- Submissions

Full Text
Trends in Telemedicine & E-health
Characterizing the Components of Telehealth Programs for Opioid Use Disorder in East Tennessee
Jacob Powell, Laura Hunt Trull* and Cory Whitfield
East Tennessee State University, United States
*Corresponding author:Laura Hunt Trull, East Tennessee State University, Tennessee, United States
Submission: October 01, 2025;Published: October 16, 2025

ISSN: 2689-2707 Volume 6 Issue 1
Abstract
Since the COVID-19 pandemic, telehealth has remained popular as a treatment tool for Opioid Use Disorder (OUD). Telehealth can decrease barriers to access OUD treatment, especially in rural areas. There is limited data, however, on the specific components of telehealth programs and how these components vary across treatment facilities. The purpose of this study was to describe the patterns of telehealth services among OUD providers in East Tennessee. Specifically, this study identified components-such as group telehealth, virtual intake, and virtual drug screening- that are variably implemented among OUD treatment facilities. We conducted a cross-sectional observational study identifying eligible OUD treatment providers in East Tennessee. Organizations were contacted directly via telephone interviews to assess telehealth availability and components. A scoring system was derived categorizing facilities based on their degree of telehealth adoption and availability. The completed facility interviews demonstrate substantial variation in components of different telehealth programs. Particularly, the adoption of group telehealth, virtual intake, and virtual drug screening is not uniform across treatment facilities in East Tennessee. This research clarifies how telehealth is used for OUD treatment across East Tennessee. Beyond simply assessing availability, the study seeks to push the conversation about OUD towards a more nuanced understanding of the key components of programs.
Keywords:Telehealth; Opioid use disorder; East Tennessee; Geographic access; Substance use treatment; Rural health
Abbreviations:OUD: Opioid Use Disorder; MOUD: Medication for Opioid Use Disorder; SAMHSA: Substance Abuse and Mental Health Services Administration; MAT: Medicated Assisted Treatment; IRB: Institution Review Board; DUI: Driving Under the Influence
Introduction
Opioid Use Disorder (OUD) remains a pressing public health concern, and telehealth has emerged as a promising treatment intervention. When implemented, telehealth has been shown to have similar outcomes among patients with substance use disorders [1]. Additionally, telehealth-based Medication for Opioid Use Disorder (MOUD) programs demonstrate similar outcomes to office based MOUD programs [2]. The use of telehealth for substance use disorder also yields high overall satisfaction and provider-patient relationship [3]. Given comparable outcomes and satisfaction, telehealth shows promise because of its ability to help overcome barriers to treatment. Barriers that are addressed by telehealth include transportation, flexibility, and ability to receive maintenance medication [4]. These factors are especially prevalent in a rural environment, and it has been shown that telehealth used to deliver MOUD increases access and retention in rural areas [5]. While telehealth is recognized as potentially effective treatment modality for OUD, little is known about what aspects of a telehealth program make it effective. In fact, there is little standardization among telehealth implementation for OUD treatment. In 2022, Fledderman characterized that “There is little standardization across telehealth MOUD programs, with variability in visit structure, technology platforms, and incorporation of additional support services” [6]. Little has been done to characterize the differences between telehealth programs for OUD treatment. This lack of understanding makes a truly dynamic analysis of patient outcomes difficult to obtain. The purpose of this study is to examine the landscape of OUD telehealth programs in East Tennessee. East Tennessee functions as an effective region for this study as it has been disproportionately affected by OUD [7]. Furthermore, this study seeks to characterize relevant features of an OUD telehealth program that vary from facility to facility. In doing so, this project may lay the groundwork for future investigations on best practice for OUD telehealth and positive patient outcomes.
Methods
This project was a cross-sectional study intended to assess/ observe the use of telehealth services as a modality for Opioid Use Disorder (OUD) in East Tennessee. Treatment facilities included in this project were identified by using a national database (SAMHSA) [8]. Facilities that were labeled as either “Substance Use” or “Opioid Treatment Programs” by SAMHSA were included in the study. Facilities were identified by searching for “Substance Use” and “Opioid Treatment Programs” in each of the 33 counties of East Tennessee as defined by the TN Department of General Services Grand Divisions of Tennessee [9]. From May to July 2025, facilities were contacted via phone by a trained medical student. A list of questions was developed, and a consistent set of core questions guided each interview. If the facility did implement telehealth, an interview typically ranged from 5 to 20 minutes. After contacting 101 facilities, it was determined that responses were reaching a point of saturation, and telephone interviews were ceased. The IRB was consulted and determined that, because participants were not discussing personal experiences, the project did not qualify as human subject’s research. In order to categorize the prevalence of telehealth use at these facilities, a scoring system was devised. A telehealth adoption scoring system from 0-6 was devised with a point being awarded for each of the following criteria:
i. 1 point if the facility utilized telehealth in any way
regarding OUD treatment
ii. 1 point if the facility utilized telehealth with a form of
group therapy
iii. 1 point if the facility utilized telehealth in concurrence
with a medication assisted treatment (MAT) program
iv. 1 point if telehealth was utilized for the intake of new
patients (i.e. no in-person physical exam)
v. 1 point if drug screens were performed with telehealth
vi. 1 point if there was no waiting list to access telehealth
services.
