- Submissions

Full Text
COJ Nursing & Healthcare
Literature Review: Admission Rates for Patients Over 50 with Congestive Heart Failure
Laura Cline, DNP, FNP-BC, CPNP, RN*
MGH Institute of Health Professions, USA
*Corresponding author: Laura Cline, DNP, FNP-BC, CPNP, RN, MGH Institute of Health Professions, USA
Submission: May 24, 2025;Published: August 11, 2025

ISSN: 2577-2007Volume9 Issue 4
Abstract
Congestive Heart Failure (CHF) remains a leading cause of hospital admissions and readmission among adults aged >50 years worldwide. This literature review examines trends in CHF-related hospitalizations from 2019 to 2024, highlighting disparities and global variations in outcomes. CHF affects an estimated 64 million people and imposes a significant burden on healthcare systems and patient quality of life. U.S. data indicate persistently high readmission rates despite declining initial hospitalizations, with Socioeconomic Status (SES), comorbidities, and racial disparities playing major roles. Internationally, 30-day readmission rates vary widely, ranging from 1.5% to 27.6%, underscoring inconsistencies in access to care, its delivery, and post-discharge follow-up. Studies have highlighted the underuse of Guideline-Directed Medical Therapy (GDMT), particularly among patients with lower SES, and revealed differences in adherence to treatment protocols across regions. Key themes include the importance of standardized treatment approaches, early intervention, and the integration of patient-centered strategies, such as regular symptom monitoring and enhanced transitional care. Health-related quality of life (HRQoL) in patients with CHF is significantly affected by physical, emotional, and social factors and correlates with mortality risk. The literature underscores a strong association between poor HRQoL and adverse outcomes, particularly in underserved populations. Recommendations include the implementation of integrated care models, targeted interventions to reduce disparities, and the promotion of telehealth and education to support self-management of CHF. This review supports urgent calls for global collaboration to improve CHF care and equity-focused policies. Addressing both clinical and social determinants is essential for reducing admission rates and enhancing outcomes in older adults living with CHF.
Keywords:Congestive Heart Failure (CHF); Older adults; Hospital admission; Readmission; Disparities; Nursing implications
Introduction
Congestive Heart Failure (CHF) remains a major global health concern, affecting approximately 64 million individuals and contributing significantly to hospitalizations and healthcare costs, especially among adults over 50 years of age [1]. Defined by impaired cardiac output and often classified by ejection fraction metrics, CHF results in frequent hospital admissions due to exacerbations and comorbidities, especially in aging populations [2].
Socioeconomic and geographic disparities in CHF outcomes remain stark, particularly regarding hospital readmission rates. Although improvements in Guideline-Directed Medical Therapy (GDMT) have reduced initial hospitalizations, 30-day readmissions remain high, especially among patients with limited access to care [3]. Global data indicate that readmission rates range from 1.5% to 27.6%, demonstrating significant variability based on regional health systems and access to care [4].
Given these disparities and ongoing readmission rates, further exploration of contributing factors and potential interventions is warranted. This literature review examines global and U.S.-based trends in CHF admissions and readmissions between 2019 and 2024, with a focus on disparities, quality of life implications, and evidence-based recommendations for reducing avoidable hospital use.
