- Submissions

Full Text
Trends in Telemedicine & E-health
Transforming Treatment: An Integrative Review of Telemedicine and Its Impact on Pediatric Eating Disorders
Katelin A Crane*
PhD Student & Conway Fellow, M Louise Fitzpatrick College of Nursing, Villanova University, USA
*Corresponding author:Katelin A Crane, M Louise Fitzpatrick College of Nursing, Villanova University, USA
Submission: July 02, 2024; Published: July 26, 2024

ISSN: 2689-2707 Volume 5 Issue 1
Abstract
Background: Eating Disorders (EDs) among children and adolescents, such as Anorexia Nervosa
(AN), Bulimia Nervosa (BN), and Binge Eating Disorder (BED) present significant clinical challenges
due to their complexity. Traditional treatment approaches often encounter barriers including limited
accessibility, high costs, and logistical constraints. Telemedicine has emerged as a promising alternative
to conventional in-person treatment, offering potential benefits in accessibility and convenience.
Objective: This integrative review aims to evaluate the efficacy, benefits, and challenges of telemedicine
interventions in the treatment of EDs among children and adolescents.
Methods: A comprehensive literature search was conducted according to Whittemore and Knafl’s
integrative review framework across multiple databases to identify studies assessing telemedicine
interventions for EDs in children and adolescents. A quality assessment was conducted on the included
studies and key outcomes were systematically analyzed.
Result: Eight studies met the inclusion criteria, showcasing a range of telemedicine interventions. Six
studies focused exclusively on video telemedicine, providing virtual therapy and monitoring. One study
utilized a combination of video telemedicine and telecommunications, while another implemented appbased
monitoring with therapeutic sessions. Virtual intensive treatment programs were highlighted in
one study, offering structured daily therapeutic activities. Home-based hospitalization, observed in one
study, provided intensive virtual care replicating inpatient treatment. The review found that telemedicine
interventions yielded positive clinical outcomes, including symptom reduction, weight stabilization, and
psychological improvements. Patient and family engagement were high, enhancing accessibility and
convenience. However, challenges such as technological barriers, privacy concerns, and maintaining
therapeutic rapport were identified.
Conclusion: Telemedicine presents a viable and effective alternative for treating EDs in children and
adolescents, offering significant advantages in accessibility and patient engagement. Despite certain
limitations, telemedicine interventions can effectively complement traditional treatment modalities.
Future research should focus on refining telemedicine approaches, exploring hybrid care models, and
investigating long-term outcomes to optimize the integration of telemedicine into eating disorder
treatment.
Keywords:Telemedicine; Eating disorders; Children; Adolescents; Video telemedicine; Virtual therapy; Telehealth; Family therapy
Background
Eating disorders among children and adolescents represent a significant public health concern, characterized by severe disruptions in eating behaviors leading to physical and mental health deterioration [1]. Among the most prevalent disorders are anorexia nervosa, bulimia nervosa, and binge eating disorder, among others. Anorexia Nervosa (AN) is a psychiatric disorder with one of the highest mortality rates, marked by severely restricted eating, an intense fear of gaining weight, and a distorted body image, often leading to severe weight loss and malnutrition [2]. Bulimia Nervosa (BN) involves cycles of binge eating and compensatory behavior (e.g., self-induced vomiting or “purging”, overexercising, restrictive eating) alongside the overappraisal body shape and weight to prevent weight gain [3]. Binge Eating Disorder (BED) is characterized by recurrent episodes of eating large quantities of food, often rapidly and to the point of discomfort, accompanied by feelings of loss of control and distress, but without regular compensatory behaviors as in BN [4].
