- Submissions

Full Text
Open Access Research in Anatomy
Impact of Aspiration and Early Swallow Therapy in Acute Stroke Patients
Govathi Nikhila K*, Akanksha Gupta, Manish singh, Payal gupta and Arun Garg
Medanta-The Medicity Hospital, Institute of Neurosciences, India
*Corresponding author: Govathi Nikhila K, TRT 122/A, Seethaphalmandi, Secunderabad Telangana, 500061, India
Submission: September 19, 2017; Published: October 26, 2017

ISSN: 2577-1922 Volume1 Issue1
Abstract
The study focuses on role of early swallow therapy in acute stroke patients.
Materials and methods: We enrolled 112 acute stroke patients from December 2015-January 2016, among which 91 patients had swallowing difficulty as assessed on fifth day of stroke onset. Impact of type of stroke, size/site of lesion on swallowing difficulty was also assessed. All patients with base GCS-E4M6 VT/V5 were included. Swallowing scoring was done as per National Outcomes Measurements System (NOMS) 8-point Penetration Aspiration scale (PAS). The patients who had aspiration on fifth day received 30 minutes of swallowing therapy for three consecutive days. After three days of therapy swallowing was re-evaluated.
Results: Out of 112 of acute stroke patients 91 (81.25%) patients had dysphagia out of which aspiration was present in 66 (72.5%) patients in their initial swallow evaluation. We couldn’t find any significant impact of Age, Gender, and Type of stroke, Size/Site of lesion on dysphagia/Aspiration. All patients had significant swallowing improvement after therapy on NOMS 8-point PAS (P<0.001). When comparing the result from Day 5 to Day 45 follow up, we found significant improvement in patients eating solid and thickliquidsaftertherapy(p<0.001).
Conclusion: Early swallow therapy is an effective way to treat dysphagia and prevent aspiration.
Introduction
The Greek philosopher Hippocrates described the stroke phenomenon as sudden Paralysis in 400 BC. A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain either bursts, ruptures or is blocked by a clot. As a result, the brain cannot get the blood and oxygen it needs and pieces of the brain die.
Aspiration
Aspiration is defined as the inhalation of oropharyngeal or gastric contents into the larynx and lower respiratory tract. Several pulmonary syndromes may occur after aspiration, depending on the amount and nature of the aspirated material, the frequency of aspiration, and the host’s response to the aspirated material. Aspiration pneumonitis (Mendelson’s syndrome) is a chemical injury caused by the inhalation of sterile gastric contents, whereas aspiration pneumonia is an infectious process caused by the inhalation of oropharyngeal secretions that are colonized by pathogenic bacteria. Other aspiration syndromes include airway obstruction, lung abscess, exogenous lipoid pneumonia, chronic interstitial fibrosis, and Mycobacterium fortuitum pneumonia. Aspiration pneumonitis is defined as acute lung injury after the inhalation of regurgitated gastric contents. This syndrome occurs in patients who have a marked disturbance of consciousness such as that resulting from a drug overdose, seizures, a massive cerebro-vascular accident, or the use of anesthesia. Adnet and Baud demonstrated that the risk of aspiration increases with the degree of unconsciousness (as measured by the Glasgow Coma Scale). Historically, the syndrome most commonly described as aspiration pneumonitis is Mendelson’s syndrome, reported in 1946 in patients who aspirated while receiving general anesthesia during obstetrical procedures [1].
Impact of Aspiration and Risk factors of Aspiration in patients with Oro-pharyngeal Dysphagia
Dysphagia (swallowing difficulty) is a growing health concern in our aging population. Age- related changes in swallowing physiology as well as age-related diseases are predisposing factors for dysphagia in the elderly. In the US, dysphagia affects 300,000– 600,000 persons yearly. Although the exact prevalence of dysphagia across different settings is unclear, conservative estimates suggest that 15% of the elderly population is affected by dysphagia. Furthermore, according to a single study, dysphagia referral rates among the elderly in a single tertiary teaching hospital increased 20% from 2002–2007; with 70% of referrals for persons above the age of 60. The US Census Bureau indicates that in 2010, the population of persons above the age of 65 was 40 million. Taken together, this suggests that up to 6 million older adults could be considered at risk for dysphagia.
