- Submissions

Full Text
Trends in Telemedicine & E-health
Evaluating the Awareness, Accessibility and Impact of Telepharmacy in Enhancing Healthcare Delivery in Pakistan
Muhammad Zulqurnain1, Ovais Ullah Shirazi2, Muhammad Arham Amin1, Huzaifa Ishtiaq1, Muhammad Yasir Iqbal1, Muhammad Nadeem Alvi1, Hassan Ahmad1, Waqas Akram1, Muzamal Hussain1, Gul Sher Ahmad1, Muhammad Moiz Ahmad1, Umda Tun Nisa2, Muhammad Saad Rao1, Itzaz Aslam3, Saad Hassan1 and Ali Akhtar1*
1Faculty of Pharmaceutical Sciences, University of Central Punjab, Pakistan
2Riphah Institute of Pharmaceutical Sciences, Riphah International University, Pakistan
3Allaint College of Professional Studies, Pakistan
*Corresponding author:Ali Akhtar, Faculty of Pharmaceutical Sciences, University of Central Punjab, Lahore, Pakistan
Submission: May 07, 2025;Published: May 28, 2025

ISSN: 2689-2707 Volume 5 Issue 4
Abstract
Background: Telepharmacy, the delivery of pharmaceutical services via telecommunications, has
emerged as a critical tool to improve healthcare access, particularly in underserved regions. While widely
adopted globally, its implementation in Pakistan remains limited and underexplored.
Aim: This study aimed to assess the knowledge, accessibility, perceptions, challenges and satisfaction
related to telepharmacy services among healthcare professionals and patients in Pakistan.
Methods: A cross-sectional survey using a structured questionnaire was conducted in Lahore, Pakistan,
with 407 participants, including healthcare professionals and patients. Descriptive statistics and
inferential tests were applied using SPSS.
Results: In this study, participants described high knowledge and the positive perception regarding
telepharmacy. Most of the healthcare professionals and patients considered that telepharmacy is playing
important role in increasing patient satisfaction, accessibility of medications and compliance of patients.
Technical barriers and insufficient digital competence are the key challenges and the difference in
knowledge and perception related to demographics is not significant.
Conclusion: Telepharmacy shows strong potential to enhance healthcare delivery in Pakistan. To ensure
its sustainable integration, targeted efforts are needed to improve digital literacy, address technical
challenges and establish clear regulatory frameworks.
Keywords:Telepharmacy; Digital health; Healthcare access; Medication adherence; Patient satisfaction
Introduction
The global healthcare landscape has undergone a remarkable transformation with the rapid advancement of digital health innovations, which offer novel opportunities to improve patient care, expand service availability and reduce healthcare disparities [1- 3]. Among these innovations, telepharmacy is the provision of pharmaceutical services through telecommunications has emerged as a promising solution to overcome barriers related to distance, cost and limited human resources [4]. By enabling pharmacists to deliver counseling, medication management and therapeutic monitoring remotely, telepharmacy addresses critical healthcare gaps, particularly in resource-limited, rural or underserved settings [4-6]. Many low and middle-income countries, including Pakistan, face persistent healthcare challenges such as rapid population growth, inadequate healthcare infrastructure, geographical barriers and a shortage of trained healthcare professionals [7-9]. These issues often result in limited access to pharmaceutical services, especially for individuals living in rural or remote areas [10]. Telepharmacy offers a creative, costeffective and scalable approach to bridging these healthcare gaps by providing timely, affordable and high-quality pharmaceutical services [11]. By reducing the need for in-person visits, minimizing travel burdens and expanding the reach of qualified pharmacists, telepharmacy has the potential to significantly enhance healthcare delivery and patient outcomes in Pakistan [12].
Despite its many benefits, the successful adoption of telepharmacy depends heavily on the knowledge, perceptions and readiness of both healthcare providers and patients [13]. International research from Malaysia, Indonesia, the United Arab Emirates (UAE) and Jordan has underscored the importance of technological literacy, digital infrastructure, patient trust and supportive regulatory frameworks in facilitating the effective implementation of telepharmacy [14]. Studies from these countries have reported positive perceptions among healthcare professionals, improvements in medication adherence and enhanced access to care, particularly during the COVID-19 pandemic [15,16]. However, they have also highlighted several challenges, including technical barriers, digital literacy gaps, data security concerns and increased workloads for pharmacists [4,11,17-19]. In the context of Pakistan, where healthcare disparities are pronounced and access to qualified pharmacists is often limited outside urban centers, telepharmacy holds enormous potential to improve healthcare delivery [8]. Yet, despite global advancements, there is a paucity of research exploring telepharmacy awareness, perceptions, accessibility and challenges within Pakistan’s unique sociocultural and healthcare landscape. Without context-specific data, policymakers and healthcare administrators may face difficulties designing effective telepharmacy programs and addressing barriers to implementation.
Although studies exist from Indonesia, Malaysia and UAE, no national data from Pakistan has been reported to date. This research gap underscores the urgent need to understand local awareness, perceptions, challenges and satisfaction levels associated with telepharmacy services among both healthcare professionals and patients in Pakistan. This study aimed to assess awareness, accessibility, perceptions, challenges and satisfaction regarding telepharmacy among healthcare professionals and patients in Pakistan. By identifying both barriers and opportunities, the study findings are expected to inform policymakers, healthcare providers and technology developers in developing targeted interventions, regulatory frameworks and educational initiatives to support the sustainable and equitable integration of telepharmacy into Pakistan’s healthcare system.
Methodology
Study design
A cross-sectional study was used to determine the knowledge, perception, accessibility and challenges related to telepharmacy among the patients and healthcare professionals in Pakistan.
Study setting
This study was conducted in Lahore, Pakistan. Lahore was selected because of the diverse city that combines urban and semi urban healthcare facilities and its population is also a representative of different socioeconomic and healthcare backgrounds.
