- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
The Clinical Applied of Intraneural Topography of Musculocutaneous Nerve
Mohamed Abd El Aziz Mohamed Ali1*, Mohamed Abdelfattah1 and Ayman M Ismail2
1Lecturer of Orthopedic Surgery, Faculty of Human Medicine, Zagazig University, Egypt
2Lecturer of Neurosurgery, Faculty of Human Medicine, Zagazig University, Egypt
*Corresponding author: Mohamed Abd El Aziz Mohamed Ali, Lecturer of Orthopedic Surgery, Faculty of Human Medicine, Zagazig University, Egypt
Submission: November 10, 2017; Published: December 05, 2017

ISSN: 2578-0069Volume1 Issue2
Abstract
Object: Loss of biceps function is a significant disability after brachial plexus root avulsion injuries. Study of nerve topography of musculocutaneous nerve and knowledge of internal motor fascicles of biceps and brachialis muscles is important as the available nerve fibers for transfer as anterolateral fascicles of the ulnar nerve, intercostal nerves and Median nerve fascicles have small number of motor nerve fibers so maximize the nerve supply to biceps and brachialis by study of topography of musculocutaneous nerve.
Method: [1] Cadavers, [2] limb with musculocutaneous nerve was dissected and its motor branches to biceps and brachialiswas studied under magnification. The motor branch of musculocutaneous nerve exits distal to the coracoids process , nerve to coraco-brachialis emerge at first on lateral side , then motor branch of biceps and brachialis then the continuation of lateral cutaneous nerve the forearm. 16 cases of brachial Plexus palsy treated by nerve transfer 10 cases by Obrelienulnar nerve and 6 cases intercostal nerves neurotization to motor fascicles to biceps and brachialis.
Result: Motor fascicles to biceps and brachialis is central nerve fiber in the musculocutaneous nerve in our cadaveric study and recovery of biceps in brachial plexus injuries was 7 Toronto score in 15 cases of 16 cases wear reconstructed by nerve transfer.
Conclusion: Study of the internal topography of the musculocutaneous nerve seeks to maximize functional outcome by decreasing the distance and time of neural regeneration and increasing the specificity of motor donor inflow to biceps and brachialis muscle.
Keywords: Brachial plexus; Musculocutaneous; Nerve; Topography
Introduction
Denervation of the biceps is an inevitable consequence of sever avulsion brachial plexus injuries. These injuries are challenging reconstructive issues for the surgeon. The relative slow rate of nerve regeneration and limited number of motor nerve fibers which available to transfer are important before the operation. The knowledge about the internal topography of musculocutaneous motor fibers to the biceps is mandatory. This knowledge helps to avoid loss of number of donor nerve axons which may sprouts away from the affected end organs of muscles [3]. Preoperative angiographic studies can determine normal and anomalous arteries and veins. In case of nerves it is not feasible to detect such anomaly and. The musculocutaneous nerve anterior to the brachial artery (1 limb) 3.3% and common course lateral to it 11 limb (96.7%) [4]. Brandt et al. [5] described a technique for maximizing biceps recovery in brachial plexus palsy. They mentioned that one half of the fibers entering the musculocutaneous nerve terminate in cutaneous receptors [5].
Invasion of Schwan cells from the distal segment into the epineurium of the donor nerve was a crucial step for the initiation of collateral sprouting from the intact nerve. The use of nerve transfer for motor re-enervation after brachial plexus injury only if other options are not available [6]. Oberlin nerve transfer (15 percent of the fascicles of the intact ulnar nerve are severed in the upper arm, and the cut fascicles are sutured4 end-to-end to the biceps nerve) [7]. Oberlin ulnar nerve to biceps nerve transfer in birth palsy cases and in cases with an intact phrenic nerve and avulsion of the upper roots of the brachial plexus. He routinely obtained full recovery of the biceps (Toronto muscle grade 7) in every case without any clinical deficits of the donor nerve [7]. Using a single fascicle from the ulnar nerve to the biceps function was originally described in adults by Sungpet et al. from Thailand; however, Oberlin was the first to use this technique in OBPP cases. Oberlin nerve transfer has several advantages, including simplicity, good size match between the transferred fascicle of the ulnar nerve and the biceps nerve, the lack of notable donor nerve deficit, no need for nerve grafting, and the short distance neurorrhaphy site and the motor end plate and recovery occurs on average after 14 weeks only. This quick recovery due to the proximity to the muscle, also allows salvage of deficit before permanent atrophy in patients who present late [1].