In patients with stroke, the prevalence of swallowing dysfunction ranges from 40 to 70 percent. Many of these patients have silent aspiration. Patients with dysphagia who aspirate are at an increased risk for pneumonia. Among patients who have had a stroke, pneumonia is seven times as likely to develop in those in whom aspiration can be confirmed than in those who do not aspirate [1,2]. Assessing the Risk of Oropharyngeal Aspiration Assessment of the cough and gag reflexes is an unreliable means of identifying patients at risk for aspiration. A comprehensive swallowing evaluation, supplemented by either a video fluoroscopic swallowing study or a fiber optic endoscopic evaluation, is required. A speech–language pathologist can perform this evaluation at the bedside. In patients found to be at risk for aspiration, further behavioral, dietary, and medical management to reduce this risk can be initiated. In patients with swallowing dysfunction, a soft diet should be introduced, and the patient should be taught compensatory feeding strategies (e.g., reducing the bite size, keeping the chin tucked and the head turned while eating, and swallowing repeatedly). Tube feeding is usually recommended in patients who continue to aspirate pureed food despite these strategies [1,2].
Aim & Objectives
We aimed to evaluate the Impact of Aspiration and the Role of Early swallow therapy in acute stroke patients.
Materials and Methods
From December 2015 to Jan 2016, there were 112 patients with Acute stroke were Admitted in Medanta-The Medicity Hospital. Among which, we were enrolled 91 (81.25%) patients (63-Men’s, and 28-women’s) with swallowing difficulties, who were admitted to a Neurology unit of Medanta Institute of Neurosciences Department in Medanta-the Medicity Hospital in Gurgaon. Among 91(81.25%) dysphagia patients, Aspiration was present in 66 (72.5%) and all these 91 (81.25%) dysphagia patients were divided based on their type of stroke, Size/site of lesion. All patients had stroke for the first time and visited Medanta as the primary Hospital. All of them affected with stroke at the Age of 45 years and above were reported in the study. The strokes were diagnosed by Neurologists according to clinical neurologic deficits relating to their brain damage and the findings on computed tomography or magnetic resonance imaging scans. Their swallowing disorders were impressed by the physician taking the history of choking or cough during swallowing or wet voice after conducting a 100ml water test. Furthermore, a formal swallowing condition was assessed by Speech-language therapist.
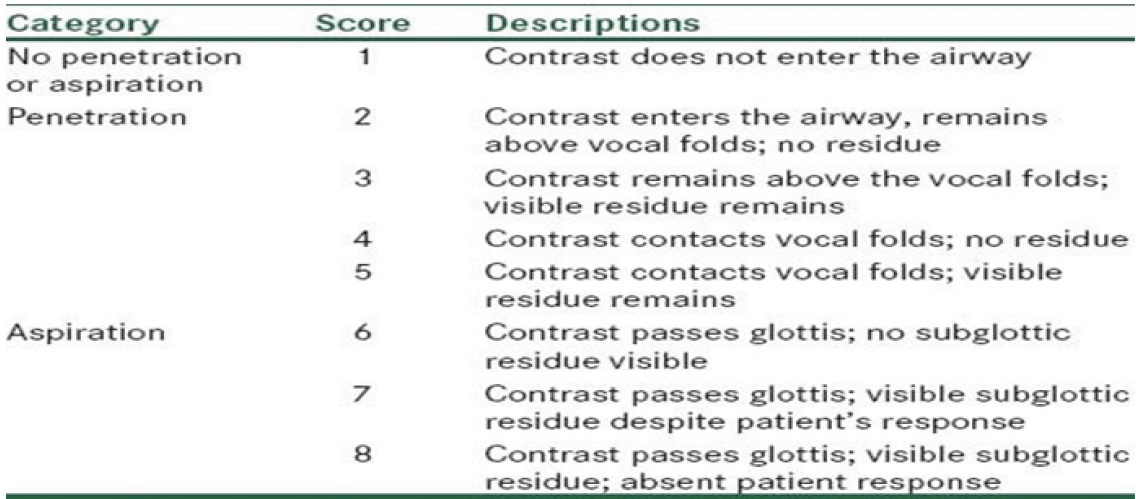
In this all patients (91(81.25%)) with dysphagia were evaluated with the initial Bedside Clinical Swallow Evaluation and ruled out with Aspiration and they are also grading with particular levels based on National Outcomes Measurements System (NOMS) from Level-1 to Level-7 and Aspiration was ruled out and severity was pointed out based on the Penetration-Aspiration 8-point rating Scale. Dysphagia patients typically began the protocol with 3ml of semi-solid (blended food) as this material afforded the best airway protection. If patient has no signs of choking or cough, the therapist would change properties of food which followed gradually according to standard guidelines. In these groups, any patient with facial weakness of facial muscles was treated with facial exercise. If the patients failed in the swallow evaluation then they will be started up with three consecutive days of swallow therapy with on and off for one or two days in a week period and again re-evaluated for the same. Later intermittently swallow evaluation is done to upgrade the (NOMS) Levels and ruled out the severity of aspiration on 8-point (PAS) to check out the functional recovery period of the patient, and also to the See the relationship between size/site of lesion and type of lesion. In addition to this the Compensatory swallow strategies are used in order to overcome the swallowing difficulties in stroke patients (Table 1,2).
