- Submissions

Full Text
Trends in Telemedicine & E-health
A Retrospective Analysis of ICD Lead Revision Presentations –Impact of Telemetric Care
Panagiotis Xynogalos1,2,3, Janina Althöfer1,2,3, Rasmus Rivinius1,2, Christopher Gose4, Elisabeth Grünberg1,2, Dierk Thomas1,2,3, Patrick Lugenbiel1,2,3, Norbert Frey1,2,3 and Ann-Kathrin Rahm1,2,3*
1Heidelberg Center for Heart Rhythm Disorders, Heidelberg University Hospital, Germany
2Department of Cardiology, Angiology and Pneumology, Heidelberg University Hospital, Germany
3DZHK (German Center for Cardiovascular Research), Partner site Heidelberg/Mannheim, Germany
4ZDI Heidelberg, Germany
*Corresponding author:Ann-Kathrin Rahm, Heidelberg Center for Heart Rhythm Disorders, Department of Cardiology, Angiology and Pneumology, Heidelberg University Hospital, and DZHK (German Center for Cardiovascular Research), partner site Heidelberg/Mannheim, 69120 Heidelberg, Germany
Submission: October 17, 2025;Published: October 31, 2025

ISSN: 2689-2707 Volume 6 Issue 1
Abstract
Background: In case of ICD lead dysfunction, interference signals can be misinterpreted as ventricular
fibrillation, leading to inappropriate shocks, which are harmful and traumatic for patients. This study
retrospectively analyzed a large single-center device registry to assess the clinical impact of remote
monitoring on electrode defects in relation to symptoms, presentation mode, and treatment.
Method: Adult ICD and S-ICD patients who underwent lead revision between 2015 and 2023 were
included. Two groups were identified: a conservatively ambulatory monitored control group and a
telemonitored group. Data were descriptively analyzed. Logistic regression was used for “number of
inappropriate shocks”, and Kaplan-Meier for “time from detection of RV lead defect to revision”.
Result: Numbers of actively telemonitored patients increased from 2017 to 2023 from 0 to 109. Of in total
146 telemonitored patients during that time frame, 5 (3.4%) underwent revision for electrode defects,
compared to 145 (4.7%) of 3056 conservatively monitored patients. Eleven patients in the control
group and none in the telemonitored group experienced inappropriate shocks (p=0.792). The time from
defect detection to revision was shorter in the telemonitored group (4.0 vs. 30.9 days, p=0.692). Most
patients with defective lead presented because of a warning tone/vibration alarm (29.9%), followed by
the defect being diagnosed during a planned ambulatory ICD interrogation (20.4%). 6.4% of patients
experienced an inappropriate shock. For most patients, the setting of diagnosis of the defect was either
their cardiologist or the outpatient office of a university hospital (together 49.0%). 26.8% presented
directly in the emergency room.
Conclusion: Remote monitoring reduced inappropriate shocks by enabling earlier detection of lead
defects. Expanding telemonitoring may improve early detection and may prevent inappropriate shocks
and utilization of emergency medicine services.
Keywords:ICD lead dysfunction; ICD lead revision; Telemonitoring; Inadequate shocks
Introduction
Heart failure is one of the leading causes of death in Germany. In 2015, 5.1% of all deaths occurred from heart failure; for women, it is the second most common cause of death and for men, heart failure was the fourth most common cause of death [1]. Implantable Cardioverter Defibrillators (ICDs) and Subcutaneous (S-)ICDs are an important component in the treatment of ventricular tachyarrythmias for primary prevention and secondary prevention of Sudden Cardiac Death (SCD). Mortality from cardiac arrhythmias has increased in Germany in recent years. While in 2000 26.0 per 100.000 died, in 2021 it was 28.5 per 100.000 [2]. In cases of documented Ventricular Fibrillation (VF) or hemodynamically intolerable Ventricular Tachycardia (VT), the ICD can reduce overall mortality by 28% [3]. The number of ICD revision operations was 19.8% in 2020 of all ICD procedures in Germany [4] with lead dysfunctions being the most common reason for ICD revisions [5]. Inappropriate shocks are one of the most dramatic consequences of lead dysfunction. These shocks are harmful for the myocardium and can lead to myocardial damage as well as severe psychological impairment [6]. Shocks are perceived differently by patients: some describe it as very painful. 20% of patients implanted with an ICD for primary prevention experienced shocks within 5 years [7]. Among secondary prevention patients, 85% receive shocks within 3 years [8]. The symptoms of post-traumatic stress disorder were detected in 13% of patients who experienced a shock [9]. The fear of shock delivery and the associated consequences might lead to a panic disorder, which in turn can trigger a shock if the lead is dysfunctional [10]. Therefore, preventing inappropriate shocks is very important in ICD patients.
