- Submissions

Full Text
Associative Journal of Health Sciences
Burn Injuries in Pregnancy - A Harmful and Challenging Association
Andrei Zbuchea1* and Cristina Zbuchea2
1Department of Plastic Surgery, District Emergency Hospital, Gageni Street No. 100, Ploiesti, Romania
2Faculty of Medicine, University of Medicine and Pharmacy, Eroii Sanitari Boulevard No. 8, Bucharest, Romania
*Corresponding author:Andrei Zbuchea, MD, PhD, Department of Plastic Surgery, District Emergency Hospital, Gageni Street No. 100, Ploiesti, Romania
Submission: October 14, 2025;Published: November 07, 2025

ISSN:2690-9707 Volume4 Issue3
Abstract
Although thermal injuries during pregnancy are uncommon, this damaging and delicate situation requires appropriate management and a multidisciplinary approach to provide optimal care for both the mother and the fetus. Systematic research was performed, and relevant data were analyzed from the literature, according to the PRISMA guidelines. This article emphasizes the importance of fetal age and burn severity in guiding therapeutic decisions and appropriate management. It also provides tables summarizing key information. The fetal survival before 28 weeks of gestation depends on the mother; however, after 32 weeks, fetal survival becomes increasingly safe, and the principle of fetal extraction is recommended for more severe burns.
Keywords: Burns; Pregnancy; Injury; Feto-maternal outcome
Highlights
a) The association of pregnancy with burn injuries is extremely challenging and requires careful management.
b) Maternal prognosis depends mainly on burn surface area, and fetal prognosis also depends on gestational
age.
c) In extensive burns, extraction of the fetus as early as possible, after 32 weeks of gestation.
Introduction
Thermal injury is one of the most serious, demanding and mutilating insults that a human being can suffer, with multiple implications at all levels (somatic, mental, emotional) and important socio-economic repercussions. Considering the special physiological status that pregnancy confers, with multiple endocrine and metabolic changes, the occurrence of a burn during pregnancy is a sudden unexpected risk and stress factor for both mother and fetus [1-3].
Thermal injury, which generally occurs at home, through flame or hot liquid, negatively
affects the natural course of pregnancy, by:
a. the initial shock with the centralization of blood circulation
b. the general post-burn reactions of the body
c. possible complications (infectious ones being the most common)
d. pain associated with burns
e. possible surgical interventions
f. the demand for vital and functional reserves of the mother
g. contraindications of some medications during pregnancy,
etc.
On the other hand, pregnancy is an aggravating factor and a criterion for the severity of burns, along with the extent of the wounds, their depth, location, association with inhalation injuries or pre-existing medical conditions [2,3]. Although rare, the association between pregnancy and burns requires special attention, hospitalization in a specialized service, and an optimal multidisciplinary approach (plastic surgery, obstetrics-gynecology, medical imaging, intensive care, neonatology, psychology etc.).
Considering these particular and aggravating aspects, which we have also encountered in our clinical practice, we investigated data from the specialized literature regarding the management of this association between burns and pregnancy, to establish some guidelines both regarding the treatment of burn injuries and the evolution of pregnancy.
We have conducted an updated systematic review, based on both personal experience and what has been published to date, on this important and challenging, life-threatening association in both pregnancy and burn management. We have also outlined some guidance on this important topic.
Material and Methods
To study the concurrent association between pregnancy and thermal injury and based on our experience, we have conducted systematic research and analyzed data from literature, according to the PRISMA guidelines [4].
The search source was PubMed, with the terms: “burns and pregnancy”, and we applied the following filters: “Abstract, English, Humans, Female”. We started the search in September 2024, with over 1400 results, but most of them had no relation to our study, such as: trauma in pregnancy, contraception, other health problems in pregnancy (thyrotoxicosis, lipid burning, hemorrhage, substance use disorders, psychosocial stress, diabetes, immersion in water during pregnancy, labor or birth, and so on). Therefore, in order not to avoid any significant article, without applying additional filters, we went through the entire list, from beginning to end, and found 43 studies related to burns in pregnancy (in fact, only 3% from over 1400). We continued by focusing on 26 of these which were included in the References, being relevant to our study in terms of epidemiology, case reports, reviews, diagnosis, therapy, prognosis, implications and recommendations.