Development of the questionnaire
After the thorough analysis of literature, the questionnaire is designed to cover all the objectives [14,20]. It was created to thoroughly evaluate people’s perspectives, knowledge, accessibility, difficulties, contentment and willingness about telepharmacy services. The questionnaire was divided into five sections: demographic profile, knowledge about telepharmacy, accessibility and usage of telepharmacy services, perceptions and attitudes toward telepharmacy and satisfaction with future willingness to use telepharmacy. To ensure uniformity and facilitate data analysis, the questionnaire was prepared in English, considering it as the primary language of instruction for the participants. A structured format was used to promote clarity, consistency and ease of response for all participants.
Study population and sample
In order to identify the research participants, non-probability convenience sampling was used. To ascertain the necessary sample size, a power analysis was performed with a 50% response distribution, a 95% confidence level and a 5% margin of error. People who participated in telepharmacy as patients or as medical professionals, including pharmacists or teleconsultants, were included in the target population. After thorough data screening and the elimination of inconsistent or missing entries, 407 valid responses from the 450 physical questionnaires that were delivered were kept for study.
Pilot study
Before starting the research, a pilot study with 16 individuals was carried out to assess the validity, reliability and clarity of the data collecting instrument. Regarding the questionnaire’s general appropriateness for the target group as well as its form and language, the pilot phase yielded insightful input. Changes were made to improve the instrument’s efficacy and guarantee higher accuracy and reliability for the bigger study sample in light of the pilot participants’ feedback and findings.
Data collection
Data collection for this study was carried out using a structured questionnaire developed based on an extensive literature review. The questionnaire was administered in person by trained enumerators across various healthcare settings in Lahore, Pakistan. Participants were approached directly and physical copies of the survey were distributed to ensure accessibility for all demographic groups. Each completed questionnaire was carefully reviewed for completeness and consistency before inclusion in the final dataset, maintaining the integrity and reliability of the collected data. The survey gathered detailed information on participants’ demographic profiles (such as age, gender, occupation and years of experience), their knowledge and perception of telepharmacy, accessibility and usage patterns, challenges faced, satisfaction levels and willingness to continue using telepharmacy services in the future.
Data analysis
The collected data were systematically organized and analyzed using IBM SPSS statistics version 27.0. Descriptive statistics, including frequencies, percentages, means and standard deviations, were used to summarize demographic variables, knowledge levels, perceptions, accessibility, satisfaction and challenges related to telepharmacy services. For the knowledge assessment, each correct response was scored as 1 and incorrect responses were scored as 0. The average knowledge scores were then calculated and categorized as follows: scores below 50% indicated poor knowledge, scores between 50% and 75% indicated moderate knowledge and scores above 75% indicated good knowledge. Perceptions regarding telepharmacy services were initially assessed through a likert scale with options ranging from “strongly agree” to “strongly disagree.” For analysis purposes, “strongly agree” and “agree” were grouped as positive responses (scored as 1), while “disagree” and “strongly disagree” were grouped as negative responses (scored as 0). Neutral responses were excluded from binary categorization to maintain clarity and consistency. Inferential analyses were conducted to explore relationships between demographic characteristics and knowledge or perception scores. For continuous variables, independent sample t-test and ANOVA were used and for categorical variables, chi-square test was applied. P-value<0.05 was considered statistically significant and p-value less than 0.2 was further analysed using logistic regression with 95% confidence intervals.
Ethical considerations
This study was done in compliance with the ethical principles and authorized by the university ethical committee. After granting approval, review board also ensures that study meets the standard guidelines. Informed consent was obtained from all the participants and the study was carried out with confidentiality.
Result
Study participants
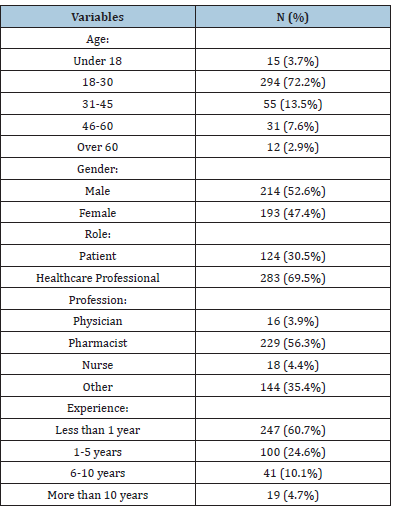
After the exclusion of incomplete or invalid responses, we achieved a high response rate of 90.4% with 407 valid responses out of 450 distributed questionnaires. The majority of responders were young people, with 72.2% of them being between the ages of 18 and 30 followed by 13.5% who were between the ages of 31 and 45, 7.6% who were between the ages of 46 and 60 and 2.9% who were above 60. A minor segment (3.7%) was under 18, indicating some adolescent engagement with telepharmacy services. In terms of gender, the sample was relatively balanced, with 214 males (52.6%) and 193 females (47.4%). Regarding participant roles, 69.5% (n=283) identified as healthcare professionals, while 30.5% (n=124) were patients, enabling the study to capture perspectives from both sides of the healthcare interaction. Among the healthcare professionals, pharmacists comprised the largest group (56.3%), followed by other roles (e.g., administrative staff and public health officers) at 35.4%, nurses at 4.4% and physicians at 3.9%. This distribution highlights the prominence of pharmacists as the primary stakeholders in telepharmacy practices. Many participants had less than one year of experience in their current role (60.7%), suggesting a largely early-career respondent base. Meanwhile, 24.6% had 1-5 years of experience, 10.1% had 6-10 years and only 4.7% reported more than a decade of experience. This skew toward less experienced professionals may reflect greater receptivity to digital tools like telepharmacy, a trend noted in previous studies.