Table 1: National Outcomes Measurements System (NOMS).
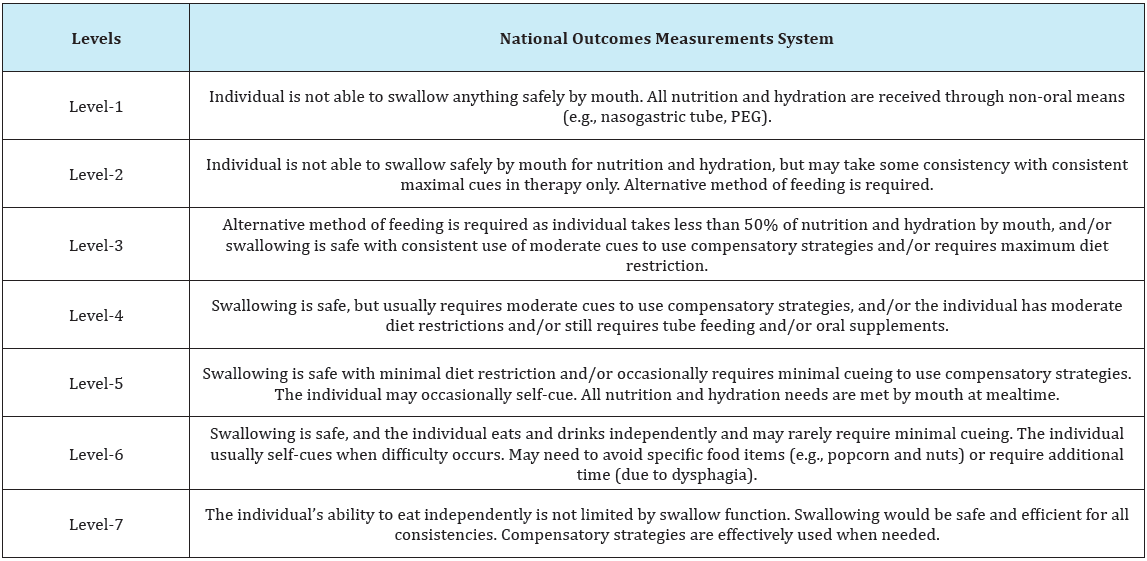
Table 2: Representing the Penetration Aspiration 8-point rating scale.
Inclusive Criteria
I. The inclusive criteria in the present study were considered as recent acute stroke patients who are visiting Medanta Hospital for primary treatment and have swallowing difficulty.
II. National outcomes Measurements system (NOMS) to rule out the severity of dysphagia in stroke patients and to grade with the particular Levels.