Methods
Search strategy
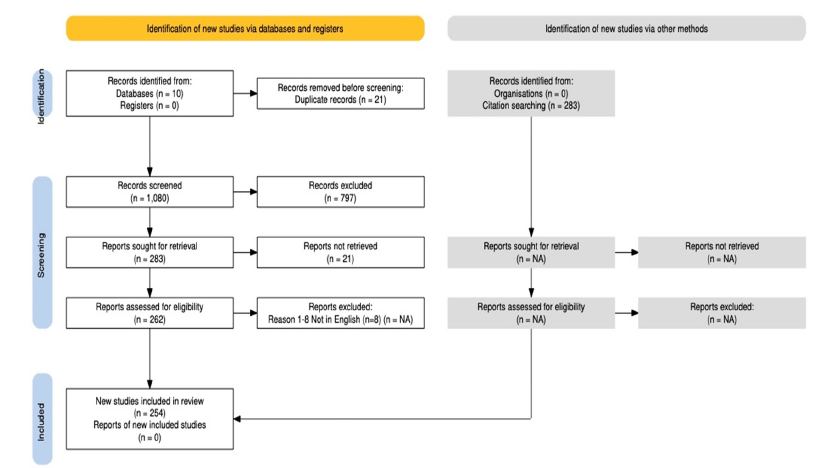
The search for current 2019-2024 peer-reviewed articles was conducted at the MGB Treadwell Library. The databases used were Academic OneFile, CINAHL Complete, Cochrane Library with Systematic Reviews, Gale OneFile, General OneFile, JSTOR, MEDLINE, Nursing Reference Center PLUS, and PubMed. Google Scholar was used to locate open-access articles. The following search terms were used to find articles specific to this study: congestive heart failure OR CHF, heart failure OR HF, ages 50+, adults, admission rates, and readmission rates. Variations in these terms were used to ensure exhaustive search results. This comprehensive literature review examines scholarly, peer-reviewed articles from 2019 to 2024 to assess trends in hospital admission rates for adults aged 50 years and older in the United States and globally. Please see Figure 1 for a Prisma Diagram.
Fgure 1:Prisma diagram.
Background
Admission rates in the United States
Among older individuals in the United States, CHF is the leading cause of hospital admissions. A study completed by the CDC between 1995 and 2009 monitored individuals aged 65 years and older and found that preventable hospital admission rates were 75% higher in this age group, while simultaneously observing significant racial disparities, particularly for black individuals compared to white individuals. Medicare was the primary payer for many hospitalizations for CHF in the United States. The rates of hospital readmission within 30 days in the United States have remained high owing to multiple factors, including the Patient’s Socioeconomic Status (SES) and comorbid health conditions. Improved disease management strategies, leading to better patient health outcomes, should be implemented to prevent the worsening of CHF and reduce hospital readmission rates.
Tsao et al. [3] provided an in-depth analysis of trends in hospitalizations and readmission rates related to HF in the United States over recent years. This study addresses the changing landscape of HF management and its implications for healthcare systems, highlighting the key factors influencing these trends and potential areas for intervention. The authors begin by discussing the overall burden of HF in the U.S., noting that it remains a leading cause of hospitalization among older adults. They emphasized that HF hospitalizations contribute significantly to healthcare costs and are associated with high morbidity and mortality rates. The study uses data from large national databases to analyze trends over time, providing a comprehensive overview of HF-related hospitalizations and readmissions.
One of the key findings of Tsao et al. [3] was the observation of a decreasing trend in hospitalizations related to HF over the study period. The authors attributed this decline to improvements in HF management, including better adherence to Guideline-Directed Medical Therapy (GDMT) and advances in medical and device-based treatments. They noted that the increased use of medications such as beta-blockers, ACE inhibitors, and Mineralocorticoid Receptor Antagonists (MRAs) has played a significant role in reducing the incidence of severe HF exacerbations requiring hospitalization. Despite the decline in initial hospitalizations, the study by Tsao et al. [3] finds that readmission rates for HF remain high. Factors contributing to these high readmission rates were explored, including inadequate post-discharge care, poor patient adherence to treatment regimens, and the presence of comorbid conditions, such as diabetes and chronic kidney disease. The authors highlighted the need for improved transitional care strategies and enhanced patient education to address these issues.
Global admission rates
Globally, the burden of CHF, along with its associated hospital readmission rates, presents significant challenges. A systematic review by the American College of Cardiology (ACC) analyzed data from 24 countries and found considerable variability in 30-day and 1-year readmission rates for patients with CHF. The 30-day readmission rate varied from 1.5% to 27.6%, whereas the 1-year readmission rate ranged from 14.0% to 63.0%. These variations were not consistently associated with a country’s healthcare expenditure or economic status, suggesting that other factors, including healthcare delivery and comorbidities, play a crucial role. In Europe, a study published in the European Heart Journal by Ponikowski et al. [4] highlighted similar trends, indicating that the 30-day readmission rates for patients with CHF varied significantly across countries, with some reporting rates as high as 25%. This study highlights the importance of standardized treatment protocols and enhanced patient management in reducing readmission rates.
