessment of nurses’ competencies, (2) staff education whenever new pediatric nurses join the unit, and (3) establishing case monitoring in the pediatric department. (4) Informatic support is needed to incorporate the adopted Buckley Scale for Assessing the Severity of Diaper Dermatitis into the electronic health record. (5) The evidence-based practice protocol must be followed for every admitted pediatric patient with diaper dermatitis across the pediatric department. (6) Nursing administration must ensure the availability of the skin care products for treating diaper dermatitis.
Conclusion
In summary, this evidence-based practice initiative was well executed, resulting in enhanced practice change among pediatric nurses. The DD team recognized that the new DD nursing protocol highlights the importance of prevention, early risk identification, and continuous nursing care in managing diaper dermatitis, which must be integrated and maintained throughout the pediatric units of the studied institution. Consequently, it substantially alleviates the strain of DD, enhancing both infant comfort and the overall quality of care.
Acknowledgment
Acknowledgment is given to the following nurses who contributed to various steps of this evidence-based practice initiative such as Marwa Al Satary, MSN, RN; Walaa Nafea, BSN RN; Munirah Yousef Al Abdurahman, BSN, RN; Shroog Nasser Al Dosari, BSN, RN; Areej Saeed Al Yamani, BSN, RN; Heidi F. Absulio, BSN, RN; and Reem Khaled Al Mutairi, BSN, RN.
The authors thank the Nursing Department of Prince Sultan Cardiac Center, the Deanship of Scientific Research of Shaqra University, and the Corporate Nursing Affairs of King Saud University Medical City, Riyadh, Kingdom of Saudi Arabia, for supporting this work.
Moreso, authors would like to recognize Dr. Ma. Ana Flor Pascua and Dr. Millie Obra for presenting the success story of this EBP initiative at the 32nd National Evidence-Based Practice Conference at the University of Iowa, USA last April 16-17, 2025.
Conflicts of Interest
The authors declare no conflict of interest in this evidencebased practice initiative.
References
- Carr AN, DeWitt T, Cork MJ, Eichenfield LF, Fölster-Holst R, et al. (2020) Diaper dermatitis prevalence and severity: Global perspective on the impact of caregiver behavior. Pediatric Dermatology 37(1): 130-136.
- Taha M, Alsohabi E, AlRufaydi N, Alesse S, Almaqadi F, et al. (2024) Public awareness, prevalence, and risk factors of diaper dermatitis among infants in Al- Qunfudhah governorate, Saudi Arabia. International Journal of Medicine in Developing Countries 8(2): 810-818.
- Burdall O, Willgress L, Goad N (2019) Neonatal skin care: Developments in care to maintain neonatal barrier function and prevention of diaper dermatitis. Pediatric Dermatology 36(1): 31-35.
- Wilborn D, Amin R, Kottner J, Blume-Peytavi U (2023) Skin care in neonates and infants: A Scoping Review. Skin Pharmacology and Physiology 36(2): 51-66.
- Rahma A, Lane ME (2022) Skin barrier function in infants: Update and outlook. Pharmaceutics 14(2): 433.
- Esser MS, Ngui EM, Johnson TS (2021) Contributing factors to diaper dermatitis and NICU length of stay. Journal of Neonatal Nursing 27(5): 358-364.
- Buckley BS, Mantaring JB, Dofitas RB, Lapitan MC, Monteagudo A (2016) A new scale for assessing the severity of uncomplicated diaper dermatitis in infants: Development and validation. Pediatric Dermatology 33(6): 632-639.
- Cullen L, Hanrahan K, Farrington M, Tucker S, Edmonds S (2022) Evidence-based practice in action: Comprehensive strategies, tools, and tips from University of Iowa Hospitals & Clinics. (2nd edn), Sigma Theta Tau International, Indiana, USA.
- Brandon D, Hill CM, Heimall L, Lund CH, Kuller J, et al. (2018) Neonatal skin care: Evidence-based clinical practice guideline. (4th edn), Association of Women’s Health, Obstetric and Neonatal Nurses, Washington DC, USA.
- McMahon PJ, Barron SA, Jolanda van Zuuren (2018) Diaper dermatitis. DynaMed, Columbia, USA.
- Novitasari PD, Wanda D (2021) Evidence-based nursing intervention to reduce skin integrity impairment in children with diaper dermatitis: A systematic review. Pediatr Med Chir 43(s1): 21-27.
- AGREE Next Steps Consortium (2022) AGREE II instrument.
- Alsatari ES, AlSheyab N, D’Sa JL, Gharaibeh H, Eid S, et al. (2023) Effects of argan spinosa oil in the treatment of diaper dermatitis in infants and toddlers: A quasi-experimental study. Journal of Taibah University Medical Sciences 18(6): 1288-1298.
- Sharifi-Heris Z, Amiri Farahani L, Hasanpoor-Azghadi SB (2018) A review study of diaper rash dermatitis treatments. Journal of Client-Centered Nursing Care 4(1): 1-12.
- Negera A, Sento M, Dereje D, Firdisa G, Negera S, et al. (2025) Diaper dermatitis and associated factors among children aged 0-24 months in low-and middle-income countries: A systematic review protocol. PLoS One 20(1): e0313923.
- Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, et al. (2010) AGREE II: Advancing guideline development, reporting and evaluation in health care. CMAJ 182(18): E839-E842.
- Buckwalter KC, Cullen L, Hanrahan K, Kleiber C, McCarthy AM, et al. (2017) Iowa model of evidence-based practice: Revisions and validation. Worldviews on Evidence-Based Nursing 14(3): 175-182.
- Melnyk BM, Fineout-Overholt E (2023) Evidence-based practice in nursing and healthcare: A guide to best practice. (5th edn), Wolters Kluwer, Alphen aan den Rijn, Netherlands.
© 2025 Millie Obra. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