Chuang et al. [8] used intercostal nerve transfer for irreparable avulsed brachial plexus injuries, obtaining a good result are (1) early exploration (less than 5 months after trauma), (2) use of three intercostal nerves, (3) mixed nerve-to-mixed nerve coaptation, (4) nerve repair without grafts and under no tension.
Narakas [9] introduced intra plexal transfers and pointed out that the concept of neurotization, i.e., transfer of an uninjured nerve to the distal stump of an injured nerve. Narakas [9] noted 1200 to 1300 myelinated fibers in one intercostal nerve, whereas the musculocutaneous nerve contained about 6000 fibers. Perhaps more intercostal nerves will provide more donor axons, thereby achieving greater biceps strength. They added that it is not clear which intercostal nerves are best for transfer. Neuroanatomy considerations consequence in order to obtain an acceptable reinnervation of the recipient nerve, the donor nerve must supply a comparable number of motor fibers. Adequate reinnervation is beyond the capacity of the majority of the donor nerve [9]. Fiber controls of the peripheral nerves approximate values of the of the musculocutaneous nerve is 6000, median nerve 1800, ulnar nerve 1600, one intercostal nerve 1200-1300, so the available donor motor nerve axons are severely limited number in comparison to the number of axons in recipient nerve [9].
Approximately 15% of the fascicles the ulnar nerve and 20% the fascicles of the median nerve were used as donor motor nerves to the biceps and brachialis so intraneural topography of musculocutaneous motor nerve is identified and separated to prevent loss of limited motor nerve fibers [3].
Materials and Methods
Twelve limbs from adult cadavers 5 males and 1 female, age range from 35-70 years were dissected for this study. All cadavers were placed in supine position with limb extended and shoulder abducted under high magnification between 4.0 and 8.0, the medial arm was incised along the interval between the biceps and triceps muscles and extended as diltopectoral groove in the infraclaviclar exposure of brachial plexus, musculocutaneous nerve arises from the lateral cord (11 Limb), from lateral and posterior cord (1 limb). A number of variations in the course and distribution of the musculocutaneous nerve reported piercing the coracobrachialismuscle, the nerve may adhere to the median nerve down the arm and then pass between the biceps and brachialis muscles to supply all three muscles. The musculocutaneous accompanied by fibers from the median nerve [4] limb. Communicating branch passes from the musculocutaneous nerve to the median (2 limbs), the anastomoses occur between the nerves of the limbs, these errors in the course of the nerves, placed nerve fibers, in order, to get their proper end-point , the bundle of nerve fibers leaves the in appropriate nerve, turns and joins the proper nerve trunk. The musculocutaneous nerve pierces the coracobrachialis (8 limbs), the muscular branch of the nerve dose not pierce the muscles (3limb). The musculocutaneous nerve was found immediately and deep and lateral to the median nerve, under the substance of the biceps muscles. The motor nerve of biceps and brachialis was grouped in group (A) single motor branch arises from the musculocutaneous nerve [9] and Group (B) [6] two primary motor branch innervate the biceps and brachialis from the main nerve trunk. The motor fascicles to biceps and brachialis and the lateral cutaneous nerve of the forearm nerve constantly located from lateral to medial (12 limb) (Figure 1).
Figure 1: Cadaveric study: A) showing theright upper limb with (1) musculocutaneous nerve (2) variant biceps muscular branch of 1 musculocutaneous nerve B) (1) biceps muscle (2) biceps muscular branch of musculocutaneous nerve (3) hilum of biceps muscle 4- brachialis muscle nerve and lateral cutaneous nerve of forearm.