Literature Review
Shahim et al. [1] provided a comprehensive review of the global public health burden of Heart Failure (HF), offering updated insights into its prevalence, incidence, mortality, and economic impact. This review highlights the growing concern regarding HF as a major public health issue worldwide, driven by aging populations and the increasing prevalence of risk factors such as hypertension, diabetes, and obesity. The author begins by highlighting the epidemiological trends of HF across different regions. They noted significant variations in HF prevalence and incidence, influenced by demographic, socioeconomic, and healthcare factors. High-income countries report stable or slightly decreasing HF incidence rates due to better management of cardiovascular diseases, whereas low- and middle-income countries face rising HF rates attributed to urbanization, lifestyle changes, and inadequate healthcare infrastructure. A critical aspect of this review is the discussion of the economic burden of HF. Shahim et al. [1] detailed the direct and indirect costs associated with HF, including hospitalizations, outpatient visits, medications, and loss of productivity.
The authors emphasize that HF is one of the costliest chronic conditions, with substantial financial strain on both the healthcare systems and patients. They called for more cost-effective strategies and healthcare policies to manage HF, particularly in resourcelimited settings. The review also explored the clinical outcomes and quality of life for patients with HF. Shahim et al. [1] reported that despite advances in treatment, HF remains associated with high morbidity and mortality. They discussed the impact of comorbidities such as chronic kidney disease, diabetes, and atrial fibrillation on the prognosis of patients with HF. The authors also highlighted the significant impairment in quality of life experienced by patients with HF due to symptoms such as dyspnea, fatigue, and fluid retention.
Ponikowski et al. [4] provided a detailed and insightful analysis of HF epidemiology in Europe and identified the key challenges and opportunities for improving patient care. Their review highlights the importance of ongoing research and innovation in addressing the increasing burden of HF and in enhancing patient outcomes across Europe. Ponikowski et al. [4] underscored advancements in HF management, including pharmacological and device-based treatments. They discussed the benefits of medications, such as ACE inhibitors, beta blockers, and mineralocorticoid receptor antagonists, as well as the roles of implantable cardioverterdefibrillators and cardiac resynchronization therapy. Despite these advancements, adherence to treatment guidelines varies across Europe, highlighting the need for standardized care protocols.
The 2022 American Heart Association (AHA)/American College of Cardiology (ACC)/Heart Failure Society of America (HFSA) guidelines for managing heart failure offer a comprehensive update on best practices for diagnosing, managing, and treating Heart Failure (HF). These guidelines, formulated by the ACC, AHA, and HFSA, integrate the latest evidence-based recommendations to improve patient outcomes and standardize care across healthcare settings. These guidelines emphasize a patient-centered approach to CHF management, acknowledging the complexity of CHF and the necessity for individualized treatment plans. Key components include early and accurate diagnosis, facilitated by advancements in imaging techniques and biomarkers such as B-type Natriuretic Peptide (BNP) and N-Terminal Pro-B-type Natriuretic Peptide (NTpro- BNP). These biomarkers aid in the differentiation from other conditions with similar clinical presentations.
