- Submissions

Full Text
Trends in Telemedicine & E-health
Telemedicine in Bangladesh: Transforming Patient Care in the Digital Age
Nusrat Kamal*
Department of Paediatrics, National Center for Control of Rheumatic Fever and heart Diseases, Bangladesh
*Corresponding author:Nusrat Kamal, Junior Consultant, Department of Paediatrics, National Center for Control of Rheumatic Fever and heart Diseases, Bangladesh
Submission: September 02, 2025;Published: September 18, 2025

ISSN: 2689-2707 Volume 5 Issue 5
Abstract
Telemedicine has emerged as a promising solution to address the significant disparities in healthcare access and quality in Bangladesh, particularly for the large, underserved rural population. Despite early, limited efforts, the COVID-19 pandemic catalysed a surge in telemedicine adoption, demonstrating its potential for remote consultations, especially during outbreaks where social distancing is crucial. This paper provides an overview of telemedicine in Bangladesh, highlighting its benefits, outlining key challenges, and discussing the future outlook based on recent developments and research findings. This review found that telemedicine offers considerable benefits, including reduced travel time and costs, enhanced convenience, and improved access to specialist care for patients in remote areas.
Keywords:Telemedicine; Telemedicine Bangladesh; Rural healthcare; E-Healthcare; Digital health Bangladesh; Remote healthcare Bangladesh
Introduction
Bangladesh, officially the People’s Republic of Bangladesh, is a South Asian country located on Bay of Bengal. With a population exceeding 170 million [1], it is one of the most densely populated nations in the world where rural population is 68.34% according to Bangladesh Census, 2022 [2]. In recent years, Bangladesh has embraced digitalization, industrial growth, and global trade, positioning itself as a rising economy often termed the “Asian Tiger in the making.” Telemedicine/Telehealth/E-health is the most prominent and visible E-business service and a blessing of Information and Communication Technologies (ICT). Telemedicine is sometimes used as a synonym to telehealth. Although WHO uses telemedicine to describe all aspects of health care including preventive care, many organizations use the term ‘telemedicine’ only to describe remote clinical services and’ telehealth’ to include nonclinical applications like administration and provider education and health information for the common people [3]. In rural regions where specialists are scarce, telemedicine enables patients to consult with doctors remotely, overcoming geographical barriers. Although use of telemedicine is not new, even not in Bangladesh; this particularly gained attention during the pandemic, as telemedicine reduces person-to-person contact, minimizing the risk of virus exposure for both patients and healthcare providers. Despite notable progress in public health, several gaps persist in accessibility, affordability, and quality of medical services. Telemedicine has emerged as a viable solution to bridge these differences. Bangladesh has one of the highest population densities in the world, yet its doctor-to-patient ratio remains below WHO recommendations. Being one of highest population density country with limited health resources and clear urban-rural disparity, telemedicine offers a way to optimize limited human resources by extending specialist consultations to underserved areas.
Out-of-pocket expenditure remains the primary mode of healthcare financing in Bangladesh, leading to financial strain for many households. There is also Rising Burden of Non-Communicable Diseases (NCDs). However, during COVID-19 pandemic, citizen has availed the importance of telemedicine as a safe, efficient, and scalable solution for maintaining essential healthcare while minimizing infection risks. It has accelerated digital health adoption and proved its relevance for future health crises. Widespread use of mobile phones, and the government’s “Digital Bangladesh” vision, the infrastructure for telemedicine is steadily expanding. This provides a strong foundation for integrating telemedicine into the national health system. Telemedicine is not just an option but a necessity for Bangladesh to overcome geographical, economic, and infrastructural barriers in healthcare, while also preparing the system for future public health challenges. In Bangladesh, providing in-person health care is challenging, particularly given the existing financial constraints, limited number of specialist doctor, limited resources and hard to reach locations particularly in the hilly areas and islands. One of the major advantages of telemedicine can be for saving of cost and effort especially of rural patients, as they need not travel long distances for obtaining consultation and treatment. Additionally, it will reduce the inconvenience and bad impact to family and social factors. In this article, I have described the importance of telemedicine service in Bangladesh, basis of sudden flourishment, the barriers and challenges that the country is facing to implement this approach and the strategies to overcome these barriers in this developing country.
History of Telemedicine in Bangladesh
It started around mid-to-late 1999.
1999: Telemedicine emerged in Bangladesh with the Swinfen
Charitable Trust, establishing one of the first telemedicine links for
remote treatment.
2001: The Bangladesh Telemedicine Association (BTA) was
founded.