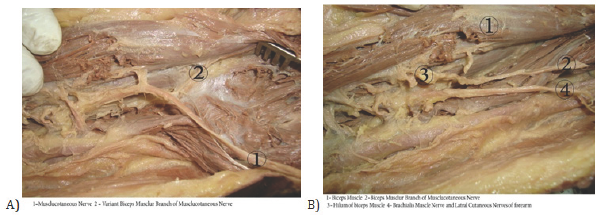
The musculocutaneous nerve and branching pattern to biceps and brachialis. Branching to biceps brachii into Group (A) (8 limb) primary motor branch that bifurcate to 2 secondary nerve branches to innervate the long and short heads of biceps. Group (B) (3 limb) two primary motor branches from the main the trunk, the proximal innervates the short head and the distal innervates the long head of biceps brachii. Group(c) (1 limb) variation from group A with a primary motor branch that bifurcates into two secondary nerves to innervate the two heads of biceps individually with an additional primary branch innervates the common belly of the biceps muscle.
Sixteen cases of brachial plexus palsy, 9 female, 7 male, 10 upper (C5-6) lesion, and 6total brachial plexus palsy. We dissected the musculocutaneous nerve till its intramuscular course. After epineurotomy, internal neurolysis was done to exclude any branches to coracobrachialis, two motor fascicle of biceps and brachialis are identified, these fascicles sectioned as proximal as possible, rerouted and are coapted to the donner nerve, coaptation is maintained by microsuture. Distally, the lateral cutaneous nerve of the forearm was identified. To innervate the biceps directly as close as possible to the branches of musculocutaneous nerve where the maximum number of motor end plates is located.
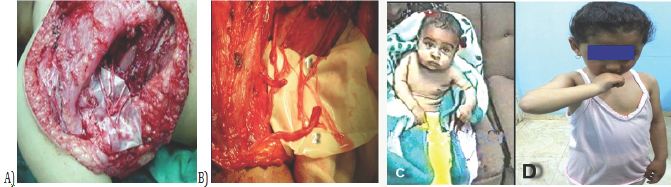
Figure 2: Case 2: FCU motor branch of ulnar nerve to biceps. Motor muscular branch of musculocutaneous nerve.

Ten cases were reconstructed by Oberline nerve transfer after epineurotomy of the ulnar nerve, motor fascicle supply to flexor carpiulnaris not motor supply to small muscles of the hand and flexors of fingers was identified by direct stimulation by nerve stimulator, it was anterolateral fascicles of the ulnar nerve, sectioned as long and proximal as to overcome the distance, rerouted and co- apted to the motor nerves of biceps and brachialis and maintained by micro suture (Figure 2a). Six cases were reconstructed by inter costal nerves (T3-T4-T5) motor branch was used as donor nerves to motor branch of biceps and brachialis (Figure 3a & 3b). Each (ICN) was cut 1cm distal to the mammary line and mobilized proximally to the posterior axillary line, the length of the (ICN) and the length of the motor branch of biceps and brachialis allowed a tension free suture and was coapted the arm in abduction and external rotation of the shoulder joint, nerve coaptation as maintained by micro suture.
Figure 3: Case 1: T3-4-5 motor branch of intercostal nerves to biceps and brachialis motor muscular branch of musculocutaneous nerve.