A critical update in the 2022 guidelines is the classification of CHF into distinct categories based on ejection fraction: Heart Failure with Reduced Ejection Fraction (HFrEF), Heart Failure with Mildly Reduced Ejection Fraction (HFmrEF), and Heart Failure with Preserved Ejection Fraction (HFpEF). This categorization allows for more tailored therapeutic strategies. The guidelines also introduce a new category, Heart Failure with Improved Ejection Fraction (HFiEF), which recognizes patients who exhibit a significant improvement in ejection fraction following treatment. These guidelines provide a detailed overview of pharmacological treatments, with a focus on Guideline-Directed Medical Therapy (GDMT). This includes the continued use of established medications such as Angiotensin-Converting Enzyme Inhibitors (ACEIs), Angiotensin II Receptor Blockers (ARBs), beta-blockers, and Mineralocorticoid Receptor Antagonists (MRAs). Additionally, the guidelines highlight the benefits of newer agents, such as sodiumglucose cotransporter-2 (SGLT2) inhibitors, which have shown promising results in reducing HF hospitalizations and mortality in patients with HFrEF and HFpEF.
Non-pharmacological interventions have been extensively investigated. These include lifestyle modifications such as sodium restriction, weight management, and physical activity. The guidelines underscore the importance of patient education and self-management and recommend multidisciplinary care teams to support patients in managing their condition effectively. Device therapy and surgical interventions were addressed, with recommendations for using Implantable Cardioverter- Defibrillators (ICDs) and Cardiac Resynchronization Therapy (CRT) in appropriate patients. These guidelines also discuss the role of mechanical circulatory support and heart transplantation in patients with advanced HF. Moreover, the guidelines emphasize the need for regular follow-up and monitoring to adjust treatment plans as needed and to detect and manage comorbidities, such as diabetes, hypertension, and renal dysfunction. The integration of telehealth and remote monitoring technologies is encouraged to enhance patient care and adherence to treatment plans.
Health-related quality of life in heart failure
HRQoL is crucial in HF management, as it reflects the disease’s impact on physical, emotional, and social well-being. The Global CHF (G-CHF) study employed standardized questionnaires to assess HRQoL, revealing several key aspects, including physical limitations, emotional and psychological impact, and social factors. Patients with HF experience significant physical impairments, leading to reduced HRQoL scores. There is a high prevalence of depression and anxiety among patients with HF, which leads to a further decrease in HRQoL. Many patients have reported social isolation and diminished roles in social activities owing to HF symptoms. This study highlighted significant differences in HRQoL and mortality across regions, including disparities in healthcare access, quality, and socioeconomic status. Countries with better healthcare systems have reported higher HRQoL and lower mortality rates. Lower-income patients faced greater challenges in managing HF, leading to a poorer HRQoL and higher mortality. The G-CHF study identified a strong link between poor HRQoL and increased mortality in HF patients. Key findings included the predictive value (lower HRQoL scores were associated with a higher mortality risk) and independent risk factors (HRQoL was an independent predictor of mortality beyond traditional clinical measures, such as ejection fraction, age, and comorbidities).
Trends and disparities in heart failure burden
A significant focus of this review is the disparities in HF care and outcomes. Shahim et al. [1] identified gaps in access to care, diagnostic services, and advanced therapies between high- and low-income regions. They argue that these disparities contribute to the worse outcomes observed in low and middle-income countries. The authors advocate global initiatives to improve access to HF care, including the development of affordable treatment options and strengthening healthcare systems. The authors also addressed the role of preventive measures in reducing the global HF burden. They emphasized the importance of controlling risk factors through public health interventions, such as promoting healthy diets, increasing physical activity, and implementing smoking cessation programs. Shahim et al. [1] called for integrated care models that involve primary care providers, cardiologists, and other healthcare professionals in the early detection and management of HF.
Tsao et al. [3] also examined the demographic disparities in HF-related hospitalizations and readmissions. Tsao et al. [3] reported that specific populations, including older adults, racial and ethnic minorities, and individuals with lower socioeconomic status, are disproportionately affected by HF hospitalizations and have higher readmission rates. The authors called for targeted interventions to address these disparities, such as culturally tailored education programs and increased access to outpatient care for vulnerable populations. In addition to demographic factors, the authors discussed the impact of healthcare system factors on HF hospitalization and readmission trends. They highlighted the role of hospital quality metrics and financial incentives in improving HF care. For instance, the implementation of the Hospital Readmissions Reduction Program (HRRP) by the Centers for Medicare & Medicaid Services (CMS) has increased the focus on reducing readmissions through improved discharge planning and follow-up care.