III. Penetration Aspiration 8-point scale to rule out the severity of Aspiration in patient with dysphagia.
IV. The patients GCS should be E4M6VT/V5 at the time of initial swallow evaluation.
V. All patients should have better cognition.
Exclusive criteria
I. Patient GCS should not be less than E4M6.
II. Impaired communication ability due to cognitivedeficit
III. Other, system in neurologic disorders leading to swallowing difficulties.
IV. Patients with oropharyngeal tumour or extensive surgeries and radiotherapy of head and neck were not involved.
V. All patients in ICU were excluded.
Procedure
a. All patients with swallowing difficulties were selected from all stroke patients and they were categorized based on their type of stroke, size/site of lesion.
b. Later all patients were underwent with initial clinical bedside swallow evaluation and the severity of dysphagia was graded based on NOMS and Aspiration was ruled out and pointing was given based on PAS. All patients who are graded with Level-1 on the NOMS and aspiration was ruled out then they were immediately started with the swallow therapy for three consecutive days with intermittent on and off in a week period.
c. The active and passive exercises were used in swallow therapy in patients who have oropharyngeal deficities and facial weakness with 30 minutes of duration period.
d. As the patient start with the oral intake the NOMS levels will upgrade regularly Aspiration severity was also checked and the compensatory strategies and swallow maneuver were also provided in order to overcome the swallow difficulty. The specific and compensatory techniques and swallowing maneuvers was based on the findings of clinical bedside swallow evaluation. These group patients were regularly evaluated with swallow test after every 2 days.
e. Later we check severity of Aspiration based on PAS and gradual functional recovery of swallowing based on the NOMS until the patient reaches to level-7 in this study.
f. Later, Day 45 follows cases and telephonic conversation was done to rule out the swallow level.
Outcome measures
The outcome measures were assessed as the changes noted with NOMS & PAS, and complications related to treatment and the swallow therapies. The functional swallowing ability and Aspiration severity of each individual was estimated using the penetration Aspiration 8-point rating scale and National Outcomes Measurement scale (NOMS) a 7 pointing rated scale reflecting the patients report of food/liquids safely ingested by mouth on a consistent basis. The scale has strong reliability and validity specific to stroke populations. Patient’s recordings of the daily diet level and method of intake (oral, non-oral, use of compensations) were determined and compared to NOMS results. Each patients report recorded the typical diet level and aspiration along with any food modifications and/ behavioural compensations used during eating. Each patient’s diet and aspiration level was documented at the onset of the therapy and again at the conclusion of the therapy and compared the scale. The duration period was calculated for each patient.
Statistical analysis
The analysis included profiling of patients on different Demo graphic, NOMS &PAS score type of stroke. The results have been presented on total number of pre-therapy NOMS & PAS scores, durational period of the therapy sessions in particular stroke type and post- therapy NOMS & PAS scores and mean changes in NOMS&PAS scores in swallow therapy between their types of stroke, size/site of lesion. The differences in the parameters were evaluated between their types, site of lesion using the independent Student t- test. Chi square test was used to test the association of gender, type of stroke. P-value <0.05 is considered statistically significant. SPSS software Version 20.0 were used for statistical analysis
Results
Graph 1: Bleed Vs Infarct
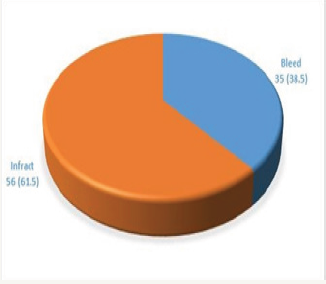
Ninety one patients with swallow difficulty were selected from 112 acute stroke patients. (Total 112/91 (81.25%)). Among these 91 dysphagia patients 66(72.5%) have Aspiration. In 91(81.25%) dysphagia patients 63 (69.2%) males and 28 (30.7%) Females were divided. Among 63(69.2%) males 48 (76.1%) have aspiration and 28 (30.8%) females 19 (67.8%) have aspiration. Later, they again divided based on their stroke type of Bleed and Infarct. In 63 (69.2%) Males there are 22 (35%) patients with bleed and among them 20 (90.9%) have aspiration and 41(65%) patients with Infarct and among them 28 (68.2%) have aspiration. In 28 (30.8%) Females there are 14 (50%) patients with bleed and among them 11 (78.57%) have aspiration and 14 (50%) patients with Infarct and among them 8 (53.3%) have aspiration with no significant difference with their age and gender factor with (0.7514>p value). Later the patients have been divided based on the Right and Left Hemispheres (RTH& LTH). There are 20 (22%) patients with RTH among which 13 (65%) have aspiration. This group again further, sub-divided with male and female ration in which there are 15 (75%) of male in which 11 (73.3%) have aspiration and there are 5 (25%) females and among them 2 (40%) have aspiration. There are 71 (78%) patients with LTH among which 53 (74.6%) have aspiration. This group again further, sub-divided with male and female ration in which there are 48 (67.6%) of male in which 37 (77%) have aspiration and there are 23 (32.3%) females and among them 16 (69.56%) have aspiration. There was no significant difference Between RTH <H in relation with their age and gender factor with (0.3211>p value). Later these 91 (100%) dysphagia patients are divided based on their stroke types Bleed and Infarct (Graph 1).