Pediatric eating disorders present a critical public health issue, with substantial prevalence and disease burden. Epidemiological studies of U.S. adolescents aged 13 to 18 years indicate the lifetime prevalence of eating disorders was nearly 3%, with prevalence rates of AN, BN, and BED were 0.3%, 0.9%, and 1.6%, respectively [5]. These disorders frequently emerge during adolescence, a pivotal period marked by significant physical, psychological and social development [1]. The disease burden associated with eating disorders in this age group is profound, affecting physical health, psychological well-being, and social functioning. Adolescents with eating disorders often experience severe medical complications, including malnutrition, electrolyte imbalances, and cardiovascular issues, which can have long-term health consequences [6]. Psychologically, these disorders are linked to high levels of comorbidity with psychiatric disorders such as depression, anxiety, and obsessive-compulsive disorder, further complicating treatment and prognosis [7]. Socially, eating disorders can disrupt academic performance, peer relationships, and family dynamics, leading to isolation and reduced quality of life [1,8]. Despite the significant impact on affected individuals and their families, there are often delays in diagnosis and treatment, exacerbating the disease burden and highlighting the need for more accessible and effective intervention strategies [1].
Traditional treatment approaches for these disorders typically include a combination of psychological therapy, nutritional counseling, and medical monitoring [9-11]. However, these methods present notable challenges, especially for younger populations. Access to specialized care can be limited by geographic location, socioeconomic factors, and the availability of trained professionals [1]. Additionally, the stigma associated with mental health and eating disorders can deter youth and their families from seeking help. Adolescents in particular may face unique barriers such as school commitments, reliance on parental support, and a need for age-appropriate engagement strategies [12]. The intensive nature of conventional treatments often requires frequent in-person visits, which can be logistically and financially burdensome, thereby hindering consistent and comprehensive care.
Significance of Telemedicine
Telemedicine refers to the use of digital communication technologies to deliver healthcare services remotely. It encompasses a variety of modalities, including video conferencing, telephone consultations, and online therapy platforms [13]. Telemedicine allows healthcare providers to diagnose, treat, and monitor patients through digital means, facilitating continuous care outside traditional clinical settings. The components of telemedicine extend beyond mere consultations to include remote monitoring, online resources, and digital tools for patient education and engagement.
For pediatric and adolescent populations, telemedicine offers several advantages. It can enhance access to specialized care for those in remote or underserved areas, reducing the need for travel and associated costs [14]. Telemedicine also provides a level of flexibility that can accommodate the schedules of young patients and their families, thereby improving adherence to treatment protocols. Moreover, the use of familiar digital platforms can increase engagement among tech-savvy adolescents, making the treatment process more relatable and less intimidating [15]. By integrating telemedicine into the care continuum, healthcare providers can offer a more personalized and responsive approach to managing eating disorders, which is particularly beneficial in maintaining therapeutic relationships and ensuring continuity of care during critical stages of recovery.
Objectives of the Review
The primary objective of this integrative review is to evaluate the efficacy, benefits, and challenges associated with the use of telemedicine in the treatment of eating disorders among children and adolescents. Specifically, this review aims to analyze the current evidence on how telemedicine compares to traditional in-person treatments in terms of clinical outcomes, patient engagement, and accessibility. It will explore various telemedicine modalities to determine their effectiveness in delivering psychological therapy, nutritional counseling, and ongoing support for this population. Additionally, the review seeks to identify potential barriers and limitations of telemedicine, including technological issues, privacy concerns, and the feasibility of remote assessments. By synthesizing findings from existing studies, this review intends to provide comprehensive insights into the role of telemedicine in improving treatment access and outcomes for pediatric and adolescent patients with eating disorders, offering recommendations for best practices and future research directions.
Methods
Whittemore and Knafl’s integrative review methodology was used to guide the review of the literature on the use of telemedicine for pediatric eating disorders. This methodology consists of five steps: 1) identification of the research problem 2) conducting the literature search 3) evaluating the data 4) analyzing the data 5) presenting the results [16].