Result
General perspective
The analysis of the specialized literature has highlighted the
particular importance of the association between pregnancy
and thermal injury, from the point of view of maternal and fetal
prognosis. It depends on the multitude of factors [5]:
a) severity of the burn, depending on the surface and depth
b) presence of associated injuries, mainly respiratory
c) gestational age of the fetus
d) presence or absence of complications.
Of all these factors, in a representative study of a group of 50 pregnant women who suffered burns [6], the only factor that proved to be statistically significant for maternal and fetal prognosis was the total surface area of the burns (p < 0.0001). Maternal and perinatal mortality increases significantly in burns above 50% TBSA (total surface area of burns), fetal mortality occurring mainly in the first days after the burn [6-8].
Maternal perspective regarding burn injury
The association between pregnancy and burns gives the burn
a severity character, due to the major physiological changes that
occur during pregnancy and that influence the evolution of the
burn, such as [9-11]:
a) alteration of immunological reactivity
b) modification of coagulation functions
c) expansion of the plasma volume
d) hyperdynamic circulatory state.
Fetal perspective
On the other hand, thermal injury has two important
repercussions on pregnancy [6]:
a) spontaneous uterine activity [12], with risk of abortion or
premature birth
b) risk of fetal intrauterine fetal death, due to centralized
circulation and compromised circulatory flow to the nonpreferential
area of the pregnant uterus and fetoplacental unit
[6,13] due to acidosis and hydroelectrolytic imbalances, as well
as the infectious load that subsequently developed.
Treatment guidelines
The treatment management of this association (between
pregnancy and burns) is complex and difficult [14,15] because
it addresses both the mother and the fetus, each with different
medical needs [16]. For the mother, the aim of the treatment is
to heal the burn, with optimal results both morphologically and
functionally. For this, therapeutic measures include [14]:
a) rapid, adequate and efficient hydroelectrolytic
resuscitation
b) infection control, through systemic antibiotic therapy and
topical antimicrobial agents
c) ensuring adequate nutritional intake
d) surgical interventions, of which early excisions followed
by skin grafting can improve maternal prognosis [6,15].
Surgical recommendation
To improve maternal and fetal prognosis, early excision of the burn wound and skin grafting, or at least late skin grafting of a granulating wound, should be performed as a priority, especially in deep burn wounds, regardless of the burn size, i.e. TBSA. Otherwise, given the altered maternal immunological status, the neglected burn wounds can develop into complications, the most dangerous being invasive infection, leading to sepsis, MODS and ultimately maternal death [16,17].
Special issue with monitoring and medication
Contrary to the needs of the mother, for the benefit of the fetus, it is necessary to avoid both anesthesia and the administration of a wide range of drugs, especially in the first trimester of pregnancy, because of fetal side effects. Also, the hydroelectrolytic resuscitation measures, the pain caused by the burn, the centralization of circulation encountered in the initial shock, with hypovolemia and hypoxia, acidosis and electrolyte imbalances, the general postcombustion reaction of the maternal body require careful maternal circulatory monitoring and compliance with optimal parameters, including urine output. Possible sepsis caused by burns can lead to fetal death, and products released from burned tissues (Prostaglandin E2) can cause spontaneous abortion or premature birth [8,9].
Because of possible decreased placental perfusion causing fetal hypoxia, elevated maternal body position and supplemental oxygen administration are recommended, even in the absence of inhalational post-burn injury [13].
Maternal and fetal prognosis depends on the extent and depth of the burns, the occurrence of complications, and the gestational age. To reduce complications and high perinatal mortality, pregnant women with extensive burns who are more than 32 weeks pregnant should deliver as soon as possible [18].
In terms of medication, spasmolytics [19], to suppress abortion or spontaneous labor [6] and to protect operations, are highly recommended, especially in patients without extensive burns, in the 2nd and 3rd trimesters of pregnancy. Dexamethasone is also indicated to allow fetal lung maturation, without affecting the maternal prognosis.
The use of tocolytics should be avoided in cases of maternal sepsis, intrauterine fetal death, or abruptio placentae. If the maternal condition is stable, progesterone can be utilized to prevent premature labor [20].