Young pharmacists’ knowledge regarding telepharmacy
Table 1:Demographic characteristics of healthcare professionals and patients participating in the telepharmacy study in Lahore, Pakistan (N = 407).
The assessment of participants regarding telepharmacy in Pakistan revealed generally high levels of awareness and understanding across key components of the practice (Table 1). A significant majority of respondents (82.3%; n=335) acknowledged that telepharmacy services are available in Pakistan, establishing a baseline awareness of its presence in the national healthcare system. Furthermore, 84.8% (n=345) recognized the knowledge of Information and Communication Technology (ICT) for pharmacists is important to effectively deliver telepharmacy services. Additionally, 87.5% (n=356) of participants acknowledged the pivotal role played by telepharmacy during the COVID-19 pandemic, underlining its critical function in supporting remote pharmaceutical care during health crises. Awareness of technological requirements was also strong, with 77.1% (n=314) of respondents affirming that a stable internet connection and high-performance technology is necessary for its implementation. When asked about specific applications and benefits of telepharmacy, 70.5% (n=287) agreed that telepharmacy improve the quality of patient counseling by offering greater privacy and extended consultation time, while 72.2% (n=294) believed that it helps alleviate waiting time issues in general hospitals.
Awareness of telepharmacy’s involvement in clinical monitoring was moderate, with 65.8% (n=268) acknowledging that telepharmacy utilized for monitoring and reporting adverse drug reactions in clinical practice, whereas 34.2% (n=139) did not recognize this function. Moreover, 66.6% (n=271) indicated that telepharmacy is carried out through drug information services during office hours and by emergency departments after hours. Regarding rural accessibility, 69.8% (n=284) of respondents agreed that it enhances access to medications and information for patients in remote areas. Finally, 70.5% (n=287) believed that its services have the potential to extend pharmaceutical care beyond standard working hours, particularly benefiting healthcare institutions that lack 24-hour pharmacy services. Based on the binary scoring of knowledge questions, participants demonstrated an overall high level of telepharmacy knowledge. The responses indicated a strong collective understanding of fundamental aspects of telepharmacy, including its availability in Pakistan, its technological requirements and its importance during the COVID-19 pandemic (Figure 1). The average knowledge scores suggest that most participants possessed good knowledge (scoring above 75%), aligning with previous findings from similar studies conducted in other developing countries (Table 2).
Figure 1:Correct versus incorrect responses across telepharmacy knowledge domains among study participants.
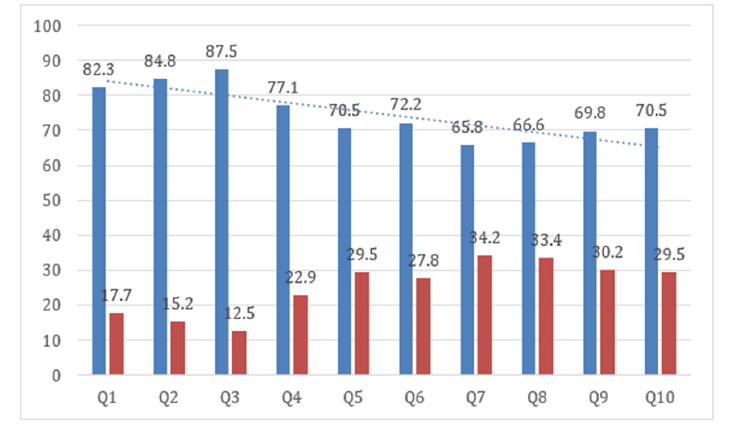
Table 2:Participant responses on knowledge of telepharmacy services, technological requirements, and clinical applications.
The high proportion of correct responses across most items reflects a well-informed group, especially among pharmacists and early-career healthcare professionals. However, moderate knowledge levels (with lower agreement percentages) were observed in areas related to telepharmacy’s role in adverse drug reaction reporting and its use by emergency departments beyond standard operating hours. These areas may benefit from targeted educational interventions to further enhance understanding and practical readiness among healthcare providers.
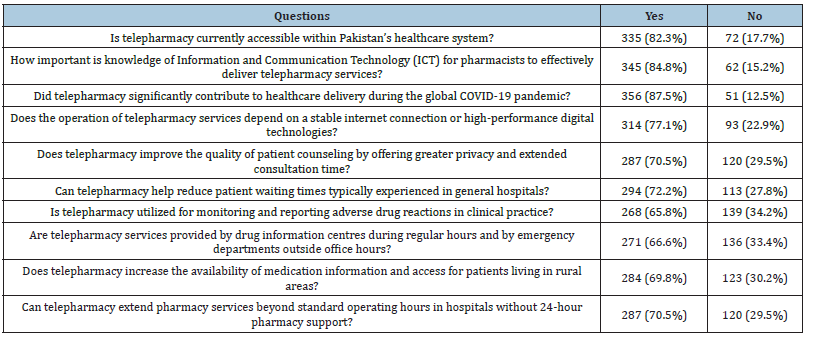
Young pharmacists’ perception regarding telepharmacy
Assessment of perception of telepharmacy services among healthcare professionals in Pakistan was done based on a series of likert-scale statements (Table 3). The analysis showed a varied range of perceptions, with generally positive attitudes toward telepharmacy’s role in enhancing healthcare delivery. Many respondents agreed that telepharmacy improves patient compliance to medication (70.5%; n=287) and enhances accessibility to medications in rural areas (60.5%; n=246). In addition, 65.4% (n=266) believed that it allows patients to save money and travel time by avoiding visits to physical healthcare facilities. Concerns were also expressed regarding potential drawbacks. About 49.4% (n=201) of participants agreed that telepharmacy may be associated with a higher error rate in dispensing medications compared to regular practice. Furthermore, 54.1% (n=220) reported concerns about increased workload and professional commitment required to implement and sustain telepharmacy services. 56.6% (n=230) of respondents were willing to share their personal information through online platforms when using telepharmacy services indicating agreement or strong agreement. In terms of educational preparedness, a significant number of participants (66.1%; n=269) agreed that pharmacy schools should integrate IT and telepharmacy training into their academic curriculum.
