- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
An Unusual Lesion of the Maxilla: A Case Report
Rubeena Arora*
Lady Hardinge Medical College and Associated Hospitals, India
*Corresponding author: Rubeena Arora, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India
Submission: October 24, 2017; Published: February 21, 2018

ISSN: 2578-0069Volume1 Issue2
Abstract
Introduction: Keratocystic odontogenic tumour (KCOT) is a distinct lesion of odontogenic origin. Cases may be sporadic or associated with Gorlin syndrome. Treatment is controversial.
Case report: A case of a 26 year old male with histopathologically proven Keratocystic odontogenic tumour of maxillary sinus with fistulous tract leading from maxillary sinus to infra orbital margin is presented. It was treated with enucleation and fistulectomy. Follow up was uneventful.
Discussion: Keratocystic odontogenic tumour (KCOT) is a benign lesion with aggressive potential. There are many treatment modalities. Present case is being highlighted because of a novel clinical presentation of an associated fistula in absence of antecedent trauma.
Conclusion: Keratocystic odontogenic tumour (KCOT) may have atypical presentation and hence should be considered in differential diagnosis of all maxillary/mandibular cysts.
Keywords: Keratocystic odontogenic tumour (KCOT); Fistula
Introduction
Keratocystic odontogenic tumour (KCOT) is a distinct lesion of odontogenic origin. It is a benign lesion but can be locally aggressive. Usual sites of occurrence are mandible and maxilla with mandibular involvement being more common [1]. Keratocystic odontogenic tumour (KCOT) has a higher tendency of recurrence compared with other odontogenic lesions, and hence treatment is controversial. Clinical presentation of Keratocystic odontogenic tumour (KCOT) is quite variable. Here we present a case of Keratocystic odontogenic tumour (KCOT) of maxilla which also had an associated fistulous opening just below the patient s right eye.
Case Report
Figure 1: Black arrow: fistulous opening.

Figure 2: Pus discharge on Valsalva maneuver.

A 26 year old male was referred to the ENT OPD from the Dental Department with chief complaints of swelling in the right cheek region of his face for the past 10 months and an opening just below his right eye for the past 2 months. Examination revealed a diffuse, hard swelling involving the right maxillary area, size approx. 3 X 3cm. The swelling was non tender and local temperature was not raised. Overlying skin was normal (Figure 1). Oral cavity examination revealed palatal expansion on the right side. Examination of the region below the right eye revealed a small opening of size approx. 3 X 3mm, present about 5 mm below the infra orbital margin and 3 mm medial to lateral canthus (Figure 2). Frank pus discharge would occur from this opening whenever the patient performed Valsalva manoeuvre (Figure 3). There was Nose and throat examination were normal. Chest X-ray was normal. no antecedent history of trauma or any prior surgical intervention. Routine blood examination reports were within normal limit.
Figure 3: CT pictures showing involvement of maxillary sinus. Two impacted teeth can be seen.
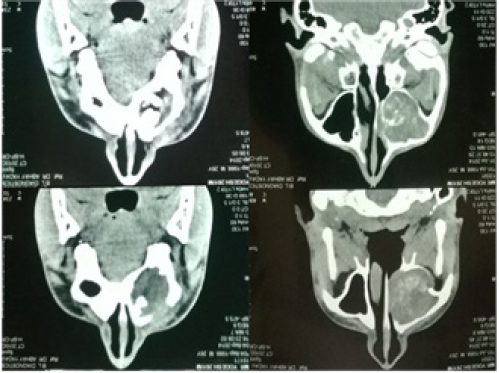
Contrast-enhanced computed tomographic scan of the nose and paranasal sinuses revealed a neoplastic expansile mass with hyperdense areas of calcification in the right maxillary sinus causing expansion, thinning and scalloping of sinus walls with cortical breach. Two unerupted teeth were seen within lower part of lesion. Head CT was normal. Based on clinical and radiological findings, differential diagnoses of keratocystic odontogenic tumour, osteomyelitis, dentigerous cyst, ameloblastoma, calcifying epithelial odontogenic tumour (Pindborg tumour), odontogenic myxoma (tennis racket pattern), and neoplastic lesion viz squamous cell carcinoma were considered.
Figure 4: HPE showing parakeratinization.