Search strategy
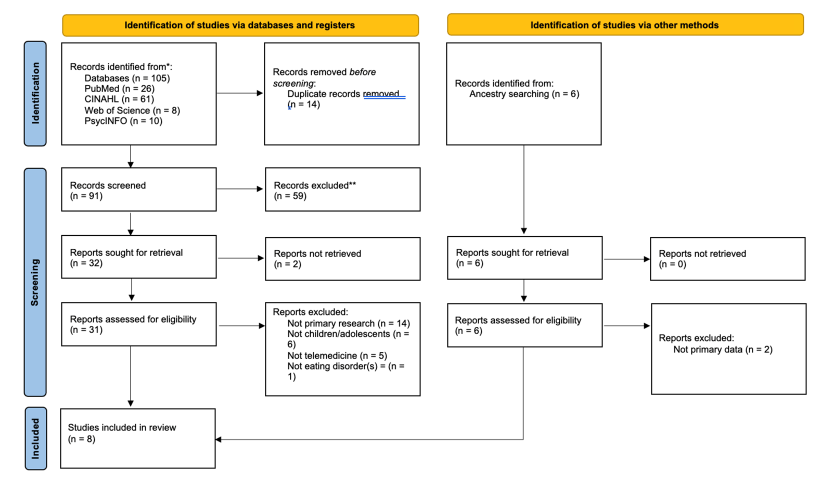
A comprehensive review of the literature was conducted in June 2024. Four online databases (PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, and Web of Science (WoS)) were searched using Medical Subject Headings (MeSH) terms relevant to the research question. Keyword searches reflected the use of telemedicine in pediatric eating disorders, including terms such as “eating disorder*”, “anorexia”, “bulimia”, and “binge eating disorder”. The population aspect was added using phrases such as “children”, “youth”, “adolescent*”, and “pediatric*”, and connected using Boolean operators. The initial search identified 105 articles (see Figure 1, PRISMA flow diagram). After duplicates were deleted (n=14), 91 records were screened at the title and abstract level, and ancestry searching was performed from the reference list.
Figure 1:PRISMA flow diagram of included studies.
Inclusion and exclusion criteria
Publications that were written in English with the full text available, featured child and/or adolescent participants, examined treating eating disorders with telemedicine, and were primary research studies published in the past 5 years were included in this review. There were no restrictions placed on country or participant gender. Studies that featured adult participants, dissertations or theses, and grey literature were excluded.
Data evaluation
Included studies were evaluated using the Critical Appraisal Skills Programme (CASP) checklist [17]. The CASP checklist is a tool designed to systematically evaluate the quality and validity of research studies by guiding users through a series of questions focused on study design, data analysis, and the applicability of findings. This systematic approach ensures that only high-quality evidence is included in the review.
Data analysis
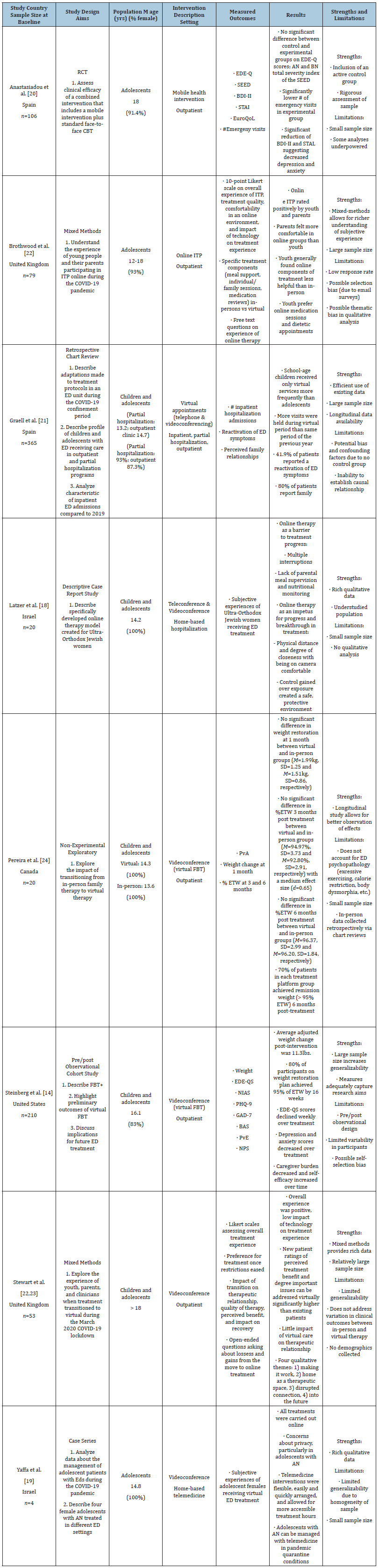
After identifying eight studies for inclusion, data were organized by aims, study design, key demographics, population, type of telemedicine, intervention description, measured outcomes, results, and limitations. A table was created to succinctly display findings (Table 1).