Bleed
There are 35 (38.46%) of patients with bleed among 91 (100%) dysphagia patients. In which 31 (88.57%) aspiration was noted. Later, these patients are again categorized with Left and Right Hemisphere Bleed (LTHB & RTHB). There are 20 (57.14%) patients with LTHB and 18 (51.4%) were having aspiration. Patients with Other site of lesions and severity of dysphagia and aspiration were also considered. In which there are 8 (87.5%) patients with BG Bleed and among them 7 patients are aspirating were one as not. 1(66.6%) was with cerebellar bleed and has aspiration, 3 (66.6%) patients with frontal bleed among which 2 are aspirating and the other was not.1 (100%) patient with post-parital bleed, 1 (100%) patient with frontal-temporal bleed and both were aspirating. 6 (100%) with thalamic bleed and all were aspirating. There are 15(42.85%) patients with RTHB and (40%) patients are aspirating.
A patient with other site of lesions and severity of dysphagia and aspiration was also considered. In which there are 7 (100%) patients with BG bleed and all were aspirating. 1 (100%) with IVH and 2 (100%) with thalamic bleed and both were aspirating. 3 (66.6%) with frontal bleed and among them 2 patients were aspirating. 2 (100%) patients with cerebellar bleed and both were aspirating.
Infract
There are 56 (61.53%) of patients with Infarct among 91 (100%) dysphagia patients. In which 36 (64.28%) aspiration was noted. Later, these patients are again categorized with Left and Right Hemisphere Infarct (LTHI & RTHI). There are 49 (87.5%) patients with LTHI and 36 (64.28%) were having aspiration. Patients with Other site of lesions and severity of dysphagia and aspiration were also considered. In which there are 45 (71.1%) patients with LT MCA and among them 32% of patients are aspirating were 13 (28.8%) not. 1 (66.6%) was with PICA and has aspiration, 1 (100%) patients with fronto-temporal infarct and was aspirating, 2(100%) with fronto-temporo-parietal infarct and both were aspirating. There are 7(12.5%) patients with RTHB and 5(40%) patients are aspirating were as other not.
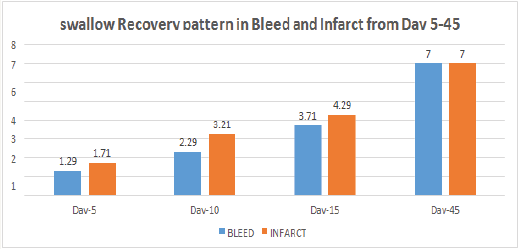
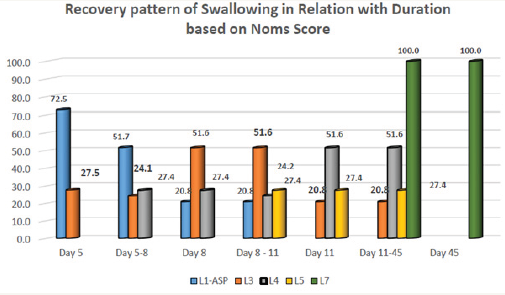
A Patient with other site of lesions and severity of dysphagia and aspiration was also considered. In which there are 5 (100%) patients with RT MCA, 1 (100%) with PICA, 1 (100%) with fronto temporal infarct and all were aspirating. But still there was no significant difference was noted in relation with their site and type of stroke including with their age and gender factor with (0.3708>p value) (Graph 2). There are 60 (65.93%) dysphagia patients who have received Active swallow exercises. 31 (34.06%) patients have been received both Active and passive swallow exercises. 78 (85.7%) of patients who have been recommended with swallow manvers. 88 (96.7%) patients have been graded with level-6 based on NOMS during the time of their Discharge, Were as 3 (3.30%) patients was discharged with Level-3 based on NOMS and later they have been visited on OPD bases for further management. On the day of 45 all 91 (100%) dysphagia patients have been achieved with normal diet +liquids orally and graded with Level-7 based on NOMS with significant (pvalue<0.001) (Graph 3).