This scoring system was established as a way to compare levels of telehealth adoption among different facilities but was not designed to provide insight on the effectiveness of a telehealth program. While awarding points to a facility for not having a waiting list to utilize telehealth may seem like an evaluation of effectiveness, it was determined that the absence of a waiting list could be evaluated as a commitment to operating a robust telehealth program. Logic presumed that operating without a waiting list required adopting adequate telehealth staff and hardware to meet demand. Following data acquisition custom maps were created using Google My Maps [10] using information gathered from interviews in combination with population data from the United States Census Bureau [11] Data was processed, and histograms were created using R [12].
Result
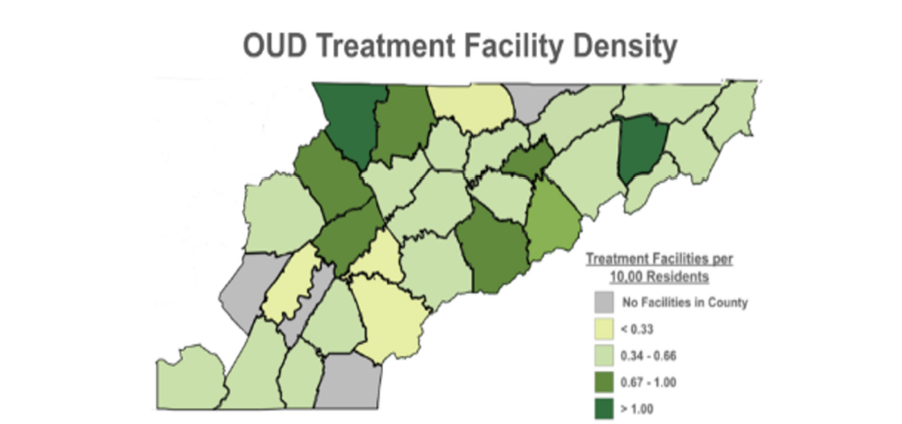
Based on selection criteria, 135 facilities were identified to be included in the study. Out of the 135 available facilities, 1 was permanently closed, and 2 were excluded due to having a primary focus on DUI remediation and driving instruction. The general distribution of the 133 eligible facilities was characterized and found to be roughly distributed in congruence with the population of East Tennessee (Figure 1-3). Of the 133 remaining facilities, contact was attempted with 101 before saturation was determined. Among those contacted, several were lost to follow up or denied request to interview, and full telephone interview ultimately yielded complete information for 30 facilities. Among those facilities, 28 were utilizing telehealth in some capacity at the time of the interview. Excluding the 2 facilities not utilizing telehealth, which would result in a score of 0, both the average and median telehealth adoption scores were 4 with a range from 1-6 (Figure 4). The majority (18) of OUD services interviewed received a score of 4. There was considerable variation among the adoption of various components of telehealth (Figure 5). The most common element of telehealth adopted was the use of telehealth in connection with a MAT program with 92.86% adoption rate. The least adopted element of telehealth was telehealth drug screening with a 17.86% adoption rate. Group telehealth (82.14%), telehealth intake (67.86%), and no wait list (46.43%) were adopted at varying levels.
Discussion
The design of this research study revealed several difficulties associated with obtaining information from OUD treatment facilities. In many instances, the number associated with a facility on SAMHSA was no longer in service. Once contact was made with a facility, there was no clear solution for finding an individual who would be willing or able to participate in an interview. On several occasions, the initial contact agreed to follow up with information yet never did. Different organizations operated at different scales, and some attempts to contact involved transfer to state or national corporate offices. These aspects increased the difficulty of pinpointing relevant information and highlighted the lack of standardization among OUD treatment facilities. When examining the distribution of OUD treatment facilities in East Tennessee, the pattern first appears as expected. The region’s population is concentrated around three metropolitan areas (Figure 1). Accordingly, most treatment facilities are located in or near these population centers (Figure 2). However, a higher number of facilities in a county does not necessarily translate to better access to care. There was not an obvious visual association between treatment facilities per 10,000 residents and total number of facilities (Figure 3). When adjusted for population, some densely populated counties still show signs of strain in treatment capacity, suggesting that the raw number of facilities does not reflect true accessibility. Importantly, it presents evidence against framing telehealth use as only a rural solution and provides further insight into why telehealth for OUD remains prevalent even after COVID. If urban and suburban regions struggle to meet physical demand, expansion of telehealth infrastructure may be considered a necessary way to treat patients. The analysis of all three maps in conjunction illustrates that all landscapes, including nonrural areas, may stand to gain benefit from refinement and further study of telehealth implementation.