Table 1:Characteristics of Included Studies. ABBREVIATIONS: AN=Anorexia Nervosa; BAS=Burden Assessment Scale; BDI-II=Beck Depression Inventory-II; BN=Bulimia Nervosa; CBT=Cognitive Behavioral Therapy; ED=Eating Disorders; EDE-Q=Eating Disorder Examination Questionnaire; EDE-QS=Eating Disorder Examination-Questionnaire Short Form; ETW=Estimated Target Weight; FBT=Family-Based Treatment; FBT+=Innovative Enhanced Family-Based Treatment; GAD-7=Generalized Anxiety Disorder Questionnaire; ITP=Intensive Treatment Program; NIAS=Nine Item Avoidant/ Restrictive Food Intake Disorder Screen; NPS=Net Promoter Score; PHQ-9=Patient Health Questionnaire; PVA=Parents Versus Anorexia Scale; RCT=Randomized Controlled Trial; SEED=Short Evaluation Of Eating Disorders; STAI=State- Trait Anxiety Inventory.
Result
Setting, samples, and design
The eight studies included in this review were published between 2020 and 2023. Two studies featured Israeli participants [18,19]. An additional two studies were conducted in Spain [20,21], and two in the United Kingdom [22,23]. One study each was conducted in Canada and the United States, respectively [14,24]. The eight studies described 853 participants, with sample sizes ranging from four to 365. The studies featured predominantly female adolescents, with samples between 83% and 100% female.
The most common design type was mixed-methods studies (n=2) [22,23]. Two studies selected case reports by way of descriptive case reports study [18] and case series [19]. One study examined data through a retrospective chart review [21]. One study was an observational cohort study [14], and one was an exploratory non-experimental study [24]. Finally, only one study was a randomized controlled trial [20]. In terms of setting, the majority of studies (n=5) contained participants engaging in treatment in the outpatient setting exclusively [14,20,22-24]. Two studies used a home-based hospitalization setting [18,19]. Only one study used multiple levels of care [21] included participants in inpatient, partial hospitalization, and outpatient settings.
Quality assessment
Studies included in this integrative review were assessed using the Critical Appraisal Skills Programme (CASP) checklist (Critical Appraisal Skills Programme, 2018). The CASP checklists for randomized controlled trials were used, as well as the Joanna Briggs Institute (JBI) checklists for case reports, case series, and cohort studies (Joanna Briggs Institute, 2017). The Mixed Methods Appraisal Tool (MMAT) was used for mixed methods studies (Hong et al. 2018). All eight studies were identified as high quality. Collectively, these studies offer a well-rounded, high-quality body of evidence, supporting the efficacy and adaptability of telemedicine for treating eating disorders in youth, while highlighting cultural and situational nuances that influence treatment outcomes during global crises.
Telemedicine interventions
Types of interventions: The reviewed studies employed a range of telemedicine modalities to address eating disorders in children and adolescents, showcasing the diversity of approaches in this evolving field. Six studies focused exclusively on video telemedicine interventions, where sessions were conducted through video conferencing platforms to deliver therapy, nutritional counseling, and monitoring [14,19-21,23,24]. These interventions aimed to replicate traditional in-person treatment by enabling realtime visual and verbal interaction between patients and healthcare providers, thereby maintaining the therapeutic relationship and allowing for visual assessment of physical and psychological states.
One study [18] combined video telemedicine with telecommunications such as phone calls to provide a more flexible and accessible approach. This hybrid method allowed for continuous support and follow-up outside scheduled video sessions, catering to the varying needs and preferences of patients and families and providing culturally informed care. Another innovative approach involved online intensive programming, which included structured, multi-component treatment modalities accessed through a webbased platform [22]. This comprehensive program offered a blend of video sessions and communication with care teams, designed to provide intensive support and address the multifaceted nature of eating disorders. Collectively, these interventions demonstrate the potential of telemedicine to offer diverse, adaptable solutions for treating eating disorders in young populations, while addressing barriers associated with traditional, in-person care.
