- Submissions

Full Text
Orthopedic Research Online Journal
The Role of Lateral External Fixation in Paediatric Humeral Supracondylar Fracture
Ren Yi Kow* Low CL and Ed Simor Khan MJK
International Islamic University Malaysia, Malaysia
*Corresponding author: Ren Yi Kow, International Islamic University Malaysia, Bandar Indera Mahkota, 25200 Kuantan, Pahang, Malaysia
Submission: February 23, 2018; Published: March 15, 2018

ISSN : 2576-8875Volume2 Issue2
Abstract
Humeral supracondylar fracture is the most common elbow injury in children. Displaced fractures are often fixed with pinning method after a closed or an open reduction. Recently, lateral external fixation is becoming more popular in the treatment of humeral supracondylar fractures with reported good outcomes. The pros and cons of this new technique are being discussed in this review.
Introduction
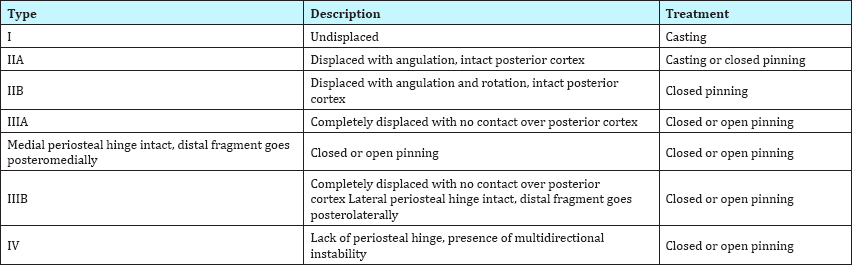
Supracondylar fracture of the humerus is the most common type of fracture at the elbow in the paediatric age group [1]. This type of injury classically occurs as a result of fall on an outstretched hand, accounting for 17% of all paediatric fractures [2]. Extension- type injury accounts for more than 90% of all supracondylar humeral fractures and it commonly involves the non-dominant hand [3]. Gartland first described the classification of supracondylar humeral fractures in 1959 to facilitate their management [4]. Since then, a modified Gartland's classification has been described with good intra-observer and inter-observer reliability [5]. A summary of the modified Gartland's classification of humeral supracondylar fractures and the respective treatment options are highlighted in Table 1.
Table 1: Types and description of the modified Gartland’s classification of humeral supracondylar fractures and the recommended treatment options [5].
Fixation using pinning method with Kirchner wires (K-wires) after an open or a closed reduction is considered the "gold standard" for Gartland III and IV supracondylar fractures [6]. Various methods of pinning have been described, including medial, lateral and combined medial and lateral approaches [7]. Biomechanical studies showed that the construct stiffness of two lateral divergent wires is similar to that of the combination of medial and lateral wires [8,9]. Moreover, avoiding medial placement of Kirchner wires also eliminates the risk of iatrogenic ulnar nerve palsy [10,11]. In fractures that are unstable or are not anatomically reduced, either three lateral divergent Kirschner wires or 2 lateral and one medial Kirchner wires can be inserted for fixation [9].
lateral external fixation
In 2008, Slongo et al. [12] introduced lateral external fixation as a new surgical technique to treat irreducible paediatric supracondylar humeral fractures. In this technique, all the Shanz pins and Kirchner wires are inserted from the radial side to avoid the risk of ulnar nerve injury. Intra-operatively, closed reduction of Gartland III and IV humeral supracondylar fractures can be challenging and the resultant conversion to open reduction can leave a bigger wound, causing more pain to the child. The "joystick" technique has been used with success to avoid open reduction [13-15]. In the lateral external fixation technique, both proximal and distal Shanz pins can be utilized as joysticks to achieve a good reduction [16]. Alternatively, another temporary Shanz pin can be placed distal to the deltoid insertion site to facilitate the rotational reduction prior to correction of sagittal and coronal planes using the proximal and distal Shanz pins [17].
Figure 1: A supracondylar humeral fracture which is fixed with cross Kirschner wires. The fixation is unsuccessful due to the rotational instability. The patient subsequently developed limited range of movement and loss of carrying angle of the right elbow. The patient also developed ulnar nerve injury secondary to the insertion of the medial Kirschner wire.

Figure 2: This patient with supracondylar humeral fracture is treated with lateral external fixation and Kirschner wire insertion. He subsequently recovers well with good cosmetic and functional outcomes.