Graph 2: Recovery of swallow pattern in Patients with Bleed and Infarct from Day 5-45 Based on Noms.
Graph 3: Recovery pattern of Swallowing in Relation with Duration based on Noms Score.
Discussion
Dysphagia is a common complication following stroke [3]. In this study we investigated the Impact of Aspiration and role of early swallow therapy in acute stroke with oro-pharyngeal dysphagia by NOMS with 7 point rating scale. The results in this study showed that early swallow therapy has significant improvement on clinical NOMS scores Aspiration/pneumonia are a common adverse infection that affects up to one-third of acute stroke patients. Aspiration/Pneumonia is also a leading cause of mortality after stroke, accounting for nearly 35% of post-stroke deaths [4]. Most stroke-related pneumonias are believed to result from dysphagia and the subsequent aspiration of oropharyngeal material. Aspiration is defined as entry of food or liquid into the airway below the level of the true vocal cords, [5,6] and aspiration pneumonia is defined as entrance of swallowed materials into the airway that results in lung infection. [4,6] A recent systematic review reported that stroke patients with dysphagia demonstrate ≥3-fold increase in pneumonia risk with an 11-fold increase in pneumonia risk among patients with confirmed aspiration. [6,7] Along with this increased risk, the burden of aspiration pneumonia is high. Increased costs associated with longer hospitalization [8], greater disability at 3 and 6 months, [8,9] and poor nutritional status during hospitalization [8] characterize aspiration pneumonia in stroke. In this study aspiration was present in 73.62% of dysphagia patients and was rated based on the Penetration aspiration scale.
Overall, all patients have improved their swallowing with significant difference (p<0.001). The good progress of the presented patients was probably because they received intensive swallowing training (30min per session) with a long number of sessions. Expert consensus support the use of manoeuvres such as chin tuck when swallowing, head turn or Mendelsohn manoeuvre. The common chin tuck entails asking patient to lower their chin towards their chest before swallowing, which brings the epiglottis and the aryepiglottic folds closer together allowing the opposition of these structures to close the airway during swallowing. The head turn is a simple rotation of head to the paretic side in an attempt to increase bolus flow. The Mendelsohn manoeuvre requires a little more training and entails the sustained contraction of the suprahyoid muscles in an effort to maintain laryngeal elevation and thus upper esophagealsphincter opening and airway closure. [9,10].
Compensatory management
CCompensatory strategies focus on implementation of techniques to facilitate continued safe oral intake of food and/or liquid; or to provide alternate sources of nutrition for maintenance of nutritional needs. Compensatory strategies are intended to have an immediate benefit on functional swallowing through simple adjustments that allow patients to continue oral diets safely. Compensatory strategies include, but are not limited to, postural adjustments of the patient, swallow maneuvers, and diet modifications (foods and/or liquids) [7,11].