Result
In our cadaveric study, the mean length of the reference line between medial epicondyle and coracoid process was 150 mm. Total numbers of cadavers [1], the right and left upper limb 12, female 1 and male 5. Origin of musculocutaneous nerve from lateral cord 11 limb (91.7%), from lateral and posterior cord 1 limb (8.3%) course of musculocutaneous nerve, piercing coracobrachialis 8 limb (66.7%) not piercing coracobrachialis 3 limbs (25%) and the muscular branches piercing the muscle 1 limb (3.8%). Communication between median and musculocutaneous nerve: Communication 2 limb (16.7%) Internal neurotopography of muscles cutaneous exit of branches from lateral to medial, motor branch to coracobrachialis emerge from lateral side 12 limb (100%), motor branch to biceps muscle emerge from lateral side 11 limb (91.7%) and from lateral side of lateral cord 1 limb (8.3%) Motor branch to brachialis laterally from main trunk after exit of biceps motor branch 12 limb (100%). Lateral cutaneous nerve of the forearm as the terminal continuation in 12 limb (100%). The group of fascicles to biceps and brachialis and the lateral cutaneous of the forearm arranged from lateral to medial and the motor fibers dissected proximally in the average distance (40-60 mm). Fifteen cases of brachial plexus palsy elbow flexion were full motor functional recovery started from (four) months postoperative to reach full recovery in 1 year (Figure 2b, 2c, 3c & 3d) 9 cases full motor functional recovery at 6 months, 6 cases full motor functional recovery at 1 year (1 case in Oberlin and 5 cases in ICN transfer). In our study one case was fair recovery of elbow flexion was reconstructed first by ICN, we did secondary reconstructive procedure by tendon transfer by lateral head of triceps to biceps tendon, and functional recovery of elbow flexion was good active elbow recovery after 8 months from secondary procedure.
Discussion
In our study the motor branches to biceps and brachialis muscles was dissected proximally from their points of exits from the main nerve trunk for a distance ranges from (40mm-60mm) so musculocutaneous nerve is mono fascicular in pattern and plexiform with limited pattern of branching joining and wandering pathway. The motor branches dissected proximally to (44mm- 53mm) Pariyut [10]. In our study origin of (MCN) from lateral cord (91.7%) and posterior and lateral cord (8.3%). Ronald [11] the nerve arises from lateral cord (90.5%) and lateral and posterior cord 4% and from posterior cord 4.1%. In our study, the course of the nerve piercing the coracobrachialis (66.7%) not piercing (25%). Ronald [7] Piercing (78%), not piercing (22%) [7]. In our study Communication between median and musculocutaneous16.7%. No communication (83.3%). Ronald [6] Communication between median and musculocutaneous 8%, no communication 92%. In our study the branching motor fibers to biceps muscle Group A (66.7%) Group B (25%) Group C (8.3%). Pariyut [10] Group (1) 62%, Group (2) (33%) and Group (3) 5%.
In our study , the motor fascicles to biceps and brachialis is central in the musculocutaneous nerve trunk and dissected proximally for distance 40mm to 60 mm. Internal topography of the musculocutaneous nerve below the coracoid process from the lateral side emerge the motor branch to the coracobrachialis muscles (12 limb), the biceps motor branches emerges as it branched laterally from the main trunk of the nerve at midpoint of biceps muscle (11 limb) and in (1 limb) the motor branch to biceps muscle emerge more proximally as it pierces the coracobrachialis. In our study the musculocutaneous nerve branch to the brachialis muscle was identified as it branched to the lateral aspect of the muscle distal to the origin of the biceps motor branch [2]. The rest of the musculocutaneous nerve continues as the lateral cutaneous nerve of the forearm (12 limb).
The motor fascicles to biceps and brachialis is centrally in the musculocutaneous trunk 12 limb (100 %). In our study MCN nerve branching patterns of the biceps: The branching nerve to biceps branching to biceps muscle are three groups: group A 8 limb (66.7%) group B 3 limb (25%) group C 1 limb (4.3%). In our study MCN nerve branching patterns of the brachialis: branching nerve to brachialis muscle are two groups: group A 8 limb (66.7%) and group B 4 limb (34.3%). The motor fascicle of biceps and brachialis dissection is monofasicly 12 limb (100 %).