The patient underwent biopsy of the lesion under general anesthesia via Caldwell-Luc approach. Histopathological examination of the lesion showed a cystic lumen lined by corrugated parakeratinized stratified squamous epithelium of 6-8 cell layer thickness. The basal layer showed tall columnar cells with reversal of polarity. Basal cell budding was evident at many areas. Separation of the lining from the underlying connective tissue was seen with flat interface at other areas. The findings were consistent with keratocystic odontogenic tumour (Figure 4).
Definitive treatment of the patient was undertaken after reviewing histopathology report. The patient underwent enucleation of entire mucosal lining of maxillary sinus with removal of impacted teeth, and fistulectomy with closure of the fistula opening. The maxillary sinus was packed with BIPP (bismuth iodophore paraffin paste) soaked tape-gauze. The packing was removed after 2 weeks. Postoperative period and follow up were uneventful.
Discussion
Keratocystic odontogenic tumour (KCOT) was formerly known as odontogenic keratocyst. It was reclassified by WHO in 2006 from an odontogenic cyst to a benign odontogenic tumour and renamed keratocystic odontogenic tumour (KCOT) [2,3]. It is locally aggressive, and has been designated as a benign tumour based on its tendency for local recurrence. There is molecular evidence of bi- allelic loss of tumour suppressor gene in KCOT. Symptoms include swelling which may be painful or painless.
Keratocystic odontogenic tumour (KCOT) occurs in two clinical settings. Most are sporadic solitary cases presenting at a mean age of 40 years. Rest occur as part of the naevoid basal cell carcinoma syndrome-also known as Gorlin syndrome.Gorlin syndrome is a rare autosomal dominant syndrome characterized by multiple basal cell carcinomas, keratocystic odontogenic tumors (KCOT), rib and vertebral abnormalities, intracranial calcifications and distinct facial abnormalities [4]. Gorlin syndrome was first described in 1960 and its incidence range from 1 in 50,000 to 150,000 [5]. Molecular genetics revealed that Gorlin syndrome is caused by mutation in PTCH gene located on chromosome 9q1 [6]. The present case was likely a sporadic case, as Head CT and chest X-rays were normal.
Keratocystic odontogenic tumour (KCOT) is a distinct lesion, owing to its unique histopathology. The cystic lining is characterized by a parakeratinized stratified squamous epithelium of uniform thickness, with a corrugated surface and a palisaded and polarized basal layer with "picket fence" or "tombstone" appearance, devoid of rete ridges. Numerous infoldings of the epithelium are a common finding. The cystic lumen generally contains a straw colored fluid or a thick creamy material which may represent keratin [7]. These were the histopathological features in our case as well.
Role of immune histochemistry
Immuno histochemistry may be used to identify expression of p63 protein. P63 is a gene belonging to the family of p53 tumour- suppressor genes. P63 protein expression in KCOT correlates with increased aggressive behaviour of the tumour, and therefore relevant modification in the treatment strategy may be required [8].
Treatment strategy
Treatment of KCOT is controversial. There are many methods of treatment- enucleation plus cryosurgery, enucleation followed by Carnoy solution application, enucleation plus peripheral ostectomy, marsupialization and decompression. Recurrence rate for all methods is similar due to the nature of lesion-viz 20-60%. In our case we performed enucleation of the tumour via Caldwell-Luc approach, stripping of mucosa of the maxillary sinus, and excision of the fistulous tract with closure of the fistulous opening. The sinus was packed with medicated tape-gauze.
Carnoy's solution is a solution made up of 30% chloroform, 60% absolute ethanol and 10% glacial acetic acid. It is often used in cases of recurrent Keratocystic odontogenic tumour (KCOT). It promotes chemical necrosis of and elimination of epithelial remnants. The US FDA banned the use of chloroform in 2013 leading to use of 'modified' Carnoy's solution i.e. without chloroform. However research conducted in 2015 found that the recurrence rate of KCOTs treated by enucleation and curettage with application of Carnoy’s solution is significantly lower than that of modified Carnoy's solution [9].
Methods to reduce recurrence of KCOTs have been extensively researched, with no clear guidelines emerging. Pogrel et al. [10] used a modified treatment strategy of decompression followed by peripheral ostectomy and claim a very low recurrence rate-they have seen no recurrence till date with the longest follow being 5 years. Our case merits mention due to the unique clinical presentation of a fistula, in the absence of trauma or surgical intervention. Thus KCOT must be considered in the differential diagnosis of maxilla as well as jaw lesions. Our case also highlights the importance of collaboration between the ENT and dental clinics.
References
- Bello IO (2016) Keratocystic odontogenic tumor: A biopsy service's experience with 104 solitary, multiple and recurrent lesions. Med Oral Patol Oral Cir Bucal 21(5): e538-e546.
- Philipsen HP (2005) Keratocystic odontogenic tumour. In: Barnes L, Eveson JW, Reichart P, Sidransky D (Eds.), World Health Organization Classification of Tumours. Pathology and genetics of head and neck tumours. IARC Press, Lyon, France, pp. 306-307.
- Reichart PA, Philipsen HP, Sciubba JJ (2006) The new classification of head and neck tumours (WHO)-any changes? Oral Oncol 42(8): 757-758.
- Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, et al. (1997) Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet 69(3): 299-308.
- Gorlin R, Goltz RW (1960) Multiple nevoid basal-cell epithelioma, jaw cysts and bifid rib. A syndrome. N Engl J Med 262(18): 908-912.
- Ohnson R, Rothman A, Xie J, Goodrich L, Bare J, et al. (1960) Human homolog of patched, a candidate gene for the basal cell nevus syndrome. Science 272(5268): 1668-1671.
- Shafer WG, Hine MK, Levy BM (1983) Cysts and tumours of odontogenic origin. In: Shafer WG, Hine MK, Levy BM (Eds.), A Textbook of Oral Pathology, (4th edn), WB Saunders Company, USA.
- Varsha B, Gharat AL, Nagamalini B, Jyothsna M, Mothkur ST, et al. (2014) Evaluation and comparison of expression of p63 in odontogenic keratocyst, solid ameloblastoma and unicystic ameloblastoma. J Oral Maxillofac Pathol 18(2): 223-228.
- Dashow JE, McHugh JB, Braun TM, Edwards SP, Helman JI, et al. (2015) Significantly Decreased Recurrence Rates in Keratocystic Odontogenic Tumor With Simple Enucleation and Curettage Using Carnoy’s Versus Modified Carnoy's Solution. J Oral Maxillofac Surg 73(11): 2132-2135.
- Pogrel MA (2015) The keratocystic odontogenic tumour (KCOT)-an odyssey. Int J Oral Maxillofacial Surg 44(12): 1565-1568.
© 2017 Rubeena Arora. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