Postural adjustments
Changes in body and/or head posture may be recommended as compensatory techniques to reduce aspiration or residue [12]. Changes in posture may alter the speed and flow direction of a food or liquid bolus, often with the intent of protecting the airway to facilitate a safe swallow [13]. Lists commonly used postural adjustments. In general, these postural adjustments are intended to be utilized short term, and the impact of each may be evaluated during the clinical examination or with imaging studies. Available literature on the benefit of these techniques is variable. For example, while some investigators report reduced aspiration from a chin down technique [11-13], others report no significant benefit [13] or no superior benefit to other compensations like thick liquids [12]. Furthermore, these compensatory strategies only impact nutritional status or pneumonia when they allow patients to consume adequate amounts of food/liquid in the absence of airway compromise leading to chest infection. No existing data confirms this potential benefit of postural adjustments and some data suggest that these strategies are inferior to more active rehabilitation efforts in the prevention of nutritional deficits and pneumonia. [14,15]
Swallow maneuvers
Swallow maneuvers are ‘abnormal’ variants on the normal swallow intended to improve the safety or efficiency of swallow function. Various swallow maneuvers have been suggested to address different physiologic swallowing deficits. Swallow maneuvers can be used as short- term compensations but many have also been used as swallow rehabilitative strategies. Different maneuvers are intended to address different aspects of the impaired swallow. For example, the supraglottic and super supraglottic swallow techniques both incorporate a voluntary breath hold and related laryngeal closure to protect the airway during swallowing [7]. The Mendelsohn maneuver is intended to extend opening or more appropriately relaxation of the upper esophageal sphincter [15]. Finally, the effortful or ‘hard’ swallow is intended to increase swallow forces on bolus materials with the result of less residue or airway compromise [16,17] Like postural adjustments, available data on the success of these techniques in patient populations is limited, conflicted, and often comprised of small samples [14-19]. Thus, the best advice for clinicians is to verify the impact of these maneuvers using swallowing imaging studies before introducing any of them as compensatory strategies. Also, similar to postural adjustments, no significant research has demonstrated the impact of these maneuvers, when used as compensatory strategies, on nutritional status or pneumonia [20-22].
In the present study there is a significant statistical difference before swallow therapy and after therapy of NOMS & PAS scores and the (96.7%) of patient was got discharged on soft diet along with thin liquids among which few are suggested to continue the swallow maneuver and few are not [23,24]. Patient who has received both active and passive exercises along with compensatory strategies and showed good improvement. However, these exercises can’t improve their compensation in the face of stable oropharyngeal dysfunction. Accordingly, all patients with neurogenic dysphagia, regardless of factors such as age, localization of lesion, time since lesion, type and degree of aspiration, and cognition status, should be considered for swallowing therapy [25]. Swallowing therapy appears to be relatively safe in that there was a low incidence of pneumonia during or within 4-6 weeks following therapy among those patients who achieved oral feeding [26].
On the other hand, patients who had to continue tube feeding were much more likely to suffer pneumonia, presumably because their severely compromised swallowing function not only precluded oral feeding but also predisposed to aspiration of oropharyngeal secretions and/or refluxed tube feedings. In present study all subjects were underwent evaluation by speech-language pathologist with clinical bed side swallow evaluation that included assessment of laryngeal elevation, diet tolerance, and swallowing delay and were then assigned an overall dysphagia severity score [27]. All patients have sever dysphagia in initial clinical swallow bed side evaluation with (100%) graded with severity of dysphagia with NOMS and severity of Aspiration with PAS [28]. Later after swallow therapy (96.7%) of patients were improved their functional swallowing with normal diet on day 45 and graded based on NOMS. Were as in (3.30%) of patients were graded with level-3 based on NOMS at the time of discharge and later they achieved level-7 with in same time period [29,30]. Dietary modification has done based on the patient requirement and comfort.
Conclusion
Early swallow therapy have greater effects on improving the swallowing function based on the clinical NOMS-Level-1-7 rating scale with dysphagia in stroke patients and prevent aspiration. However, large placebo study is required.
References
- Logemann JA, Veis S, Colangelo L A (1999) Screening procedure for oropharyngeal dysphagia. Dysphagia 14(1): 44-51.
- Marik PE (2001) Aspiration Pneumonitis and Aspiration pneumonia. N Engl J Med 344(9): 665-671.
- Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL (1994) Pharyngeal effects of bolus volume, viscosity and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Hear Res 37(5): 1041-1049.
- Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL (1994) Pharyngeal effects of bolus volume, viscosity and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Hear Res 37(5): 1041-1049.
- Martino R, Foley N, Bhogal S, Diamant N, Speechley M, et al. (2005) Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 36(12): 2756-2763.
- Livia Sura, Aarthi Madhavan, Giselle Carnaby, Michael A Crary (2012) Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging 7: 287-298.
- Groher ME, Crary MA (2010) Dysphagia: Clinical Management in Adults and Children. Maryland Heights, MO: Mosby Elsevier
- Crary MA, Groher ME (2003) Introduction to Adult Swallowing Disorders. Philadelphia, PA: Butterworth Heinemann.