Significant improvement in programming as well as differentiating algorithms have been achieved over the last years, causing a substantial reduction in inappropriate shocks. Nevertheless, telemetric monitoring of the ICD and S-ICD might help to detect a dysfunctional lead even before an inappropriate shock occurs. Compared to an ambulatory setting where the patient is required to present every 6 months for a device interrogation, telemedicine monitoring has been shown to detect an event 4.9±0.5 months earlier [11]. In an ICD population study in France, telemedicine reduced the number of inadequate ICD shocks by 52% and reduced the hospitalization rate by as much as 72% with no effect in mortality [12]. In another study including patients with ICD, pacemakers or CRT telemonitoring showed an absolute mortality reduction of 1.9% [13]. The scope of this retrospective single center analysis was to descriptively measure effects of telemetric monitoring in an ICD lead revisions patient collective to analyze the clinical course of the patients including utilization of emergency medicine services and to assess if telemetric monitoring influenced inadequate shocks and time to revision.
Materials and Methods
Patients
Our study was conducted in accordance with the ethical standards of the Declaration of Helsinki. The local institutional review board gave approval to this study (ethics approval number: S-018/2023). It did not require additional consent for this observational study as only routine clinical data were utilized. We screened all patients (≥18 years) who underwent ICD and S-ICD revision at the center, between 2015 and 2023. Only patients with ICD/S-ICD lead revisions due to lead dysfunction were included. Exclusion criteria were age under 18 years and other indications for ICD and S-ICD revision operations other than electrode dysfunction. Patients undergoing ICD and S-ICD lead revisions were stratified according to the device interrogation plan: telemetric monitoring or ambulatory monitoring. The planning for either ambulatory interrogation or telemedicine was dependent on the individual clinicians and patient decision. There was neither a preselection nor randomization concerning the application of telemetric monitoring or ambulatory monitoring during the study period.
Follow-up
Follow-up of ICDs and S-ICD was performed in accordance with center’s routine clinical protocol every 3-6 months depending on the type of electrode, battery status or telemonitoring intervals. After hospital discharge following ICD and S-ICD implantation, patients were seen 4-6 weeks after implantation in the outpatient office, and approximately two times per year thereafter (with routine visits in external cardiological outpatient offices or within the department’s outpatient office). ICD and S-ICD routine inhouse follow-up included ICD and S-ICD interrogation, medical history, physical examination and resting 12-lead ECG. Telemetric monitoring was performed with the respective companies telemetric monitoring system and data transferred directly to our MediConnect database (Fleischhacker GmbH & co. KG, Schwerte, Germany).
Statistical analysis
The primary scope of this study was to retrospectively analyze a large single-center device registry to assess the clinical impact of remote monitoring on electrode defects in relation to symptoms, presentation including utilization of emergency medicine services, and treatment in patients with ICD and S-ICD lead revision. Patients with ICD and S-ICD lead revisions were assessed by stratification in two groups, one with telemonitoring and one without ambulatory interrogation. Mode, symptoms including inadequate ICD and S-ICD shocks and location of patient presentation were assessed. Logistic regression was used for “number of inappropriate shocks”, and the Kaplan-Meier method was utilized for “time from detection of RV lead defect to revision”. Data were analyzed using IBM SPSS Statistics (Version 29.0) and shown as mean±Standard Deviation (SD), median with Quartiles (Q), or as count (n) with percentage (%). For measures of association, a difference of mean with a 95% confidence interval (CI) was applied. Depending on the variable type and question, we used Student’s t-test, chi-squared test or cohens’d, as appropriate. The Kaplan-Meier estimator using logrank test was applied to graphically compare time from detection of ICD dysfunction to revision. To reduce alpha error accumulation, the Bonferroni correction was applied.