Figure 1: Population total by county in East Tennessee. Counties are shaded from light green to dark green based on the total number of residents living in the county, with darker shades indicating higher populations.
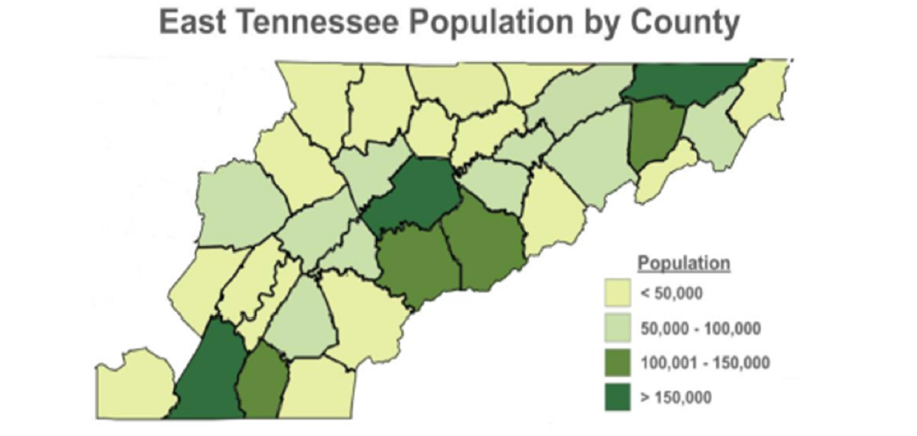
Figure 2: Distribution of OUD treatment facilities by county in East Tennessee. Counties are shaded from light green to dark green based on the total number of facilities located within the county, with darker shades indicating more facilities.
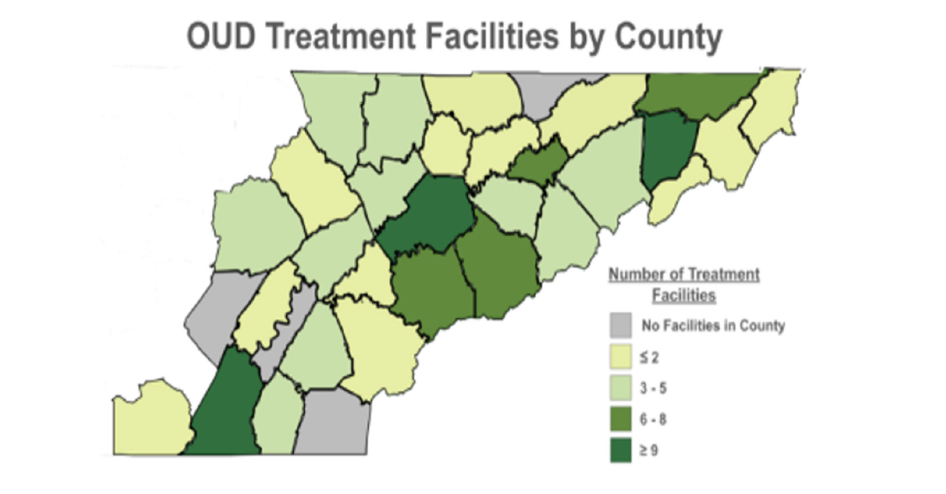
Figure 3: Density of OUD treatment facilities relative county population. Counties are shaded from light green to dark green based on the number of treatment facilities per 10,000 residents, with darker shades indicating a higher density of facilities.
Overwhelmingly, the most common telehealth adoption score received was 4/6 (Figure 4). This information might lead to hasty generalizations that adoption of telehealth programs among OUD treatment providers is homogenous. However, deeper analysis reveals that while telehealth is being adopted in a seemingly uniform manner, the individual components of a telehealth program vary by facility. There is wide variability among the adoption of individual elements of telehealth (Figure 5), and this variability demonstrates that a score of 4 may represent very different program structures and implementation. Taken as a whole, the data suggests that measuring whether telehealth is being used fails to capture the nuance of how it is implemented. Furthermore, the variability among telehealth implementation extends beyond data observation. Qualitative analysis of the telephone interviews revealed that genuine philosophical differences persist regarding telehealth best practice. The telephone interviews displayed the stark contrast of philosophies and guidelines regarding telehealth implementation persist among OUD treatment facilities. This is exacerbated by a lack of coordination between facilities. This idea was exemplified by one interviewee who conveyed doubts that the study would yield any groups utilizing telehealth to a high degree. These factors lead to markedly different attitudes, opinions, and telehealth implementation plans that were encountered during the interviews.