The general hypercoagulable state encountered during pregnancy is further increased in burn injuries, which activate the coagulation systems through the release of cytokines, and the risk of thrombosis is further increased in an uncorrected hypovolemic state. The hypercoagulable state, with the risk of thrombosis, conferred by both pregnancy and burn injuries, can be corrected by routine prophylactic administration of intravenous heparin, at an initial dose of 2U/kg per hour, monitored and subsequently corrected by partial thromboplastin time [13], to prevent coagulation and inflammation, to restore the normal blood flow, and to promote healing [20].
Also, the hypermetabolic state developed in pregnancy is further increased in associated burns, especially in severe burns, which cause very high metabolic stress. Intensive and balanced nutritional support contributes to wound healing, decreases aberrant immune response, restores and maintains normal gastrointestinal function. In pregnancy, an anabolic state is present, whereas in burn injuries, it is initially a contradictory catabolic state that must be switched to an anabolic state along with the wound healing and epithelization process. The enteral feeding should be started as early as possible and continued uninterrupted to maintain mucosal integrity, buffer gastric acid, and decrease susceptibility to infection. The recommended daily allowance (RDA) for a pregnant woman is normally higher than for a nonpregnant woman but is even higher when associated with burns. For pregnant women, enteral feeding of 36kcal/kg/day is recommended, along with a well-balanced diet that includes protein (essential amino acids), lipids, minerals, vitamins and fibers [20].
If the patient’s condition clearly deteriorates and serious complications occur despite appropriate treatment, then termination of pregnancy may be recommended [20], to preserve maternal life.
Burn reconstructive surgery can be performed in the initial stages, to release scar contracture in pregnant women with severe scar contractures from abdominal burns [21-23], or in rehabilitation stage, to restore the patient’s appearance and functionality, through scar excision, contracture repair, skin grafts, and even prostheses [20].
The management of burn injuries in pregnancy depends on two main factors, the severity of the burn (TBSA) and gestational age, and is illustrated in Tables 1&2 [20].
Table 1:The management of pregnancy associated with burn injuries.
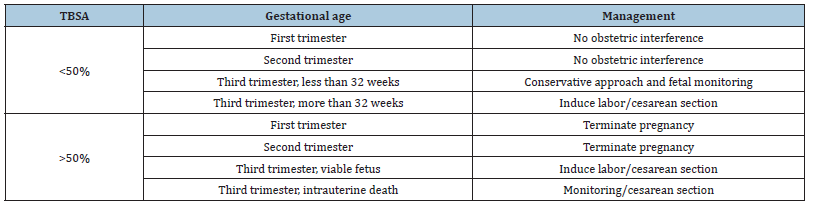
The total burn surface area represents the only factor that proved to be statistically significant for maternal and fetal prognosis, as maternal and perinatal mortality increases significantly in burns above 50% TBSA [6-8]. In the first and second trimesters, in burns over 50% TBSA, termination of pregnancy is recommended, but in the third trimester, the situation depends mainly on the viability of the fetus.
Table 2:Recommendations for the management of burn injuries in pregnancy.

Table 2 presents a list of recommendations for the management of burns in pregnancy, in the form of guiding measures.
Discussion
Burn injuries in pregnancy, although rare, cause additional stress on the maternal body, which has already been drastically altered by the presence of the fetus, and can therefore be demanding and lifethreatening for both mother and fetus. The aim of management is to save the life of the mother and fetus. The therapeutic protocol must be well coordinated, requiring a multidisciplinary team involving plastic surgeons, intensive care, and obstetricians [24].
Medical treatment includes intensive fluid resuscitation, nutrition, oxygen therapy, thromboprophylaxis, and early and effective antibiotic therapy. Surgical treatment with early excision of deep burn wounds and skin grafting is the cornerstone of the management of pregnant women with burns, to reduce the burden of prostaglandins and cytokines released from burned tissues into the circulation and to achieve faster wound coverage and healing.
The conservative local treatment can be applied for superficial burn wounds, through wound debridement, cleansing and dressing. Silver sulfadiazine is the gold standard as antibacterial agent in burns therapy, to decrease the bacterial load and fight infection. In human pregnancy, well-controlled safety studies are missing, and its use is not recommended unless strictly necessary, particularly in the last month of pregnancy. Considering all this, a safer alternative for pregnant women are honey-based dressings, which also have the advantage of wound healing activity, in addition to their antibacterial action, as we have shown in our previously published studies.
To achieve fetal rescue, induction of labor is imperative if the pregnancy is in the third trimester to extract the fetus from the toxic environment, otherwise, tocolysis and obstetric monitoring are necessary to reach the third trimester [24].