Result
Patient characteristics of patients undergoing ICD revisions
Of 146 telemonitored patients from 2005 till 2023, 5 (3.4%) underwent revision for electrode defects, compared to 145 (4.7%) of 3056 conservatively monitored patients. The demographic data of the patients included in the patient collective with ICD revisions are shown in Table 1. The two groups did not differ in age (p=0.802) and BMI (p=0.758). While the telemedicine group consisted entirely of male patients, 22.1% of the patients in the control group were female (p=0.585). The age of the respective ICD lead at time of revision was 7.29 years (SD=5.44) in the conventional monitored group and 5.34 years (SD=4.66) in the telemetric monitored group (p=0.429). While no patient in the telemedicine group suffered from an inappropriate shock during the observed period, an inappropriate shock occurred in 11 patients in the conventionally monitored group (7.2%; p=0.792). The time interval between detection and revision was 30.89 days (SD=151.27 days) in the conventionally monitored group and 4.00 days (SD=47.00; p=0.692) in the telemetrically monitored group. In the conventionally followed group, 49% received an ICD for primary prophylactic reasons and 50.3% received one for secondary prophylaxis. In contrast, 80% of telemetrically monitored patients had a primary prophylactic ICD and only 20% had a secondary prophylactic one (p=0.393) (Table 2). Underlying cardiovascular diseases as reason for ICD implantation can be found in Table 2. 37.9% (p=0.375) of the conventionally monitored patients had a cardiomyopathy as an indication, which is further subdivided into DCM (22.8%), HNCM (3.4%) HOCM (2.8%), ICM (13.1%), NCCM (0.7%) and ARVC (0.7%). In the telemetric monitored group 60% had a cardiomyopathy, with 40% DCM and 20% ICM.
Table 1: Demographic table.
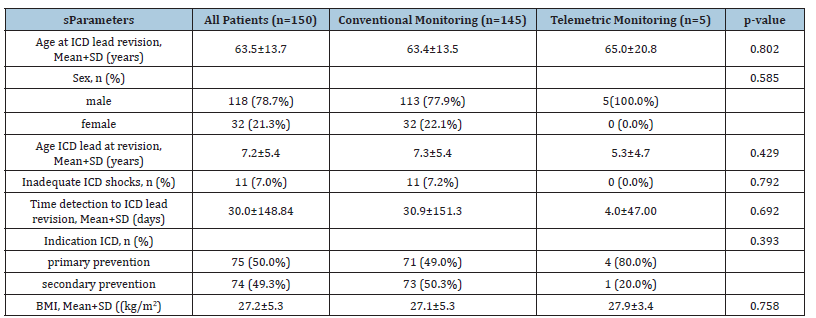
Notes: The p-value for nominally distributed variables was determined using Fisher’s exact test and the Chi-squared test, while for numerical variables, the student’s t-test was used. Abbreviations: SD, Standard Deviation, RV lead, Right Ventricular Lead; ICD, Implantable Cardioverter Defibrillator; BMI, Body Mass Index; CAD, Coronary Artery Disease.
Table 2:Underlying cardiovascular disease and ICD indication.
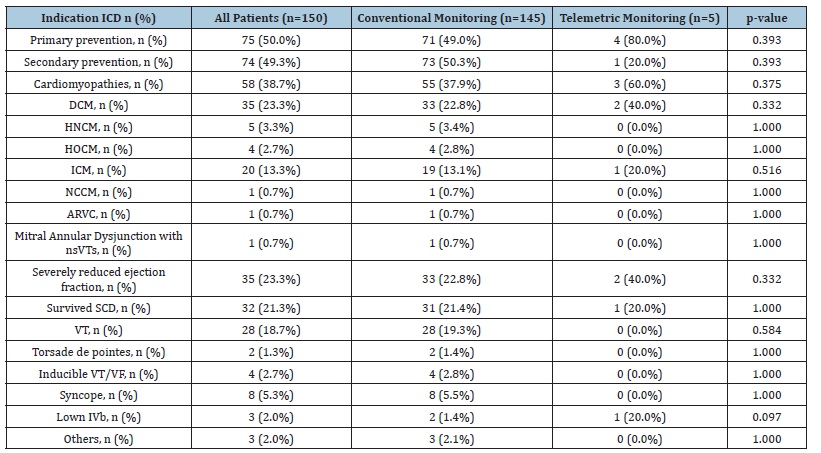
Notes: The p-value for primary and secondary prevention was determined using the Chi-squared test, while the p-values for the individual underlying conditions were calculated using Fisher’s exact test. Abbreviations: ICD, Implantable Cardioverter Defibrillator; DCM, Dilated Cardiomyopathy; HNCM, Hypertrophic Non-Obstructive Cardiomyopathy; HOCM, Hypertrophic Obstructive Cardiomyopathy; ICM, Ischemic Cardiomyopathy; NCCM, Non-Compaction Cardiomyopathy; nsVTs, Non-Sustained Ventricular Tachycardias; LVEF, Left Ventricular Ejection Fraction; VT, Ventricular Tachycardia; VF, Ventricular Fibrillation; ARVC, Arrhythmogenic Right Ventricular Cardiomyopathy.