Figure 4: Histogram of telehealth adoption scores among OUD treatment providers interviewed in East Tennessee. Only facilities offering telehealth services were included, resulting in scores ranging from 1 to 6. Higher scores indicate more comprehensive adoption of telehealth components.
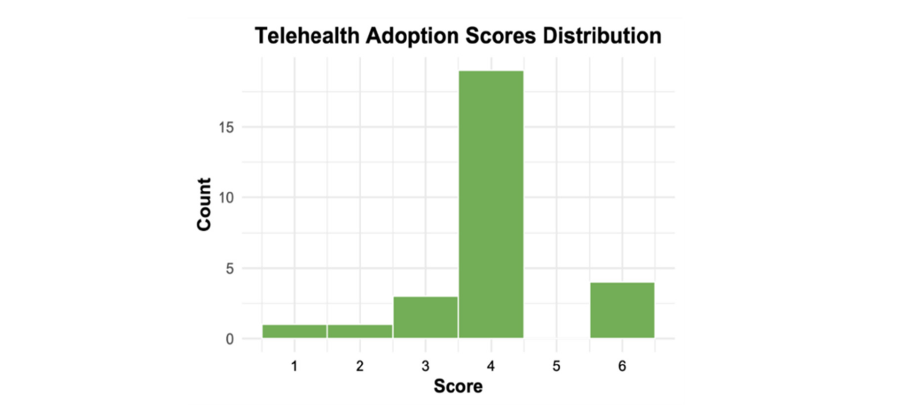
Figure 5: Prevalence of telehealth components among OUD telehealth treatment providers in East Tennessee. Bars represent the percentage of facilities offering each component. Percentages are displayed above each bar. Components include group telehealth sessions, Medication-Assisted Treatment (MAT) via telehealth, no wait time for telehealth appointments, telehealth intake processes, and telehealth drug screening.
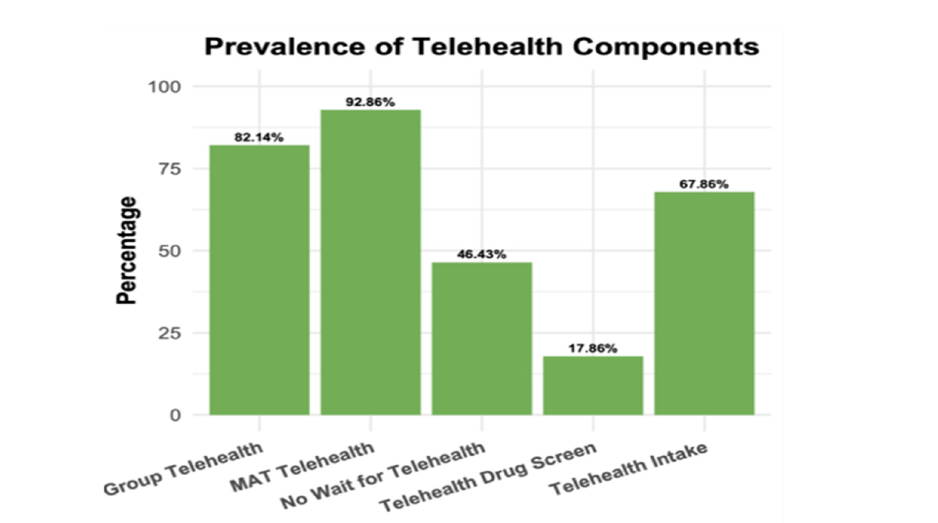
A noted difference among OUD telehealth services was the debate to make both the intake process and drug screen aspect of the program available to be completed virtually. To the programs who incorporated telehealth into the intake or drug screening process, the goal was to maximize patient participation. For these institutions, there was a philosophical priority placed on increasing patient convenience and comfort to increase patient participation. On the other hand, organizations that did not include a telehealth intake or drug screens often cited the exclusion of these aspects of a telehealth program as a safeguard to uphold compliance to protocol. One interviewee at an organization with no telehealth drug screening shared an anecdote of a new patient who informed the staff that he had re-used the same picture of a drug screen and submitted this image virtually for several months as a patient at a previous organization. It is worth noting that interviewees on both sides of this issue contended that they believed their respective policies were best for patient outcomes, demonstrating a lack of available evidence-based guidelines. Another difference among OUD treatment organizations was the choice to offer group therapy modalities via telehealth. Some interviewees were adamant that group therapy via telehealth is logistically unfeasible due to privacy concerns. Other interviewees contended that group therapy, including when delivered by a telehealth modality, was one of the most important parts of the treatment plan. This disparity further supports the notion that telehealth as an OUD treatment tool cannot be treated as a monolith. Knowing that an organization provides telehealth services does not provide sufficient information as to what type of service is being provided. To meaningfully advance the conversation about the efficacy and policy surrounding telehealth, the conversation must move beyond a binary yes/no framework and examine how these variable components of telehealth implementation affect patient outcomes.