2003: The Sustainable Development Network Program (SDNP)
Bangladesh began its e-HL project, connecting regional nodes to
satellite for diagnostic support.
2005: Grameen Telecom (GTC) and DAB launched formal
telemedicine services, linking Faridpur General Hospital to
specialist doctors in Dhaka through video conferencing.
2012: Laptops were distributed to community clinics to support
telemedicine and health data management.
2016: The National Telehealth services is known as
‘ShasthyoBatayon16263’ that was inaugurated [4].
2020: Bangladesh Medical and Dental Council (BMDC) issued
Telemedicine Guidelines in July 2020, in accordance with the
BM&DC Act, 2010, to regulate telemedicine practices by registered
medical doctors.
The Growth Path of Telemedicine in Bangladesh
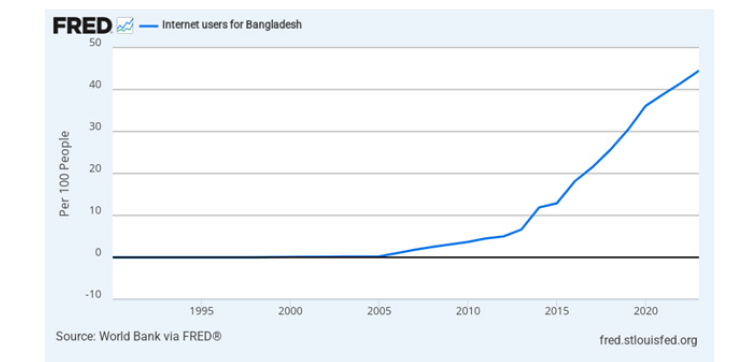
As time has progressed, internet reach and smart phone use in Bangladesh have increased and that has eventually made the ecosystem better and more accessible for both service providers and customers. Smart phone usage has been significant growth showing 72.8% of households using smart phones in late 2023, up from 63.3% in previous year [5]. A total of 185 million cellular mobile phone connections were active in early 2025 in Bangladesh which shown 106% of total population and during that time, there were 77.7 million individuals using the internet [6,7]. The graph highlights a slow initial uptake, followed by rapid acceleration from the 2010s onward (Figure 1), and steady growth in the early 2020s, reflecting expanding infrastructure, mobile internet adoption, and digital inclusion efforts.
Figure 1: Bioinformatics of genomic material.
Bangladesh Perspective
In accordance with the BM&DC Act, 2010-
Who can provide Tele medicine
A registered medical doctor is a person who holds the degree- MBBS/BDS and is registered with Bangladesh Medical and Dental Council in accordance with the Bangladesh Medical and Dental Council Act 61, 2010.
Tools for Telemedicine
Doctors may use any telemedicine tool suitable for carrying out technology-based patient consultation e.g. telephone, video, devices connected over LAN, WAN, internet, mobile or landline phones. Chat platforms like WhatsApp, Facebook Messenger, or mobile apps or internet based digital platforms for telemedicine or data transmission systems like e-mail/Skype/fax etc. Irrespective of the tool of communication used, the core principles remain the same.
Types of Tele health Services
There are various types of telehealth services available
including:
a. Live video conferencing: Facilitates real-time video
consultations between patients and physicians.
b. Asynchronous video (store-and-forward): Permits
patients to transmit their health records and obtain
consultations from physicians remotely.
c. Remote Patient Monitoring (RPM): Facilitates healthcare
providers in overseeing patients’ vital signs and health
conditions from a distance.
d. Mobile Health (mHealth): Employs mobile devices and
health-oriented
Seven Elements to be considered in any telemedicine
consultationi.
Context
ii. Identification of Registered Medical Doctor and Patient
iii. Mode of Communication
iv. Consent
v. Type of Consultation
vi. Patient Evaluation
vii. Patient Management
Consent
Patient consent Patient consent is necessary for any tele medicine consultation. The consent must be explicit. Patient can send an email, text or audio/video message. Patient can state his/her intent on audio/video platform to the Registered Medical Doctor (e.g. “Yes, I consent to avail consultation via tele medicine” or any such communication in simple words). The Registered Medical Doctor must record this in his patient records. A prescribed form that is given in annexure will serve the purpose better.
Types of consultation
There are two types of patient consultations, namely, first consult and the follow-up consult.
Patient management
Based on physician’s Judgement, it could be health education,
counselling & medication.
Health education: These could be related to diet, physical
activity, cessation of smoking, contagious infections and so on.
Likewise, s/he may give advice on immunizations, exercises,
hygiene practices, mosquito control etc.