Table 3:Participant perceptions on the benefits, risks and implementation challenges of telepharmacy services, based on Likert-scale ratings.
Additionally, 60.4% (n=246) believed that telepharmacy could help minimize pharmacist shortages, especially in underserved or rural settings. According to these results, telepharmacy is usually seen favourably by Pakistani pharmacists, especially when it comes to its ability to improve patient burden and healthcare access. Nonetheless, sceptical opinions continue to exist, particularly with regard to implementation issues including hazards to data privacy, the possibility of prescription mistakes and increasing task expectations. A mostly positive attitude among Pakistani healthcare workers was revealed by the computed average perception ratings across the likert-scale questions. Most respondents strongly agreed with statements highlighting the advantages of telepharmacy, including increased patient adherence, accessibility in rural areas and financial convenience. On the other hand, worries about the possible drawbacks of telepharmacy also generated significant reactions. Increased workload, privacy concerns and the possibility of higher error rates were acknowledged by a significant subset of participants. These findings highlight a balanced viewpoint: while the participants are supportive of telepharmacy’s broader integration, they remain mindful of operational and infrastructural challenges. The overall perception score, derived from the categorized responses, demonstrates that pharmacists and healthcare professionals in Pakistan are generally supportive of telepharmacy initiatives, recognizing both the substantial opportunities and the necessary areas for policy and practice refinement.
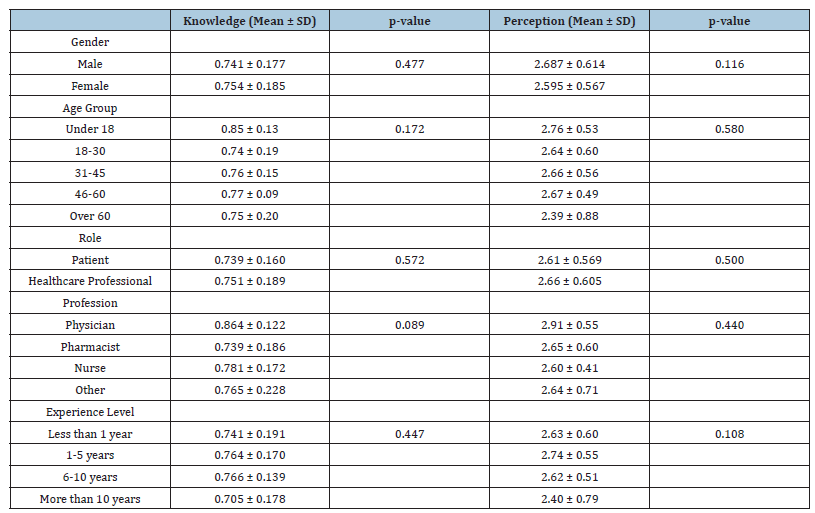
Relationship between demographics and knowledge
No statistically significant association was found between knowledge scores and gender (p=0.477), age group (p=0.172) or years of experience (p=0.447). Although minor variations were observed-such as slightly higher knowledge scores among physicians and participants under 18-these differences were not significant. Overall, the data suggest that knowledge of telepharmacy was consistently high across different demographic groups.
Relationship between demographics and perception
No significant associations were found between demographic characteristics and perception scores. Variables such as gender (p=0.118), age (p=0.580), role (p = 0.500) and years of experience (p=0.108) did not show any meaningful differences in perception toward telepharmacy. Although slight variations in mean scores were noted-such as higher perception among participants with 1-5 years of experience and physicians-these were not statistically significant, indicating a generally positive perception of telepharmacy across all groups (Table 4).
Table 4:Comparison of telepharmacy knowledge and perception scores across demographic groups, with mean ± standard deviation and p-values.
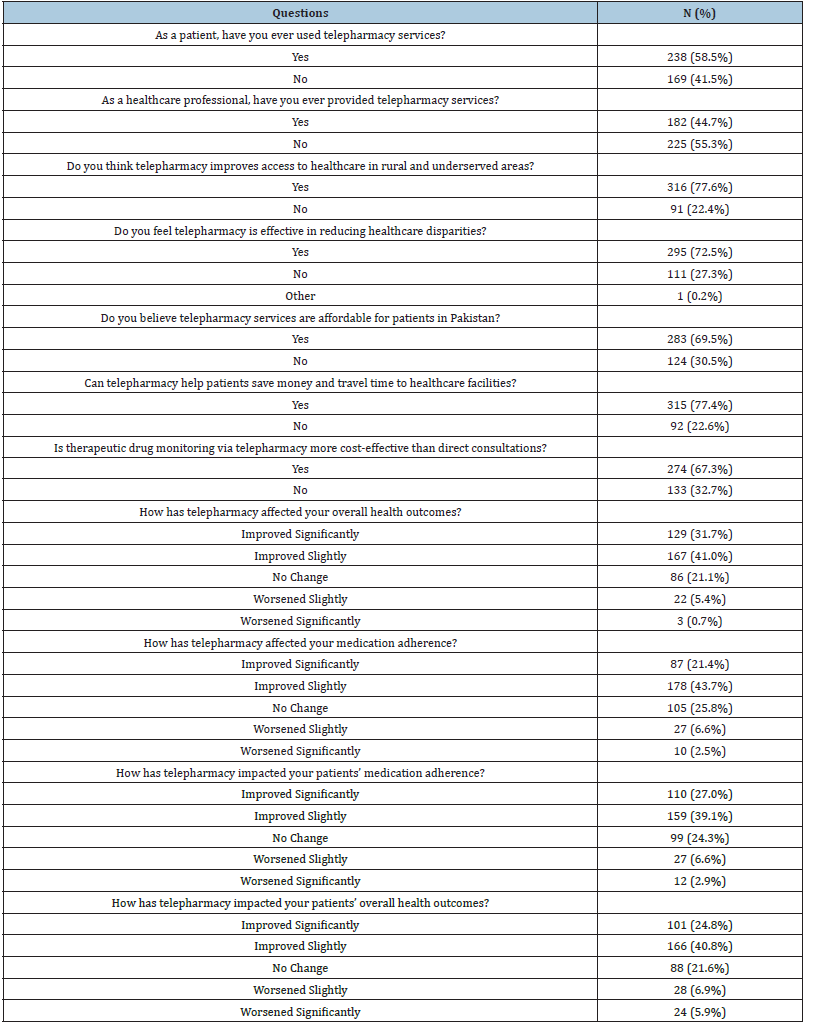
Impact on Medication Adherence and Patient Outcomes