Table 3 shows the manufacturers of the ICDs and the leads. No significant differences of the manufacturer types were seen in both groups (p=0.075). In the conventional monitored group 40.3% had an ICD from Medtronic, 37.6% from St. Jude medical/Abbott, 6.7% from Bortnick, 14.8% from Boston Scientific and 0.7% from Sorin Group. In the telemetric monitored group 40% had an ICD from St. Jude medical/Abbott and 60% from Boston Scientific. The ICD-leads were divided in RV lead and subcutaneous lead. The manufacturers of the RV-Leads were 42.8% from Medtronic, 27.6% of the RV leads were from St. Jude medical/Abbott, 11.8% by Bortnick, 12.5% by Boston Scientific and 0.7% from Sorin group in the conventional monitored group. In the telemetric group 20% of the RV leads were from Medtronic and 20% from St. Jude medical/Abbott. In the conventional group the subcutaneous lead was 0.7% from Boston Scientific, whereas 60% of the subcutaneous leads in the telemetric monitored group were from Boston Scientific (p=0.118). While in the telemetric group none of the patients had obtained a RA-lead, 62 patients (0.43%) in the conventional monitored group had one. 27.9% by Medtronic, 39.3% from St. Jude medical/Abbott, 11.5% by Bortnick, 16.4% by Boston Scientific and 1.6% by Sorin Group.
Table 3:Manufacturer of ICD and leads.
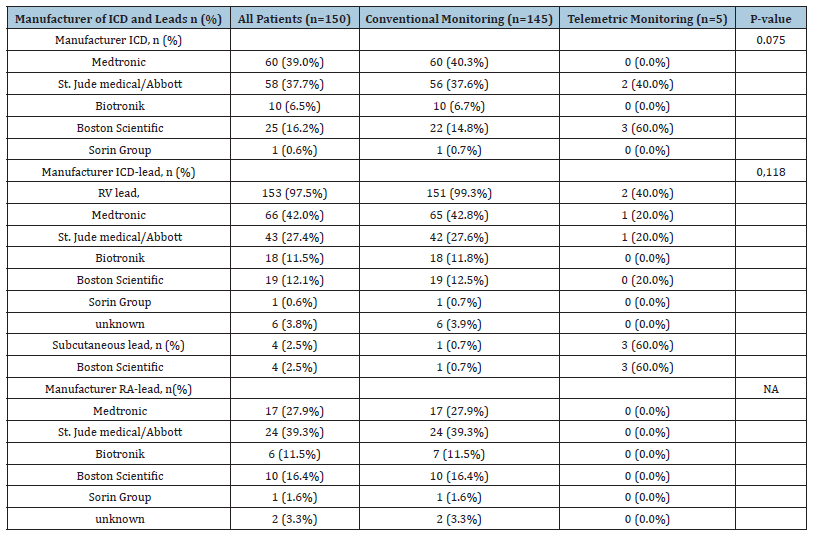
Notes: The p-value was determined using the Chi-squared test. Abbreviations: ICD, Implantable Cardioverter Defibrillator; RV lead, Right Ventricular lead; RA lead, Right Atrial lead; NA, Not Applicable.
Patients in telemonitoring
Patient numbers in active telemetric monitoring increased 0 to 109 from 2015 to 2023. A total of 146 patients were monitored during the observed period (Figure 1).
Figure 1:A. The numbers of ICD lead revisions per year from 2015-2023, B. Alive ICD-patients in telemetric monitoring from 2015-2023.