A significant focus of the review is on the disparities in access to Guideline-Directed Medical Therapy (GDMT) and advanced HF treatments. Shah et al. [5] demonstrated that patients with lower SES are less likely to receive evidence-based medications such as beta-blockers, ACE inhibitors, and MRAs. They are also less likely to undergo advanced procedures such as Cardiac Resynchronization Therapy (CRT) and Implantation of Cardioverter-Defibrillators (ICDs). The authors attributed these disparities to financial constraints, lack of health insurance, and differences in healthcare provider practices. The study also examined the role of healthcare systems in perpetuating or mitigating these disparities. Shah et al. [5] argued that healthcare policies and institutional practices have a significant impact on the equitable distribution of HF care. They discuss how systemic biases and structural barriers within healthcare systems can disadvantage patients with lower SES, leading to suboptimal care and worse outcomes.
Another critical aspect discussed was the intersectionality of socioeconomic factors with race and ethnicity. Racial and ethnic minorities, who often belong to lower SES groups, face compounded barriers to accessing HF care. Culturally competent care models that address the unique needs of these populations are needed. Targeted interventions are needed to reduce the socioeconomic disparities in HF care. Advocating for policy changes to improve access to health insurance and reduce financial barriers to care is necessary. Community-based initiatives should be developed to enhance health literacy and support self-management among patients of lower SES. Emphasis should be placed on the importance of training healthcare providers to recognize and address socioeconomic factors in clinical practice.
Jones et al. [6] conducted a systematic review and meta-analysis to assess the survival of patients with CHF in a community setting. This study compiled data from various cohorts to evaluate survival rates, identify prognostic factors, and compare outcomes across different patient populations. The Global Congestive Heart Failure (G-CHF) study analyzed data from 23,000 patients with HF from 40 countries. The primary objectives were to evaluate HRQoL and its relationship with mortality, taking into account demographic, comorbid, and healthcare variations. This meta-analysis revealed a wide range of survival rates, reflecting the heterogeneity of CHF populations and healthcare contexts. The median survival times varied significantly, underscoring the complex nature of CHF management in the community. This study highlights improvements in survival over time, likely due to advancements in the treatment and management of CHF. Jones et al. [6] identified several vital prognostic factors that influence survival in patients with CHF, including age, sex, comorbid health conditions, and clinical indicators. Older age and male sex were associated with poorer survival outcomes. The presence of comorbid conditions such as diabetes and chronic kidney disease significantly affects survival rates. The ejection fraction and New York Heart Association (NYHA) classification were significant predictors of mortality. Patients managed in specialized heart failure clinics generally had better survival rates than those receiving standard primary care, highlighting the benefits of specialized care.
Recent literature has emphasized the importance of addressing disparities in CHF care. For example, one study highlighted that socioeconomic disparities significantly impact hospitalization rates for CHF. The research pointed out that patients from lower socioeconomic backgrounds are more likely to experience higher readmission rates owing to factors such as limited access to healthcare resources and suboptimal disease management. Another critical aspect is the sex disparity in CHF hospitalizations. Women, particularly older women, have been reported to have higher rates of preventable hospitalizations than men. This finding suggests a need for targeted interventions to address sex-specific factors in CHF management. The presence of other chronic illnesses exacerbates the severity of CHF, leading to higher admission and readmission rates among patients with multiple comorbidities. Additionally, patients with CHF monitoring, starting immediately after discharge, are less likely to have a readmission due to a CHF flare within 30 days of discharge from the hospital. Effective management strategies can reduce hospitalization rates, including enhanced patient education regarding CHF, regular monitoring visits, and appropriate medical therapy.