The data presented highlights the strong positive impact of telepharmacy on both medication adherence and overall health outcomes. A notable 31.7% of respondents reported that telepharmacy significantly improved their overall health, while an additional 41.0% observed slight improvements. Only a minority experienced no change (21.1%) or negative effects (6.1% combined). In terms of medication adherence, 21.4% of patients indicated significant improvement and 43.7% reported slight enhancements, with just 2.5% noting a decline. From the perspective of healthcare professionals, 27.0% observed significant improvement in their patients’ adherence, while 39.1% saw slight improvements. Reports of deterioration were minimal. When assessing patient health outcomes, 24.8% of professionals noticed significant positive changes and 40.8% observed slight improvements, with only 5.9% reporting any worsening. These findings collectively emphasize the promising role of telepharmacy in enhancing healthcare delivery, despite a small portion of participants reporting limited or adverse effects (Table 5).
Table 5:Participant responses on telepharmacy experiences, effectiveness and affordability.
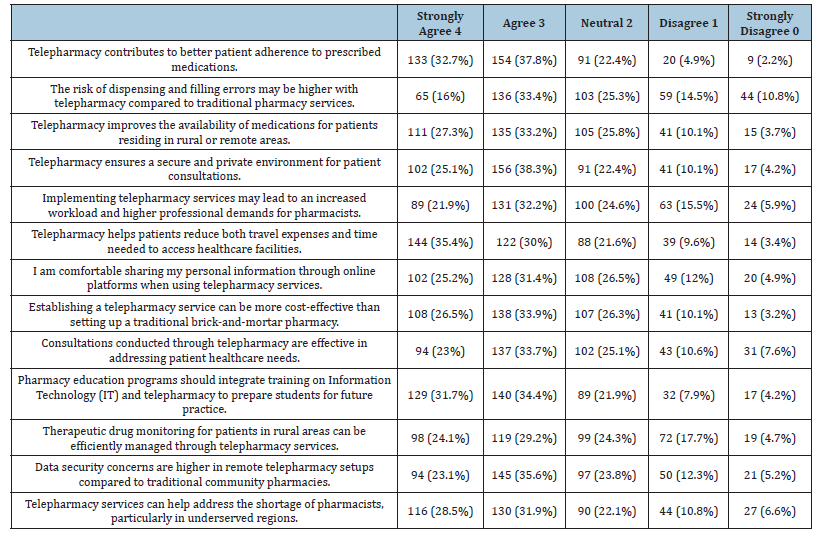
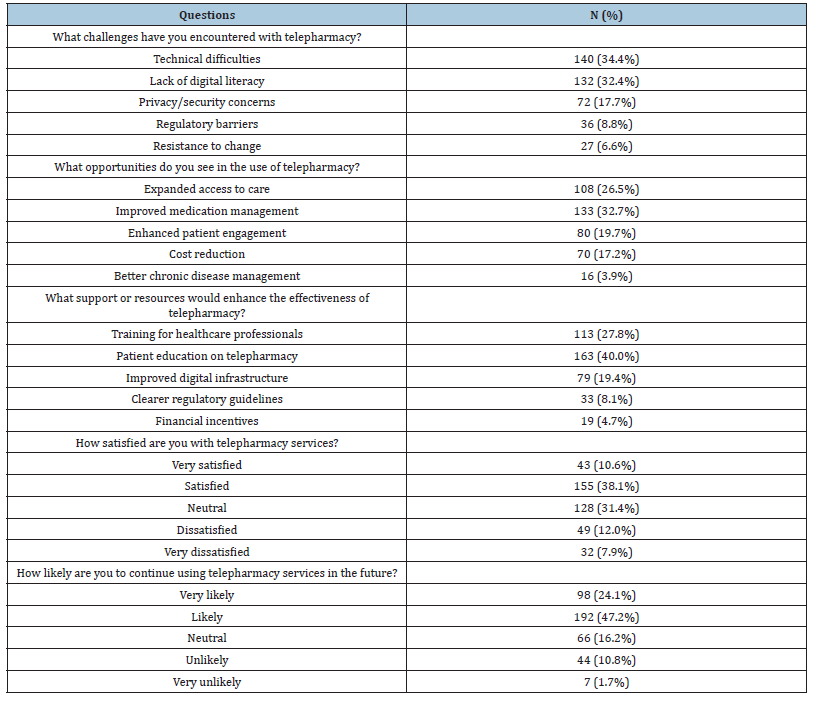
Challenges and Opportunities in Implementing Digital Health Solutions
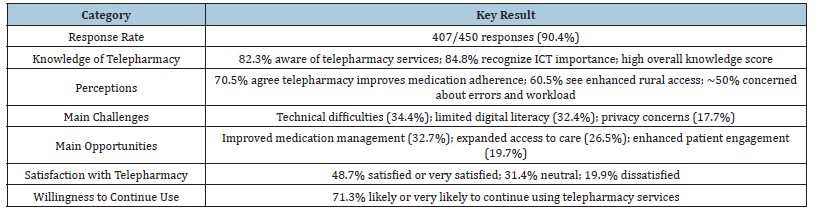
The implementation of telepharmacy faces several key challenges, with technical difficulties (34.4%) and limited digital literacy (32.4%) emerging as the most significant barriers. Other notable concerns include issues related to privacy and security (17.7%), regulatory barriers (8.8%) and resistance to change among users (6.6%). Despite these challenges, the study highlights numerous opportunities associated with telepharmacy. The most frequently identified opportunity was improved medication management (32.7%), followed by expanded access to care (26.5%) and enhanced patient engagement (19.7%). Additional perceived benefits included cost reduction (17.2%) and improved chronic disease management (3.9%). Participants recommended that along with the training of healthcare professionals (27.8%), there is also a need for patient education (40%) to increase the benefits of telepharmacy. For the successful implementation of telepharmacy, there is need to establish the proper regulatory guidelines (8.1%), promoting digital infrastructure (19.4%) and also provide financial incentives (4.7%). Overall satisfaction with telepharmacy services was relatively high, with 38.1% of respondents reporting satisfaction and 10.6% expressing high satisfaction. Meanwhile, 31.4% remained neutral and 19.9% reported dissatisfaction or strong dissatisfaction. Regarding future use, 47.2% of participants indicated they were likely to continue utilizing telepharmacy services, while 24.1% stated they were very likely (Figure 2). Only a small proportion expressed uncertainty or reluctance, with 10.8% being unlikely and 1.7% very unlikely to continue (Table 6).
Figure 2:Participant satisfaction levels with telepharmacy services.
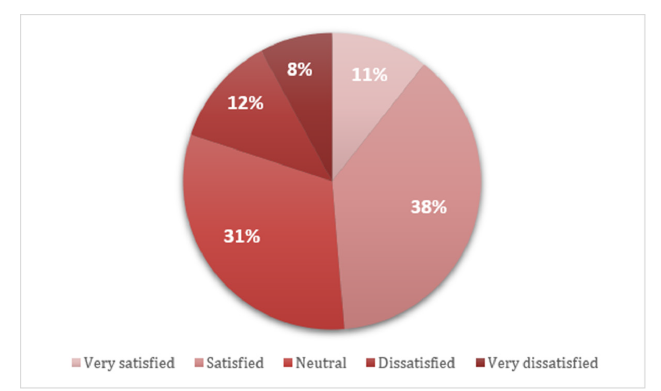
Table 6:Challenges encountered and opportunities identified in telepharmacy implementation.
Discussion
According to the demographics analysis, it is found that 72.2% participants were adults within the age of 18-30 which aligns with the studies done in Indonesia and Malaysia where young healthcare professionals are ready to convert on digital platforms [21,22]. 47.4% of participants were female, which is lower than in previous studies where female participation was dominant, suggesting that females are generally more likely to participate voluntarily aligning with previous studies that provide a balanced perspective [21,23].