Clinical presentations of patients for ICD revisions
Most of the patients consulted for an ICD checkup because of a warning tone or vibration alarm (n=47 (29.9%); n=46 (30.3%)) in the conventional monitoring group and (n=1; 20.0%) in the telemetric monitoring group (p=0.622) (Table 4). The second most frequent reason was a diagnosis of lead dysfunction during a planned ICD interrogation (n=31; 20.4%) in the conventional monitoring group and (n=1; 20.0%) in the telemetric monitoring group (p=0.199), followed by more frequent in-house queries as a reason for presentation (n=22; 14.5%) in the conventional monitoring group and (n=1; 20.0%) in the telemetric monitoring group (p=0.983). An inadequate shock was the reason for emergency presentation for 6.4% of the patients (n=10; 6.6%) in the conventional monitoring group and none (n=0; 0%) in the telemetric monitoring group (p=0.553). An incidental diagnosis of lead dysfunction during generator change was present in 4.5% of cases (n=7; 4.5%) in the conventional monitoring group and none (n=0; 0%) in the telemetric monitoring group (p=0.623). In 2.5% of the patients an ICD malfunction was the reason for presentation (n=4; 2.6%) in the conventional monitoring group and none in the telemetric monitoring group (p=0.713). Other rarer causes for presentation can be found in Table 3.
Table 4:Reasons for presentation prior to ICD revision.
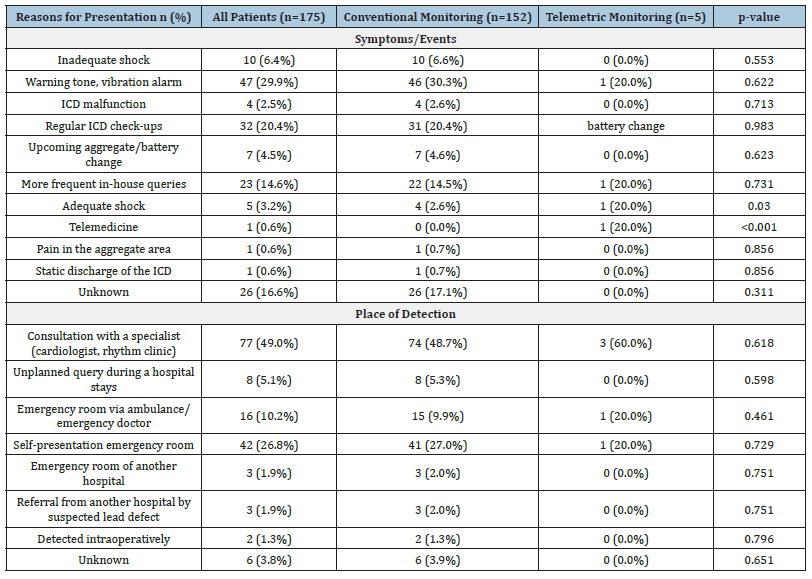
Notes:The p-value was determined using Fisher’s exact test. Abbreviations: ICD, Implantable Cardioverter Defibrillator.
The two groups differed significantly in the percentage of patients who went to a physician because of telemedicine (p<0.001; n=1 (0.6%)). Telemedicine was the reason for a presentation for 20.0% of the patients in the telemetric monitoring group (n=1) and for missing telemetric monitoring, obviously none in the conventional monitoring group. The second significant difference was an adequate shock as a reason for presentation (p=0.030). It was the initiator for 2.6% in the conventional monitoring group (n=4) and for 20.0% in the telemetric monitoring group (n=1). Table 4 also shows where the patients first present themselves. Most patients went to a consultation with a specialist (n=74; 48.7%) in the conventional monitoring group and (n=3; 60.0%) in the telemetric monitoring group (p=0.618). 26.8% (n=42) performed a self-presentation in an emergency room (n=41; 27.0%) in the conventional monitoring group and (n=1; 20.0%) in the telemetric monitoring group (p=0.729). The ICD revision indication was detected in an emergency room via ambulance or emergency doctor (n=15; 9.9%) in the conventional monitoring group and (n=1; 20.0%) in the telemetric monitoring group (p=0.461). At an unplanned query during the hospital stay 5.1% of the indications of ICD revisions got detected (n=8; 5.3%) in the conventional monitoring group and none (n=0; 0%) in the telemetric monitoring group (p=0.598). Other rarer modes of presentation can be found in Table 4.
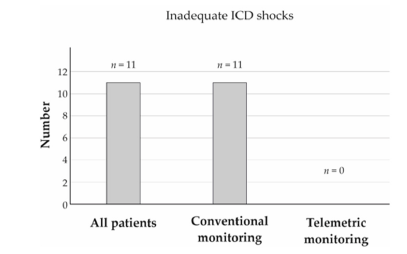
Inadequate shocks
Eleven patients in the control group (7.2%) and none in the telemonitored group experienced inappropriate shocks (p=0.792) as presented in Figure 2.