Discussion
This review confirms that CHF readmission remains a significant burden, particularly for older adults and socioeconomically disadvantaged populations. While guideline-directed therapies have improved outcomes in some cohorts, their inconsistent implementation contributes to persistent disparities [5]. The need for equitable access to GDMT and transitional care services is evident. The reviewed literature supports the use of integrated care models, including early follow-up and multidisciplinary teams, as effective strategies for reducing readmissions and improving patient-reported outcomes [7]. Innovations such as remote monitoring and telehealth are especially promising for underserved populations [8]. Findings from the Global CHF study emphasize that health-related quality of life (HRQoL) is not only a consequence of CHF but also a predictor of mortality, highlighting the importance of holistic care models that address physical, emotional, and social needs [6]. Tailoring interventions to these domains may help mitigate both acute events and long-term risks [9-15].
Conclusion
This literature review highlights the persistent challenges associated with CHF hospital admissions and readmissions, particularly among patients aged 50 years or older. Despite clinical advancements, disparities linked to race, socioeconomic status, and geographic location remain substantial barriers to optimal outcomes. Key findings include the underutilization of GDMT in lowresource populations, the predictive value of HRQoL for mortality, and the effectiveness of integrated care models. Future efforts should focus on expanding access to evidence-based interventions, enhancing care transitions, and addressing social determinants of health to reduce avoidable hospitalizations.
References
- Shahim B, Kapelios CJ, Savarese G, Lund LH (2023) Global public health burden of heart failure: An updated review. Card Fail Rev 9: e11.
- Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, et al. (2022) 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145(18): e895-e1032.
- Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, et al. (2020) Trends in heart failure-related hospitalization and readmission rates in the United States. Journal of the American Heart Association 9(8): e014547.
- Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, et al. (2020) Heart failure epidemiology: A European perspective. European Heart Journal 41(12): 1128-1140.
- Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, et al. (2019) Socioeconomicic disparities in heart failure care. Circulation 139(10): 1234-1245.
- Jones NR, Roalfe AK, Adoki I, Hobbs FDR, Taylor CJ (2019) Survival of patients with chronic heart failure in the community: A systematic review and meta-analysis. European Journal of Heart Failure 21(11): 1306-1325.
- Saxena FE, Bierman AS, Glazier RH, Angaran P, Thavendiranathan P (2022) Association of early physician follow-up with readmission among patients hospitalized for acute myocardial infarction, congestive heart failure, or chronic obstructive pulmonary disease. JAMA Network Open 5(7): e2222056-e2222056.
- Reid P, Kandasamy V, Chambers B, Panarelli M (2021) 58 The benefits of a virtual ward model in the management of care of elderly patients admitted with decompensated heart failure. Age and Ageing, 50(Supplement 1): i12-i42.
- Johansson I, Joseph P, Balasubramanian K, McMurray JJV, Lund LH, et al. (2021) Health-related quality of life and mortality in heart failure: The global congestive heart failure study of 23,000 patients from 40 countries. Circulation 143(22): 2129-2142.
- Will JC, Valderrama AL, Yoon PW (2022) Preventable hospitalizations for congestive heart failure: Establishing a baseline to monitor trends and disparities. Prev Chronic Dis 9: E85.
- Editorial Manager. Journal of Cardiovascular Nursing.
- Goyal P, Norton C, Verma A, Patel A, Ziaeian B (2020) Gender disparities in heart failure: A review of current literature. Journal of Cardiology 75(3): 212-219.
- Nair R, Lak H, Hasan S, Gunasekaran D, Babar A, et al. (2020) Reducing all-cause 30-day hospital readmissions for patients presenting with acute heart failure exacerbations: A quality improvement initiative. Cureus 12(3): e7420.
- Monday LM, Sebastian J, Nguyen P, Yazdanpanah O, Solokowski C, et al. (2022) A resident-driven quality improvement project to increase primary care follow-up after congestive heart failure exacerbation: Use of a quality and safety award. Am J Med Qual 37(4): 314-320.
- Weeks K, Kile D, Garber J (2020) Implementing a nurse discharge navigator: Reducing 30-day readmissions for heart failure and sepsis populations. Professional Case Management 25(6): 343-349.
© 2025 Laura Cline. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