In this research, most of the participants were healthcare professionals (69.5%), in which pharmacists were making up over half of this group (56.3%). This outcome is in line with findings from research carried out in Indonesia and Iran, where the main group using telepharmacy services was pharmacists [24,25]. Most respondents (60.7%) had less than one year of professional experience that is also consistent with the study in Malaysia [21] which suggests new healthcare professionals who are more open to technology are more attractive towards the telepharmacy. Furthermore, both patients (30.5%) and healthcare professionals (69.5%) participated in the study providing a balanced perspective, consistent with the study from Jordan [26].
Most participants (82.3%) were aware that telepharmacy services are available in Pakistan similar to the findings in Malaysia and Indonesia [22,23], where a majority of the public was aware of telepharmacy services. A high percentage (84.8%) of participants agreed that knowledge of Information and Communication Technology (ICT) is important for pharmacists using telepharmacy matches the results in Malaysia [21]. However, only 37.5% of participants correctly recognized that telepharmacy played a major role during the COVID-19 pandemic globally. This awareness level is lower compared to findings in Indonesia [24], where COVID-19 significantly boosted telepharmacy use across the country. Similarly, Ibrahim et al. found that telepharmacy was vital in maintaining healthcare delivery during the pandemic [17]. The majority of respondents (77.1%) understood that telepharmacy requires a high-performance technology that is consistent with barriers reported in Iran [27]. Other knowledge areas, such as understanding that telepharmacy can solve waiting time problems (72.2%), extend hospital pharmacy services (70.5%) and improve medication access for rural patients (69.8%), were reasonably strong. These results align with the international experience reported in UAE, where telepharmacy expanded healthcare access and reduced waiting times [28]. On the other hand, the lower awareness that telepharmacy is involved in Adverse Drug Reaction (ADR) monitoring (65.8%) suggests that some participants may not fully understand the wide clinical roles of telepharmacy.
The findings show that participants generally have a positive perception of telepharmacy. A large number (70.5%) agreed that telepharmacy improves patients’ adherence to medication similar to the study in Iran [27]. However, some participants (about 50%) were concerned that telepharmacy may have a higher error rate for dispensing and filling medications compared to traditional pharmacies. This fear is understandable and was also mentioned in the UAE study [28]. About 60% agreed that telepharmacy enhances patient access, especially in rural areas and these results are supported by studies in Malaysia and in Indonesia [22,23]. Around 64% of respondents agreed that telepharmacy offers a better privacy setting. This matches with study in Jordan, who found that patients valued privacy when using telepharmacy services [26]. However, around 54% of participants believed that telepharmacy increases pharmacists’ workload and commitment. Similar concerns were raised by Ameri et al. (2020), who discussed that telepharmacy, while convenient for patients, can lead to increased work stress for pharmacists if proper support systems are not in place [25]. Participants also believed strongly (65.4%) that telepharmacy saves time and money consistent with findings in Malaysia [21]. Regarding data security, about half of the participants were willing to share their personal information online. While this shows a good level of trust, it is important to note that concerns about cybersecurity were raised in UAE [28]. A large proportion (over 70%) agreed that pharmacy schools should introduce education programs focused on telepharmacy [27].