Thirty out of 31 patients who underwent lateral external fixation for supracondylar humeral fractures had achieved good functional range of movement and all 31 of them had excellent cosmetic results [12]. Case series published by Kow et al. [17] also reported good cosmetic and functional outcomes in all bar one of their patients. Lateral external fixation offers a more superior biomechanical stability than the pinning method in flexion, extension, internal and external rotations [18]. Patients who have had lateral external fixation do not require post-operative back slab protection as a contrary to those undergoing pinning due to its more stable construction. Therefore, lateral external fixation will be useful for patients with comorbidities such as epilepsy or spasticity or for those in whom a stable fixation is difficult to be achieved as a step to anticipate unsuccessful pinning [16]. Furthermore, range of movement exercises can be started immediately post-operation when pain is tolerable, hence potentially achieving a better functional outcome. When the injured upper limb is free from the protective back slab, wound care will become easier and better. It is of utmost importance for a limb with multiple wounds.
Precaution
In lateral external fixation of supracondylar humeral fractures, care should be taken to avoid iatrogenic radial nerve palsy. It is recommended to place the proximal Shanz pin under direct vision with a drill sleeve, 2cm proximal to the fracture line to prevent injury to the radial nerve which crosses the lateral supracondylar ridge of the humerus at the diaphyseal-metaphyseal junction [13,19].
Some surgeons may argue that this new technique poses a higher risk of infection due to the presence of more hardwares. However, current evidence has shown that it has similar or reduced rate of infection compared to the closed pinning method [13,19].
Conclusion
Although pinning method is still the surgical treatment of choice for the management of supracondylar humeral fracture, lateral external fixation has a role to play in selected patients. It is advisable for orthopaedic surgeons to consider lateral external fixation technique as an effective alternative in the treatment of supracondylar humeral fracture
References
- Houshian S, Mehdi B, Larsen MS (2001) The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci 6(4): 312-315.
- Pretell Mazzini J, Rodriguez Martin J, Andres-Esteban EM (2010) Surgical approaches for open reduction and pinning in severely displaced supracondylar humerus fractures in children: a systematic review. J Child Orthop 4(2): 143-152.
- Mahan ST, May CD, Kocher MS (2007) Operative management of displaced flexion supracondylar humerus in children. Journal of Pediatric Orthopaedics 27(5): 551-556.
- Gartland JJ (1959) Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 109(2): 145-154.
- Barton KL, Kaminsky CK, Green DW, Shean CJ, Kautz SM, et al. (2001) Reliability of a modified Gartland classification of supracondylar humerus fractures. Journal of Pediatric Orthopaedics 21(1): 27-30.
- Mangwani J, Nadarajah R, Paterson JMH (2006) Supracondylar humeral fractures in children - ten years' experience in a teaching hospital. J Bone Joint Surg Br 88(3): 362-365.
- Hussain S, Dhar S, Qayoom A (2014) Open Reduction and Internal Fixation of displaced Supracondylar Fractures of Humerus with Crossed K-wires via Medial Approach. Malaysia Orthopedic Journal 8(2): 29-34.
- Feng C, Guo Y, Zhu Z, Zhang J, Wang Y (2012) Biomechanical analysis of supracondylar humerus fracture pinning for fractures with coronal lateral obliquity. J Pediatr Orthop 32(2): 196-200.
- Bloom T, Robertson C, Mahar AT, Newton P (2008) Biomechanical analysis of supracondylar humerus fracture pinning for slightly malreduced fractures. J Pediatr Orthop 28(7): 766-772.
- Anuar RIM, Gooi SG, Zulkiflee O (2015) The role of nerve exploration in supracondylar humerus fracture in children with nerve injury. Malaysian Orthopaedic Journal 9(3): 71-74.
- MA Ikram (1996) Ulnar nerve palsy: a complication following percutaneous fixation of supracondylar fractures of the humerus in children. Injury 27(5): 303-305.
- Slongo T, Schmid T, Wilkins K, Joeris A (2008) Lateral External Fixation - A New Surgical Technique for Displaced Unreducible Supracondylar Humeral Fractures in Children. J Bone Joint Surg Am 90: 1690-1697.
- Parmaksizoglu AS, Ozkaya U, Bilgili F, Sayin E, Kabukcuoglu Y (2009) Closed reduction of the pediatric supracondylar humerus fractures: the "joystick” method. Arch Orthop Trauma Surg 129(9): 1225-1231.
- Basaran SH, Ercin E, Bilgili MG, Bayrak A, Cumen H, et al. (2015) A new joystick technique for unsuccessful closed reduction of supracondylar humeral fractures: minimum trauma. Eur J Orthop Surg Traumatol 25(2): 297-303.
- Novais EN, Andrade MA, Gomes DC (2013) The use of a joystick technique facilitates closed reduction and percutaneous fixation of multidirectionally unstable supracondylar humeral fractures in children. J Pediatr Orthop 33(1): 14-19.
- Slongo T (2014) Radial external fixation for closed treatment of type III and IV supracondylar humerus fractures in children. A new surgical technique. Oper Orthop Traumatol 26(1): 75-96.
- Kow RY, Zamri AR, Ruben JK, Jamaluddin S, Mohd-Nazir MT (2016) Humeral Supracondylar Fractures in Children: A Novel Technique of Lateral External Fixation and Kirschner Wiring. Malays Orthop J 10(2): 41-46.
- Hohloch L, Konstantinidis L, Wagner FC, Strohm PC, Sudkamp NP, et al. (2015) Biomechanical evaluation of a new technique for external fixation of unstable supracondylar humerus fractures in children. Technol Health Care 23(4): 453-461.
- Horst M, Altermatt S, Weber DM, Weil R, Ramseier LE (2011) Pitfalls of lateral external fixation for supracondylar humeral fractures in children. Eur J Trauma Emerg Surg 37(4): 405-410.
© 2018 Ren Yi Kow, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