- Teasell RW, Bach D, McRae M (1994) Prevalence and recovery of aspiration post stroke: a retrospective analysis. Dysphagia 9(1): 35-39.
- Smithard DG, O’Neill PA, Parks C, Morris J (1996) Complications and outcome after acute stroke. Does dysphagia matter? Stroke 27(7):1200– 1204.
- Ney DM, Weiss JM, Kind AJ, Robbins J (2009) Senescent swallowing: impact, strategies, and interventions. Nutr Clin Pract 24(3): 395-413.
- Kidd D, Lawson J, Nesbitt R, MacMahon J (1995) The natural history and clinical consequences of aspiration in acute stroke. QJM 88(6): 409-413.
- Rasley A, Logemann JA, Kahrilas PJ, Rademaker AW, Pauloski BR (1993) Prevention of barium aspiration during video fluoroscopic swallowing studies: value of change in posture. Am J Roentgenol 160(5): 1005-1009.
- Logemann JA, Gensler G, Robbins J, Lindblad AS, Brandt D, et al. (2008) A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res 51(1):173-183.
- Shanahan TK, Logemann JA, Rademaker AW, Pauloski BR, Kahrilas PJ (1993) Chin-down posture effect on aspiration in dysphagic patients. Arch Phys Med Rehabil 74(7): 736-739.
- Carnaby G, Hankey GJ, Pizzi J (2006) Behavioural intervention for dysphagia in acute stroke: a randomised controlled trial. Lancet Neurol 5(1): 31-37.
- Kahrilas PJ, Logemann JA, Krugler C, Flanagan E (1991) Volitional augmentation of upper esophageal sphincter opening during swallowing. AM J Physiol 260(3): G450-G456.
- Hind JA, Nicosia MA, Roecker EB, Carnes ML, Robbins J (2001) Comparison of effortful and noneffortful swallows in healthy middle-aged and older adults. Arch Phys Med Rehabil 82(12):1661-1665.
- Huckabee ML, Butler SG, Barclay M, Jit S (2005) Submental surface electromyographic measurement and pharyngeal pressures during normal and effortful swallowing. Arch Phys Med Rehabil 86(11): 2144- 2149.
- Elmstahl S, Bulow M, Ekberg O, Petersson M, Tegner H (1999) Treatment of dysphagia improves nutritional conditions in stroke patients. Dysphagia 14(2):61-66.
- Neumann S, Bartolome G, Buchholz D, Prosiegel M (1995) Swallowing therapy of neurologic patients: correlation of outcome with pretreatment variables and therapeutic methods. Dysphagia 10(1): 1-5.
- Carnaby-Mann GD, Crary MA (2008) Adjunctive neuromuscular electrical stimulation for treatment-refractory dysphagia. Ann Otol Rhinol Laryngol 117(4): 279-287.
- Robbins JA, Nicosia M, Hind JA, Gill GD, Blanco R, et al. (2002) Defining physical properties of fluids for dysphagia evaluation and treatment. Perspectives on Swallowing and Swallowing Disorders 11:16–19.
- Garcia JM, Chambers Et, Molander M (2005) Thickened liquids: practice patterns of speech- language pathologists. Am J Speech Lang Pathol 14(1): 4-13.
- Whelan K (2001) Inadequate fluid intakes in dysphagic acute stroke. Clin Nutr 20(5): 423-428.
- Robbins J, Gensler G, Hind J, Logemann JA, Lindblad AS et al. (2008) Comparison of 2 interventions for liquid aspiration on pneumonia incidence: a randomized trial. Ann Intern Med 148: 509-518.
- Wright L, Cotter D, Hickson M (2008) The effectiveness of targeted feeding assistance to improve the nutritional intake of elderly dysphagic patients in hospital. J Hum Nutr Diet 21(6): 555–562.
- Germain I, Dufresne T, Gray-Donald K (2006) A novel dysphagia diet improves the nutrient intake of institutionalized elders. J Am Diet Assoc 106(10): 1614-1623.
- Groher ME, McKaig TN (1995) Dysphagia and dietary levels in skilled nursing facilities. J Am Geriatr Soc 43(5): 528-532.
© 2017 Govathi Nikhila K, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