Limitations
As with any cross-sectional design, this study has several limitations that should be considered during interpretation. First, data acquisition relied on publicly available information from the internet and student-led interviews. While a practical method for a broad sample, this approach may have introduced inconsistencies due to outdated online information, variable knowledge by staff interviewees, and willingness to respond. Furthermore, several facilities could not be reached or never responded to follow up, potentially introducing selection bias among the results. Additionally, while variable components of telehealth implementation were identified, the absence of patient data and outcomes limits the scope of this study. This study does not allow any conclusions to be drawn on the functionality or efficacy of specific telehealth components. Moreover, while the scoring system was synthesized to be logically structured, it has not been validated and may be subject to expansion or change in future research. Finally, this project is limited to East Tennessee and may not reflect telehealth implementation patterns in other geographic regions. Despite these limitations, this study provides an important foundation for understanding the landscape of telehealth adoption in OUD treatment and highlights critical areas for future investigation and policy development.
Conclusion and Recommendations for Future Research
In the future, studies should look to compare the presence or absence of specific components of a telehealth program to patient outcomes. This may be accomplished in the form of multivariable regression between components of telehealth and patient outcomes. Furthermore, the relationship between funding and staffing at a facility and the ability to execute various components of a telehealth program should be explored. In addition, this work should be expanded to other regions of the country keeping in mind the possibility that there are other key components of telehealth implementation that have not yet been characterized. Ultimately, this study should serve as a foundational groundwork to explore the best practices for establishing and implementing the best practices for structuring and implementing telehealth in the domain of OUD treatment.
Funding Statements
The first author has received a small research stipend from the College of Medicine. The remaining authors received no financial support for the research, authorship, and/or publication of this article.
References
- Gallagher JR, Krishnan SD, Chartrand JM, Parks MJ, Ngo Q, et al. (2025) Comparing abstinence, peer support, and quality of life among patients receiving virtual and in-person substance use disorder treatment: A six-month follow-up study. Alcohol Treat Q 43(2): 132-143.
- Weintraub E, Seneviratne C, Anane J, Coble K, Magidson J, et al. (2021) Mobile telemedicine for buprenorphine treatment in rural populations with opioid use disorder. JAMA Netw Open 4(8): e2118487.
- Hendy L, Olguin A, Jimes C, Barrett E, Coffey MJ, et al. (2025) Satisfaction with telehealth treatment for opioid use disorder among individuals living in rural and nonrural areas. Telemed J E-Health 31(8): 1039-1046.
- Monico LB, Eastlick M, Michero D, Pielsticker P, Glasner S (2025) Overcoming barriers to traditional care delivery and pharmacy challenges: a qualitative study of buprenorphine, telehealth, and a digital therapeutic for opioid use disorder. Subst Abuse Treat Prev Policy 20(1): 8.
- Meyers K, Herman S, Schuler H, Mun C, Bresani E, et al. (2025) The opioid epidemic in rural communities: Can telehealth increase access to medications for opioid use disorder and offset barriers to care? Drug Alcohol Depend 271: 112628.
- Fleddermann K, Chwastiak L, Fortier A, Gotham H, Murphy A, et al. (2025) Levels of telehealth use, perceived usefulness, and ease of use in behavioral healthcare organizations after the covid-19 pandemic. J Behav Health Serv Res 52(1): 48-63.
- Schwartz AN, Buchanan ZV, Meschke LL (2022) Community strengths and challenges related to opioid use disorder in rural counties of east Tennessee. J Appalach Health 4(1): 20-30.
- (2025) FindTreatment.gov.
- TN department of general services. Grand Divisions of Tennessee.
- (2025) Google My Maps.
- Bureau UC (2025) County population totals and components of change: 2020-2024. United States Census Bureau.
- (2025) An introduction to R.
© 2025 Laura Hunt Trull. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