Fetal prognosis depends on both gestational age and burn severity. If the pregnancy is up to 28 weeks determined by ultrasound, the survival of the fetus is highly dependent on that of the mother [13,16]. In this situation, tocolysis can be considered if maternal conditions allow it. It is preferable to use parenteral magnesium sulfate over β-mimetic agents because it has less vasodilator and metabolic effects [13]. In conservative treatment, continuous electronic monitoring of the fetus is recommended during the first week after burns, when there is the greatest risk of harm to the fetus, and then frequent ultrasound examinations [13,25].
The maternal prognosis is worse if the burn exceeds 50% TBSA. In the cases without severe maternal complications, maternal survival is usually accompanied by fetal survival. Burn injuries increase the risk of spontaneous abortion and of premature labor, and fetal survival depends on fetal maturity. Early obstetric intervention is indicated only in the critically ill patient, in cases where complications (hypoxia, hypotension, sepsis) threaten the life of a viable fetus. The mode of delivery should be established by obstetric considerations [26].
In extensive burns, after 32 weeks of gestation, the most urgent extraction of the fetus is generally recommended, to improve the maternal prognosis, while the fetal prognosis is not improved by timing [5,8, 12,13,15,16,19,25]. Vaginal delivery, spontaneous or induced, is possible even in the presence of perineal burns [9,19] but caesarean section is preferable. In any case, fetal survival depends mainly on the gestational age [14], thus emphasizing the importance of its correct imaging assessment.
To detect pregnancy in patients of reproductive age who have suffered burns, routine urine pregnancy tests are recommended upon admission to the hospital, even if pregnancy is not obvious [13,19,25,27]. A prospective study thus identified a percentage of 7.1% of pregnancies that were not detected during hospitalization (mostly initially undeclared, but also with menstrual irregularities), highlighted by urine pregnancy tests and then confirmed by ultrasound examination [27].
Various published studies have reported an incidence of burned women of reproductive age ranging from 0.6 to 15% [8,25,27], with an average of 7% [6], being higher in developing countries and in disadvantaged socio-economic categories.
The best attitude remains that of preventing burns during
pregnancy [6,9,14], through:
a) primary preventive measures: health education, prenatal
care, especially in lower socioeconomic categories [28,29],
avoiding the use of flammable substances and very loose
clothing during pregnancy, etc.
b) secondary measures: reducing the severity of the burn
and avoiding the deepening of the lesions, through prompt
first aid interventions (removing adherent burned clothes,
immediate cooling of the burned regions with cold water).
Conclusion and Recommendations
1. The occurrence of a burn during pregnancy requires
special attention, careful monitoring and adequate and effective
therapeutic management, for a favorable evolution of both the
mother and the fetus.
2. The therapeutic approach is complex, delicate,
individualized, multidisciplinary (plastic surgery, obstetricsgynecology,
intensive care, neonatology, psychology etc.),
considering both the needs of the mother and those of the fetus.
3. The maternal prognosis depends mainly on the surface
of the burn, and the fetal prognosis also depends on the
gestational age, therapeutic decisions being made based on
these two parameters.
4. Extraction of the fetus as early as possible, in case of
extensive burns, after 32 weeks of gestation.
5. Routine practice of pregnancy tests in hospitalization, in
the case of patients of fertile age.
6. The need to prevent thermal injury during pregnancy.
Conflict of Interest
None.
References
- Dijkerman ML, Breederveld-Walters ML, Pijpe A, Breederveld RS (2022) Management and outcome of burn injuries during pregnancy: A systematic review and presentation of a comprehensive guideline. Burns 48(7): 1544-1560.
- Parikh P, Sunesara I, Lutz E, Kolb J, Sawardecker S, et al. (2015) Burns during pregnancy: Implications for maternal-perinatal providers and guidelines for practice. Obstet Gynecol Surv 70(10): 633-643.
- Seyedzadeh MS, Rezavand N, Seyedzadeh A, Tohidi MR, Hemati M, et al. (2021) Maternal and fetal outcome of burn during pregnancy: 3rd report from Kermanshah, Iran. Int J Burns Trauma 11(2): 90-95.
- (2024) Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) - the PRISMA 2020 statement.