Figure 2: Number of inadequate ICD shocks divided into conventional monitored and telemetric monitored group.
Timing of lead revisions
The time from defect detection to revision was shorter in the telemonitored group (4.0 vs. 30.9 days, p=0.692) as shown in Figure 3.
Figure 3: The time from defect detection to revision was shorter in the telemonitored group.

Discussion
Patient characteristics
The demographic data of our retrospective patient collective was comparable to already published telemetric monitoring cohorts regarding sex and age. The patient population of this study consists of 78.7% male and 21.3% female, with a mean age of 63.5 years alike the patients of the French ECOST trial. 88.2% of the French patients were male, 11.8% female and the average age was 61.6 years. In the conventional group 77.9% were male and 22.1% female and the average were 63.43 years while in the ECOST trail it was 87.3% male and 12.7% female patients and an average of 62.0 years. In the telemetric monitored group, all our patients were male, and the average age were by 65.0 years while in the ECOST trial the patients were 89.2% male and 10.8% female with an average of 61.2 years [12]. The TRUST trials also show similar demographic data. The age in the conventional group was 64.0 vs 63.3 years in the telemetric monitored group. 73.1% patients were male in the conventional group versus 72.0% in the telemetric group [14]. The two groups did not differ significantly in the reasons for ICD implantation. In the control group 49.0% of the patients had a primary prevention ICD and 50.3% a secondary prevention ICD, while in the telemetric monitored group it was 80.0% primary prevention and 20.0% secondary prevention. In the ECOST trial the ratio was 53.8% primary vs 46.2% secondary in the conventional group and 53.3% versus 46.7% in the telemetric group [12].
Telemetric monitoring in Germany-development needed
In Germany many patients are sceptical about the technology and have concerns about the protection of their data [15]. The study also found that patients with secondary prophylactic indications mainly chose telemonitoring because of concerns about health issues [15]. Although our telemedicine patients mostly received primary prophylactic ICDs, the study suggests that there will be a further increase in telemedicine patients, which we have already seen starting in 2021 [16], While the telemetric monitoring of ICDs has already been recommended in Germany since 2013 [17]. According to Sandgren et al, there is no difference between primary prophylactic and secondary prophylactic ICDs regarding the number of inappropriate shocks [16]. Therefore, even if in future studies with telemedicine primarily treat ICDs implanted for secondary prophylactic purposes, conclusions can be drawn about the whole. Reimbursement issues in Germany so far also imposed a putative limiting factor in the implementation of telemonitoring.
Presentations and health care burden
29.9% of patients presented because of a warning tone and in 20.4% the defect was diagnosed during a regular interrogation. That is equivalent to the study of Vollmann et al. [18] where 30% of the dysfunctional ICD-leads were detected through patient alert [18]. Only 2.5% of all patients had symptoms or pain in the aggregate pocket. In 0.6% of our patients the lead dysfunction was diagnosed by telemonitoring alone before any alarm or symptoms could occur. The four remaining telemetric monitored patients had a shortened presentation interval due to increased RV thresholds or warnings from the manufacturers. According to the EVOLO study a device alarm does not necessarily lead to direct patient contact with healthcare services. Some patients are not capable of noticing the alarm. It has been shown that a median of 20 days after a warning signal is needed until access to healthcare services has taken place [19-21]. However, if the doctor contacts the patient because an unusual query was sent to him via telemedicine, it could lead to the patient being seen more quickly. Nishii et al. [22] demonstrated that 64.7% of implantable cardiological devices did not give a warning despite a defect [22]. Older generators with less eloquent algorithms possibly are unable to alarm the patient with every dysfunction of their system [23]. These problems can be addressed with telemonitoring since the physician can immediately contact the patient in case of a diagnosed dysfunction. For most patients, the first contact person was either the rhythm clinic or their cardiologist (49.0%). 26.8% presented to the emergency room and 10.2% used rescue services such as ambulances.
Inadequate ICD shocks
In total there were eleven inadequate shocks, none occurred in the telemetric monitored group. Although there is no statistically significant difference demonstrated in our retrospective patient cohort, it is remarkable that telemonitored patients had no inadequate shocks despite the rates of lead malfunction being approximately equivalent in both groups (3.42% of telemedicine patients versus 4.74% of all telemedicine patients). Therefore, both groups make up a similarly large proportion of their total population. The ECOST-Trial showed that the rate of inadequate shocks was reducible through telemetric monitoring [12]. The Health Quality Ontario was also able to show that telemedicine resulted in fewer inadequate shocks [24].