Counselling: This is specific advice given to patients and it
may, for instance, include food restrictions, dos and don’ts for
a patient on anticancer drugs, proper use of a hearing aid, home
physiotherapy, etc to mitigate the underlying condition. This may
also include advice for new investigations that need to be carried
out before the next consult.
Prescribing medicines
Prescribing medications, via telemedicine consultation is at the professional discretion of the Registered Medical Doctor. It entails the same professional accountability as in the traditional in-person consult. If a medical condition requires a particular protocol to diagnose and prescribe as in a case of in-person consult then the same prevailing principle will be applicable to a telemedicine consult. Registered Medical Doctor may prescribe medicines via telemedicine only when Registered Medical Doctor is satisfied that s/he has gathered adequate and relevant information about the patient. There are certain limitations on prescribing medicines on consult via telemedicine depending upon the type of consultation and mode of consultatio.
Framework for practicing telemedicine in 4 scenarios
a. Patient to Registered Medical Doctor
b. Health Worker to Registered Medical Doctor
c. Registered Medical Doctor to Registered Medical Doctor
d. Emergency Situations
Sectors of telemedicine services
Although different medical and surgical branches have gained such advancement in technology, that almost all branches can provide telemedicine service in some extent. In Bangladesh, among branches of medicine- Tele-cardiology, Tele-ophthalmology, Teleradiology, Tele-pathology, Tele-rehabilitation are gaining popularity.
Operating Market Actors
Both government and non-government projects are active in delivering telemedicine to patients all over the country.
Government initiatives
Citizens can take health suggestions for free now from doctors working in government health centres. For this a mobile phone has been given to each district and sub-district hospital of Bangladesh. The numbers of these mobile phones have been publicized locally. Doctors receive calls in these numbers 24 hours. Under the Directorate General of Health Services (DGHS), high-quality telemedicine services have been established at 2 specialized hospitals (Bangabandhu Sheikh Mujib Medical University and National Institute of Cardiovascular Diseases), 3 district hospitals (Shatkhira, Nilphamari, and Gopalganj) and 3 sub-district hospitals (Pirgonj, Dakope, and Debhata) [8]. Additionally, webcams have been given in each sub-district, district, medical college, and postgraduate institute hospitals. The service enables patients admitted at districts and sub-district levels to take advice and suggestions from specialists through telephone and webcam services.
Private sectors initiatives
Now a days almost all clinics, hospitals, private medical colleges,
telecom services are providing telemedicine service in some extent.
Physicians are also using telemedicine as a part of their private
practices. Some recommended examples could bea.
Tonic Dakter- Grameen phone offers telehealth services
through a platform called Tonic, which provides access to an
in-house clinical team and health content from institutions
like Mayo Clinic. By dialing *789# from their Grameen phone
mobile [9].
b. “Jeeon” has been one of the key players in the telemedicine
industry for some too. They entered the market by signing
an agreement with Paperfly. Paperfly will deliver life-saving
medicine to remote areas pharmacies of the country as a
partner of Jeeon. Currently, Jeeon has 2084 pharmacies in their
network with a countrywide distribution channel [10].
c. Aponjon provides a mobile health service. The Aponjon
mHealth program, a USAID effort in Bangladesh sponsored
by the Mobility Alliance for Maternity Action (MAMA) had
undergone a successful test [11].
d. Other like Zaynax Health, Sebaghar, DOCTIME, Sasthy
sheba are gaining much popularity.
Challenges
Key challenges for telemedicine in Bangladesh include a poor digital infrastructure, low digital literacy among patients and providers, and underdeveloped policy and regulatory frameworks. These issues are amplified in rural areas, where limited access to high-speed internet and high-quality equipment impedes effective service delivery.
Infrastructural and technological barriers
a. Poor internet connectivity: Many rural areas suffer
from unreliable and slow internet, making high-quality video
consultations difficult and hindering the widespread adoption
of telemedicine.
b. Insufficient equipment: Early telemedicine projects
struggled with hardware failures, poor camera performance,
and inconsistent power supply. Consistent, stable hardware
and software are critical for reliable service.
c. Cost of technology: The financial investment required
for ICT infrastructure and specialized medical devices is
a significant hurdle for providers, especially in resourceconstrained
settings.
d. Lack of unified systems: Disparate and non-interoperable
technology platforms prevent a national-level, seamless
integration of patient data, such as Electronic Health Records
(EHR).