Je Hun Lee [12] the mean length of the reference line between medial epicondyle and coracoid process was 275.1 14 .8mm. MCN nerve branching of the biceps is 3 types: Type I (57, 1%), type II (39.3%) and Type III (3.6%). MCN nerve branching patterns of the brachialis muscle two types: Type I (55, 4%), Type II (44.6 %). In our study the advantage of clinical topography of (MSN) study was excellent in 16 cases of brachial plexus, fully functional recovery in 15 cases, no need for nerve graft, no mixing of sensory and motor axons at nerve transfer and short time of recovery so increasing the function outcome of brachial plexus recovery and musculocutaneous nerve reconstruction. In our study 10 cases of brachial plexus injury were reconstructed by obrelien technique 9 cases were full elbow flexion against resistance by 8 months (90%) and 1 cases active elbow flexion against resistance by 12 months (10%). Robert J [2] 6 cases of brachial plexus injury (C5-6 avulsion was managed by using 1 or 2 fascicles of an intact ulnar nerve for direct fascicular transfer to biceps motor branch, early recovery by 2-3 months and regain flexion against gravity by 6 months. In our study 6 cases of brachial plexus injury (MCN) were reconstructed by (T3, T4 and T5) inter costal motor branches technique 5 cases were full elbow flexion against resistance by 12 months (83.4%) and 1 cases fair elbow flexion (16.6%). Kawabata et al. [13] third through sixth inter costal motor branches technique for direct coaptation was MCN neurotization for elbow flexion, results (84%) of cases active elbow flexion against resistance. The percentage of satisfactory recovery in our study was 15/16(94%).
Conclusion
Mixing of sensory and motor axons at nerve transfer decreases the specificity of motor donner inflow and decreases the functional outcome of MCN recovery. For this reason, the study of internal topography of MCN seeks to maximize functional out come by decreasing the distance and time of neural regeneration. Another advantage is the preservation of motor end plate architecture and function after denervation. Using selective donner motor nerve transfer gives little morbidity, can result in excellent functional elbow flexion recovery and able to relearn functions independently.
References
- AL Qattan MM (2002) Oberlin's ulnar nerve transfer to biceps nerve in Erb's Palsy. Plast Reconstr Surg 109(1): 405-407.
- Robert JS, Alexaner YS, Allen TB (2005) Update on brachial plexus surgery in adult. Techniques in Hand Upper Extermity Surgery 9(4): 220-232.
- Nath RK, Lyons AB, Bietz G (2006) Physiological and clinical advantages of median nerve fascicles transfer to musculocutaneous nerve following brachial plexus root avulsion injury. J Neruosurg 105(6): 830-834.
- Beheiry EE (2004) Anatomical variations of the median nerve distribution and communication in the arm. Folia Morphol 63(3): 313318.
- Brandt KE, Mackinnon SE (1993) A technique for maximizing biceps recovery in brachial plexus reconstruction. J Hand Surg Am 18(4): 726733.
- Bisinella GL, Birch R, Smith SJ (2003) Neurophysioglical prediction of outcome in brachial plexus palsy. J Hand Surg 28(2): 148 -152.
- Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, et al. (1994) Nerve transfer to biceps using apart from ulnar nerve for C 5- C6 avulsions of brachial plexus anatomical study and report of four cases. J Hand surg Am 19(2): 232-237.
- Chuang DC, Ma HS, Wei FC (1998) A new evaluation system to predict the sequelae of late obstetric brachial plexus palsy. Plast Reconstr Surg 101 (3): 673-685.
- Narkas AO (1984) Thoughts on neurotization or nerve transfer in irreparable nerve lesions. Clin Plast Surg 11(1): 153-159.
- Pariyut C, Somsak L, Kiat W, Chairoi U, Phairat T (1998) Anatomy and internal topography of the musculocutaneous nerve. The nerves to the biceps and brachialis muscle. The Journal of Hand Surgery 23(2): 250255.
- Bergman RA, Afifi AK, Roysuk M (1995) Variation in median and musculocutaneous nerves in the arm; Buch Hansen, K uber Varietaten des Nervus medianus und des Nervus musculocutaneus und deren Beziehungen. Anat Anz 102: 187-203.
- Lee JH, Kim HW, Im S, An X, Lee MS (2010) Localization of motor entry points and terminal intramuscular nerve endings of the musculocutaneous cutaneous nerve to biceps and brachialis muscles. Surg Radiol Anat 32(3): 213-220.
- Kawabatta H, shibata T, Matswiy (2001) Use of inter costal nerves for neurotization of musculocutaneous nerve in infants with birth related brachial plexus palsy. J Neurosurg 94(3): 386-391.
© 2017 Mohamed Abd El Aziz Mohamed Ali, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