Time to revision
In terms of time from possible defect detection till revision, the median and average for the telemedicine group is 4 days, for the control group the median is 5 days and the average 30.89 days. However, the differences were not statistically significant due to sample size.
Summary
This study compared two groups of ICD patients in need of ICD lead revision, one monitored telemetrically and the other conventionally, focusing on revision rates, inappropriate shocks, and time to revision and subsequent health care system presentation. Patient demographics were similar between the two groups, with the telemetric group having a higher proportion of primary prophylactic ICDs. Although both groups had comparable lead malfunctions, the telemetric group had no inappropriate shocks, while 7.2% of the conventional group did. The time from defect detection to revision was significantly shorter in the telemetric group (4 days vs. 30.9 days), although this difference was not statistically significant. Overall, the study suggests that telemonitoring may lead to quicker revisions and fewer inappropriate shocks, with further adoption expected in Germany despite some patient scepticism and reimbursement challenges.
Limitations
This is a single center study. Data was collected and analyzed retrospectively. Secondly the groups differ in size, which may result in non-significant results. In addition, the percentage of S-ICD patients in the telemedicine group is higher than in the control group.
Conclusion
Remote monitoring reduced inappropriate shocks by enabling earlier detection of lead defects. Expanding telemonitoring may improve early detection and prevent inappropriate shocks.
Author Contributions
Conceptualization: P X, A K R; Methodology: P X, J A, A K R; Software: P X, J A, R R, A K R; Validation: P X, A K R; Formal Analysis: P X, J A, A K R; Investigation: P X, J A, C G, A K R; Resources: N F, P L, A K R; Data Curation: P X, J A, C G; Writing-Original Draft Preparation: P X, J A, A K R.; Writing-Review and Editing, P X, J A, R R, C G, E G, D T, P L, N F, A K R; Visualization: J A; Supervision: P X, J A, A K R; Project Administration, A K R; Funding Acquisition: A K R, P L, N F. “All authors have read and agreed to the published version of the manuscript.”
Statements and Declarations
i. Ethical considerations: Our study was conducted in accordance
with the ethical standards of the Declaration of Helsinki. The
local institutional review board (IRB) gave approval to this
study (ethics approval number: S-018/2023). It did not require
additional written informed consent for this observational
study as only routine clinical data were utilized.
ii. Consent to participate: Not applicable.
iii. Consent for publication: Not applicable.
iv. Declaration of conflicting interest: The authors declare no
conflict of interest.
v. Funding statement: This research was funded in parts by
Heidelberg University Medical School Olympia-Morata Grant
to AKR.
vi. Data Availability Statement: Raw data may be acquired from
the corresponding author on reasonable request.
vii. Institutional Review Board Statement: The institutional
review board (IRB) of Heidelberg University, Heidelberg,
Germany gave approval to this study (ethics approval number:
S-018/2023). It did not require additional consent for this
observational study as only routine clinical data were utilized.
viii. Informed Consent Statement: Not applicable.
ix. Acknowledgments: Not applicable.
Conflicts of Interest: The authors declare no conflict of interest.
References
- (2019) German Medical Association, National association of statutory health insurance physicians, Association of scientific medical societies. National care guideline chronic heart failure-long version (3rd Edn).
- Bestehorn K, Stolpe S (2022) Mortality and morbidity of heart disease-an overview. German Heart Report 2022, pp. 9-30.
- Priori SG, Blomström LC, Mazzanti A, Blom N, Borggrefe M, et al. (2015) 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. The task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European society of cardiology (ESC). Endorsed by: association for European paediatric and congenital cardiology (AEPC). Eur Heart J 36(41): 2793-2867.
- Tilz RR, Bosch R, Butter C, Kuck KH, Richter S, et al. (2022) Recommendations on lead extraction-joint recommendations of the German cardiac society (GCS) and the German society for thoracic and cardiovascular surgery (GSTCVS). The Cardiology 16(3): 213-232.
- Markewitz A (2021) Annual report 2018 of the German pacemaker and defibrillator registry-Part 2: Implantable cardioverter-defibrillators: Working group on cardiac pacemakers and cardioverter-defibrillators at IQTIG-Institute for quality assurance and transparency in healthcare. Pacemaker Electrophysiology 32(1): 75-88.