Regulatory and legal issues
a. Data privacy and security concerns: The potential for
mishandling sensitive patient data raises significant concerns
about privacy and security, undermining patient trust in digital
health platforms.
b. Reimbursement policies: Unclear policies regarding
reimbursement for telemedicine consultations deter healthcare
providers from fully adopting digital services.
Socioeconomic and cultural barriers
a. Limited digital literacy: A significant portion of the
population, particularly in rural and low-income areas, lacks
the digital literacy to use telemedicine platforms effectively.
b. Lack of trust in digital healthcare: Many people remain
hesitant to use telemedicine because they do not believe a
virtual consultation can be as effective as a traditional, inperson
visit. This is a cultural barrier that requires targeted
marketing and successful case studies to overcome.
c. Resistance from health providers: Some healthcare
professionals are resistant to changing established practices
and lack the motivation or skills to use new telemedicine
technologies.
d. Patient dissatisfaction: Poor quality of care, a lack of
awareness about the technology, and the absence of reputed
doctors on some platforms can lead to patient dissatisfaction
and distrust.
Operational challenges
a. Funding and sustainability: Initial pilot projects often fail
due to a lack of sustainable financial support. Over-reliance
on donor funding, as with the USAID cuts to a major program,
makes projects vulnerable.
b. Shortage of trained personnel: There is a scarcity of
personnel trained to operate and manage telemedicine
systems, including IT specialists and medical staff proficient in
telehealth.
c. Scalability for rural areas: Most successful telemedicine
services have focused on urban areas where the infrastructure
and consumer base are more developed. Expanding into remote
and underserved areas is a significant long-term challenge.
Future Recommendations
Strengthen regulatory framework & quality standards
a. Transform draft frameworks into enforceable laws to
ensure consistent practice and patient safety, as highlighted by
health leaders.
b. Define e-health standards for consultations, prescriptions,
data privacy, and professional liability to build public trust and
institutional credibility.
Invest heavily in digital infrastructure Enhance digital literacy through education & training
a. Launch targeted digital literacy programs for both patients
and healthcare providers, especially in rural communities.
b. Improve usability of telehealth apps.
Integrate AI, wearables, and IoT for remote monitoring Build integrated & sustainable telehealth ecosystems
a. Develop seamless platforms combining video
consultations, e-prescriptions, online pharmacies, and lab
integration-responding to user needs for one-stop convenience.
b. Embed telemedicine into healthcare systems through
digital inclusion in national programs like Smart Bangladesh
and collaboration with Health Informatics Bangladesh (HIBD).
Support healthcare workforce capacity building
a. Train rural health workers in teleconsultation tools,
triage systems, and digital patient management to extend reach
effectively.
b. Enable task-shifting frameworks, where non-specialist
staff can handle initial screening and support tele-doctors.
Integrate telehealth into mainstream healthcare
Governments and healthcare providers must collaborate to introducing and maintaining telehealth inside existing health care system.
Foster community engagement & awareness
a. Run awareness campaigns to counter mistrust,
emphasizing success stories.
b. Ensure credible content and localization, offering
multilingual support and endorsements from respected
clinicians or institutions.
Conclusion
For telemedicine in Bangladesh to fully realize its potential, the country must address these challenges proactively. This includes continued investment in and expansion of digital infrastructure and internet access, especially in rural communities. Crucially, the government and service providers must work to increase public education and digital health literacy to foster greater trust and adoption. Regulatory frameworks must be strengthened to ensure patient data security, enable seamless integration of digital health records, and create an enabling environment for continued innovation.
References
- (2025) Population, total-Bangladesh. World Bank Group.
- (2023) Report: 68% Bangladeshis live in villages. Dhaka Tribune.
- (2020) Bangladesh medical & dental council. Telemedicine Guidelines.
- (2025) Directorate General of Health Services (DGHS). Health service through mobile phone.
- (2023) Bangladesh’s mobile users reach 190.36 million. The Business Standard.
- (2025) Digital 2025: Bangladesh. DataReportal-Global Digital Insights.
- Federal Reserve Bank of St. Louis (2024) Internet users for Bangladesh (per 100 people).
- (2025) Directorate General of Health Services (DGHS). Telemedicine Service.
- (2016) Free health service TONIC launched for Grameenphone customers.
- (2019) Jeeon healthcare signs deal with Paperfly. Bangladesh Post.
- Rahman H, Rubel M, Sadia B, Sarker N, Kabir S, et al. (2022) Use of telemedicine in Bangladesh: Current status and future prospects. North American Academic Research 5(4): 1-13.
© 2025 Nusrat Kamal*. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