Participants also viewed telepharmacy positively for its role in monitoring adverse drug reactions (about 61%) and addressing the shortage of pharmacists (about 60%) also discussed in the study during COVID [17]. This study found no significant differences in telepharmacy knowledge and perception scores across gender, age, role, profession or experience levels. Both males and females showed similar knowledge (p=0.477) and perception (p=0.116) scores, consistent with studies in Malaysia [21,23]. Younger participants (under 18) had slightly higher scores, but age was not a significant factor (p=0.050), matching findings from Indonesia [22]. Healthcare professionals scored slightly better than patients, yet the difference was not significant (p=0.5), similar to study in Indonesia [24]. Among professions, physicians had the highest knowledge scores, but the variation was not statistically meaningful (p=0.089), agreeing with Ameri et al. [25]. Experience level also showed no significant influence, though early-career professionals had slightly higher perception scores, as noted by the study in UAE [28]. Briefly, demographic factors did not strongly affect telepharmacy knowledge or perception, indicating a generally uniform readiness across all groups.
About 31.7% of respondents reported a significant improvement in their overall health and 41.0% noticed slight improvements. Only a small percentage (6.1%) experienced negative effects. Similarly, regarding medication adherence, 21.4% reported major improvements and 43.7% reported slight improvements, showing telepharmacy’s potential to help patients manage their medications better. Healthcare professionals also observed improvements: 27.0% noticed a significant improvement in patient adherence and 39.1% noticed slight improvement. These results match earlier findings in Malaysia and Indonesia, where telepharmacy was reported to improve patient medication use and overall healthcare access [22,23]. Despite the benefits, several challenges were identified. Technical difficulties (34.4%) and lack of digital literacy (32.4%) were the most common problems faced by participants. Privacy concerns (17.7%) and regulatory issues (8.8%) were also noted. These challenges are consistent with findings from UAE, who reported technical and privacy barriers as common obstacles in telepharmacy adoption [25,28]. In contrast, developed nations often report fewer issues related to basic access but focus more on regulatory alignment and advanced data privacy measures [29]. Hence, it is crucial to contextualize telepharmacy implementation strategies according to the technological readiness and digital inclusion of the target population.
However, improved medication management (32.7%), expanded access to care (26.5%) and enhanced patient engagement (19.7%) were major positive outcomes. These findings match with study in UAE, which emphasized telepharmacy’s role in improving medication safety and healthcare efficiency [26]. To strengthen telepharmacy services, participants highlighted the need for patient education (40.0%) and healthcare professional training (27.8%), supported by better digital infrastructure (19.4%). Similar recommendations were made by Emadi et al., who pointed out the importance of technology training and support for telepharmacy success [27]. About 92% of participants reported they would use telepharmacy in the future, reflecting the growing acceptance and anticipated advancements in telepharmacy services and about 78% of participants were satisfied with their telepharmacy experience regardless of technical difficulties that matches with the study findings in Indonesia [24]. While this study provides valuable insights into the awareness, perceptions, and challenges of telepharmacy in Pakistan, it is important to acknowledge its limitations, including its focus on urban populations and reliance on quantitative data. Future studies should include rural settings, qualitative interviews and intervention trials to capture more diverse perspectives and evaluate the long-term effectiveness of telepharmacy interventions (Table 7).
Table 7:Summary of key findings on telepharmacy awareness, perceptions, challenges, satisfaction and future use among healthcare professionals and patients in Pakistan.
Strengths and Limitations of the Study
This study has several notable strengths. It achieved a high response rate, which enhances the reliability of the findings. The inclusion of a diverse participant pool, comprising both healthcare professionals and patients, strengthens the validity and representativeness of the results. The large sample size and comprehensive focus on telepharmacy awareness, perceptions, accessibility, challenges and satisfaction offer an in-depth understanding of the current status and future potential of telepharmacy in Pakistan. Furthermore, the inclusion of participants from various demographic backgrounds offers valuable insights into the broad patterns of acceptance and readiness across the healthcare system. However, several limitations should be acknowledged. The study was limited to Lahore, an urban setting, which may restrict the generalizability of the findings to rural and remote areas of Pakistan. The use of non-probability convenience sampling may have introduced selection bias, as individuals with greater interest or familiarity with telepharmacy were potentially more likely to participate. Additionally, the reliance on self-reported data raises the possibility of recall bias and social desirability bias, which may have influenced participants’ responses. These limitations highlight the need for cautious interpretation of the results and suggest that future research should include rural populations, employ probability sampling methods and incorporate qualitative interviews and intervention trials to further validate and extend the findings.
Conclusion
This study concluded that patients and healthcare professionals have high level of awareness and positive perception regarding telepharmacy which shows its greater potential in the near future. These findings emphasize that while telepharmacy can significantly enhance healthcare delivery, its sustainable integration demands targeted efforts. However, challenges such as technical difficulties, digital literacy gaps and privacy concerns must be addressed. These results highlight the need for improved infrastructure, targeted training and clear regulations to support telepharmacy’s successful implementation and long-term sustainability, ultimately enhancing healthcare access nationwide.
References
- Iyengar K, Gaurav KU, Raju V, Vijay J (2020) COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr 14(5): 733-737.