- Unsur V, Oztopcu C, Atalay C, Alpay E, Turhanoglu B (1996) A retrospective study of 11 pregnant women with thermal injuries. Eur J Obstet Gynecol Reprod Biol 64(1): 55-58.
- Akhtar MA, Mulawkar PM, Kulkarni HR (1994) Burns in pregnancy: Effect on maternal and fetal outcomes. Burns 20(4): 351-355.
- Polko LE, McMahon MJ (1998) Burns in pregnancy. Obstet Gynecol Surv 53(1): 50-56.
- Srivastava S, Bang R (1988) Burns during pregnancy. Burns Incl Therm Inj 14(3): 228-232.
- Mabrouk AR, El-Feky AE (1997) Burns during pregnancy: A gloomy outcome. Burns 23(7-8): 596-600.
- Akinlaja O (2016) Hematological changes in pregnancy - the preparation for intrapartum blood loss. Obstet Gynecol Int J 4(3): 95-98.
- Shi Y, Zhang X, Huang BG, Wang WK, Liu Y (2015) Severe burn injury in late pregnancy: a case report and literature review. Burns Trauma 3: 2.
- Ullmann Y, Blumenfeld Z, Hakim M, Mahoul I, Sujov P, et al. (1997) Urgent delivery, the treatment of choice in term pregnant women with extended burn injury. Burns 23(2): 157-159.
- Guo S, Greenspoon J, Kahn A (2001) Management of burn injuries during pregnancy. Burns 27(4): 394-397.
- Jain ML, Garg AK (1993) Burns with pregnancy - A review of 25 cases. Burns 19(2): 166-167.
- Benmeir P, Sagi A, Greber B, Bibi C, Hauben D, et al. (1988) Burns during pregnancy: Our experience. Burns 14(3): 233-236.
- Deitch EA, Rightmire DA, Clothier J, Blass N (1985) Management of burns in pregnant women. Surg Gynecol Obstet 161(1): 1-4.
- Prasanna M, Singh K (1996) Early burn wound excision in ‘major’ burns with ‘pregnancy’: a preliminary report. Burns 22(3): 234-237.
- Cheah SH, Sivanesaratnam V (1989) Burns in pregnancy - maternal and fetal prognosis. Aust N Z J Obstet Gynaecol 29(2): 143-145.
- Matthews RN (1982) Obstetric implications of burns in pregnancy. Br J Obstet Gynaecol 89(8): 603-609.
- Habibie PH, Kurniaputra DD (2024) Pregnancy with burn injury: A case report. J Med Pharm Chem Res 6: 1677-1682.
- Mitsukawa N, Saiga A, Satoh K (2014) Protocol of surgical indications for scar contracture release before childbirth: Women with severe abdominal scars after burn injuries. J Plast Surg Hand Surg 49(1): 32-35.
- Takeda K, Sowa Y, Numajiri T, Nishino K (2013) Expansion abdominoplasty for a pregnant woman with severe abdominal wall contracture due to a major burn during childhood: A case report. Ann Plast Surg 70(6): 643-646.
- Widgerow AD, Ford TD, Botha M (1991) Burn contracture preventing uterine expansion. Annals of Plastic Surgery 27(3): 269-271.
- Chfiri A, Karti S, Jalal A, Fikry A, Habla M, et al. (20224) Burn and pregnancy. European Journal of Medical and Health Sciences 4(2): 3-6.
- Gang RK, Bajec J, Tahboub M (1992) Management of thermal injury in pregnancy - an analysis of 16 patients. Bums 18(4): 317-320.v
- Rode H, Millar AJ, Cywes S, Bloch CE, Boes EG, et al. (1990) Thermal injury in pregnancy-the neglected tragedy. S Afr Med J 77(7): 346-348.
- Masoodi Z, Ahmad I, Yousuf S (2013) Routine use of urinary HCG test in adult burn females to detect ‘‘hidden’’ pregnancies: A review. Burns 39(4): 803-807.
- Bande BD (2020) Critically Ill Obstetric Patients and Fetomaternal Outcome. Indian J Crit Care Med 24(11): 1005-1007.
- Miglani U, Pathak AP, Laul P, Sarangi S, Gandhi S, et al. (2020) A study of clinical profile and fetomaternal outcome of obstetric patients admitted to intensive care unit: A prospective hospital-based study. Indian J Crit Care Med 24(11): 1071-1076.
© 2025 Andrei Zbuchea*. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