- (2017) Every ICD shock worsens the prognosis. Cardiovasc 17: 31.
- Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, et al. (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352(3): 225-237.
- The AVID Investigators (1997) A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med 337(22): 576-583.
- Kapa S, Rotondi TD, Mariano Z, Aves T, Irvine J, et al. (2010) Psychopathology in patients with ICDs over time: Results of a prospective study. Pacing Clin Electrophysiol 33: 198-208.
- Benninghoven D, Kunzendorf S, Heberlein I, Jantschek G (2006) Anxiety disorders in patients with implanted cardioverter-defibrillator (ICD). Psychotherapist 51: 206-213.
- Hauck M, Bauer A, Voss F, Weretka S, Katus HA, et al. (2009) Home monitoring for early detection of implantable cardioverter-defibrillator failure: A single-center prospective observational study. Clin Res Cardiol 98(1):19-24.
- Guédon ML, Lacroix D, Sadoul N, Clémenty J, Kouakam C, et al. (2013) A randomized study of remote follow-up of implantable cardioverter defibrillators: Safety and efficacy report of the ECOST trial. Eur Heart J 34(8): 605-614.
- Hindricks G, Varma N, Kacet S, Lewalter T, Søgaard P, et al. (2017) Daily remote monitoring of implantable cardioverter-defibrillators: Insights from the pooled patient-level data from three randomized controlled trials (IN-TIME, ECOST, TRUST). Eur Heart J 38(22): 1749-1755.
- Varma N, Michalski J, Epstein AE, Schweikert R (2010) Automatic remote monitoring of implantable cardioverter-defibrillator lead and generator performance: The Lumos-T safely reduces routine office device follow-up (TRUST) trial. Circ Arrhythm Electrophysiol 3(5): 428-436.
- König L, Grünberg E, Xynogalos P, Thomas D, Rivinius R, et al. (2023) Acceptance of telemetric care for patients with sICD safety advice: Qualitative interview study in cardiological health services research. Herzschr Elektrophys 34(2): 136-141.
- Sandgren E, Rorsman C, Engdahl J, Edvardsson N (2015) Low rate of and rapid attention to inappropriate ICD shocks with remote device and rhythm monitoring: A qualitative study. Open Heart 2(1): 1-7.
- Müller A, Rybak K, Klingenheben T, Schumacher B, Israel C, et al. (2013) Recommendations for telemonitoring in patients with implanted pacemakers, defibrillators and cardiac resynchronization systems. The cardiologist 7: 181-193.
- Vollmann D, Erdogan A, Himmrich E, Neuzner J, Becker D, et al. (2006) Patient alert for the detection of ICD lead failure. Europace 8(5): 371-376.
- Landolina M, Perego GB, Lunati M, Curnis A, Guenzati G, et al. (2012) Remote monitoring reduces healthcare use and improves quality of care in heart failure patients with implantable defibrillators: The evolution of management strategies of heart failure patients with implantable defibrillators (EVOLVO) study. Circulation 125(24): 2985-2992.
- Simons EC, Feigenblum DY, Nemirovsky D, Simons GR (2009) Alert tones are frequently inaudible among patients with implantable cardioverter-defibrillators. Pacing Clin Electrophysiol 32(10): 1272-1275.
- Knackstedt C, Mischke K, Schimpf T, Waringer J, Fache K, et al. (2008) Fluid content measurement in CHF decision-making. Pacing Clin Electrophysiol 31(8): 961-967.
- Nishii N, Miyoshi A, Kubo M, Miyamoto M, Morimoto Y, et al. (2018) Analysis of arrhythmic events is useful to detect lead failure earlier in patients followed by remote monitoring. J Cardiovasc Electrophysiol 29(3): 463-470.
- Lovelock JD, Cruz C, Hoskins MH, Jones P, El CMF, et al. (2014) Generator replacement is associated with an increased rate of ICD lead alerts. Heart Rhythm 11(10): 1785-1789.
- Health Quality Ontario (2018) Remote monitoring of implantable cardioverter-defibrillators, cardiac resynchronization therapy and permanent pacemakers: A health technology assessment. Ont Health Technol Assess Ser 18(7): 1-199.
© 2025 Ann-Kathrin Rahm. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