- Shiferaw F, M Zolfo (2012) The role of Information Communication Technology (ICT) towards universal health coverage: The first steps of a telemedicine project in Ethiopia. Global Health Action 5(1): 1-8.
- Shah MN, Erin BW, Suzanne MG, Nancy EW, Wang H, et al. (2015) High-intensity telemedicine decreases emergency department use for ambulatory care sensitive conditions by older adult senior living community residents. Journal of the American Medical Directors Association 16(12): 1077-1081.
- Poudel A, Nissen LM (2016) Telepharmacy: A pharmacist’s perspective on the clinical benefits and challenges. Integr Pharm Res Pract 5: 75-82.
- Alexander E, David BC, Andrea D, Matthew TJ, Robert DL, et al. (2017) ASHP statement on telepharmacy. American Journal of Health-System Pharmacy 74(9): e236-e241.
- Lester CA, Chui MA (2016) The prescription pickup lag, an automatic prescription refill program and community pharmacy operations. J Am Pharm Assoc 56(4): 427-432.
- (2010) Increasing access to health workers in remote and rural areas through improved retention: Global policy recommendations. World Health Organization.
- Zaidi S, Maryam B, Aleem N, Arash R (2013) Access to essential medicines in Pakistan: Policy and health systems research concerns. PloS One 8(5): e63515.
- Mills A (2014) Health care systems in low-and middle-income countries. N Engl J Med 370(6): 552-557.
- Baldoni S, Amenta F, Ricci G (2019) Telepharmacy services: Present status and future perspectives: A review. Medicina 55(7): 327.
- Pathak S, Carrie MB, Elizabeth M, Benjamin YU (2021) A systematic review of the effect of telepharmacy services in the community pharmacy setting on care quality and patient safety. Journal of Health Care for the Poor and Underserved 32(2): 737-750.
- Almukalfi RD, Sultan SA, Ayad SA, Rabeh AM, Aloufi ZM, et al. (2023) The impact of telepharmacy on rural and underserved communities. Acta Scientiae 6(2): 169-180.
- Ahmed NJ, Ziyad SA, Asmaa HA, Alturki A, Abdulaziz HB, et al. (2023) Knowledge, perceptions and readiness of telepharmacy among community pharmacists. Saudi Pharmaceutical Journal 31(9): 101713.
- Ghozali MT (2024) Assessment of knowledge, perception and readiness for telepharmacy-assisted pharmaceutical services among young pharmacists in rural Indonesia. Explor Res Clin Soc Pharm 16: 100513.
- Omboni S, Caserini M, Coronetti C (2016) Telemedicine and M-health in hypertension management: Technologies, applications and clinical evidence. High Blood Press Cardiovasc Prev 23(3): 187-196.
- Jamie YP, Peter JZ, Mary AV (2022) Perspectives and experiences with telepharmacy among pharmacists in Canada: A cross-sectional survey. Pharmacy practice 20(1): 2609.
- Mohamed IO, Ibrahim MR, Derar HA, Ahmad ZM, Nadia AM (2021) Evaluation of telepharmacy services in light of COVID-19. Telemed J E Health 27(6): 649-656.
- Unni EJ, Patel K, Isaac RB, Hung M (2021) Telepharmacy during COVID-19: A scoping review. Pharmacy 9(4): 183.
- Win AZ (2017) Telepharmacy: Time to pick up the line. Res Social Adm Pharm 13(4): 882-883.
- Muhammad K, Baraka MA, Shah SS, Hammad MB, Wali H, et al. (2022) Exploring the perception and readiness of pharmacists towards telepharmacy implementation; a cross-sectional analysis. PeerJ 10: e13296.
- Mahmud NR, Hamdan NE, Usir E (2025) Knowledge, perception and readiness to utilize telepharmacy among Malaysian public. Malaysian Journal of Medicine and Health Sciences 21(1): 134-140.
- Tjiptoatmadja NN, Alfian SD (2022) Knowledge, perception and willingness to use telepharmacy among the general population in Indonesia. Frontiers in Public Health10: 825554.
- Ahmad A, Shubashini G, Karuppannan M (2024) Embracing telepharmacy: Unveiling Malaysians’ perceptions and knowledge through online survey. PLoS One 19(8): e0307897.
- Kusuma IY, Hiba FM, Arizandi AK, Akbar MB, Khamdiyah IK, et al. (2024) Telepharmacy in Indonesia: Navigating knowledge, perception and readiness among 6,000 pharmacists and related sociodemographic determinants. Telemedicine and E-Health 30(9): 2483-2494.
- Ameri A, Farzad S, Sareh K, Kambiz B (2020) Investigating pharmacists’ views on telepharmacy: Prioritizing key relationships, barriers and benefits. J Pharm Technol 36(5): 171-178.
- Jarab AS, Walid AQ, Tareq M, Ahmad AA, Zelal K, et al. (2024) Factors influencing public attitudes and willingness to utilize telepharmacy services in the UAE. International Journal of Telemedicine and Applications 2024: 5755493.
- Emadi F, Arash G, Sulmaz G, Bastani P, Melissa TB (2022) Factors affecting medication adherence among older adults using tele-pharmacy services: A scoping review. Archives of Public Health 80(1): 199.
- Jirjees F, Mohanad O, Lynn A, Zelal K, Karem HA, et al. (2022) The rise of telepharmacy services during the COVID-19 pandemic: A comprehensive assessment of services in the United Arab Emirates. Pharmacy Practice 20(2): 2634.
- Scott KC, Karem P, Shifflett K, Vegi L, Ravi K, et al. (2018) Evaluating barriers to adopting telemedicine worldwide: A systematic review. Journal of Telemedicine and Telecare 24(1): 4-12.
© 2025 Ali Akhtar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