Description of interventions: Studies included in this review encompassed a variety of telemedicine interventions tailored to the complex needs of children and adolescents with eating disorders. One study [20] employed personal monitoring via a smartphone application (“app”) combined with regular sessions with therapists, where the app was used for daily self-monitoring of symptoms, mood, and eating patterns, supplemented by periodic virtual therapy sessions to provide individualized feedback and support. Another study [22] focused on virtual Intensive Treatment Programs (ITP), offering a structured and immersive approach that included daily therapeutic activities, psychoeducation, and group support sessions delivered entirely through a digital platform.
A different approach was observed in a study utilizing virtual therapy [21], which consisted of scheduled video sessions with therapists to deliver psychotherapy and nutritional counseling, mirroring traditional outpatient care in a virtual setting. One particularly innovative intervention was home-based hospitalization for Ultra-Orthodox Jewish women [18], where patients received intensive virtual care including daily video checkins with a multidisciplinary team, continuous remote monitoring, and real-time adjustments to treatment plans, effectively replicating inpatient care in the home environment. Additionally, four studies [14,19,23,24] integrated virtual family therapy, recognizing the critical role of family dynamics in eating disorder treatment. These interventions involved family-based therapy sessions conducted via video conferencing, aiming to engage family members in the treatment process, enhance communication, and provide support in managing the ED at home. Together, these interventions highlight the adaptability of telemedicine to provide diverse, effective, and accessible treatment options for young individuals struggling with EDs.
Key outcomes: Overall, studies indicated positive results both quantitatively and qualitatively. In the Anastasidou study (2020), there was no significant difference between the experimental group receiving both face-to-face therapy and a mobile health intervention and the control group receiving face-to-face therapy only on Eating Disorder Examination Questionnaire (EDE-Q) scores, reflecting the presence and severity of ED psychopathology. Additionally, they found a significantly lower number of emergency department visits, as well as decreased Beck Depression Inventory (BDI) and State-Trait Anxiety Inventory (STAI) scores, suggesting decreased depressive and anxiety symptoms. Additionally, Steinberg and colleagues (2022) identified 80% of participants receiving virtual family-based therapy reached 95% of their Estimated Target Weight (ETW) by 16 weeks of treatment, as well as decreases in EDE-Q scores weekly and depressive and anxiety symptoms, as well as decreased caregiver burden, which lends credibility to the efficacy of virtual health interventions. Another quantitative study [24] found no significant difference in weight restoration in adolescents receiving virtual therapy when compared to those receiving in-person care, as well as meeting 95% of their ETW at 3 months and 6 months post-treatment. Finally, results from Graell et al.’s study [21] found that more visits were held during the COVID-19 lockdowns necessitating virtual care than at the same time the previous year; however, there was a 41.9% reactivation of ED symptomatology, suggesting negative effects of the pandemic on the mental health of young people. Encouragingly, 80% of patients report that family relationships either remained stable or improved with the use of virtual therapies.
Qualitative and mixed-methods studies also suggested telemedicine shows great promise in the treatment of pediatric EDs. Participants in Brothwood’s [22] study rated online ITP positively by youth, however, they felt that online therapy was generally less helpful than in-person. When asked on their preference of continuing virtual care or returning to face-to-face visits, adolescents preferred in-person visits for individual and family therapy sessions, but felt that medication management and dietetic appointments would be as equally effective if kept virtual. Latzer’s [18] study found two main themes: online therapy could be either a barrier to progress in therapy, or an impetus for progress and breakthrough depending on multiple individual and familial factors. Stewart & Colleagues [22,23] found that youth receiving virtual family-based therapy felt online care was positive and reported a low impact of technology on their treatment experience, as well as on the therapeutic relationship. Finally, Yaffa’s [19] study suggested some concerns about privacy, particularly in adolescents with AN. However, participants shared that telemedicine visits were flexible, easy, and quickly arranged, which allows for more accessibility to treatment. These results underline the efficacy and acceptability of telemedicine for pediatric EDs.
Discussion
This integrative review evaluated the effectiveness of telemedicine interventions for treating eating disorders in children and adolescents, revealing several significant insights into how digital health technologies can be adapted to meet the complex needs of this population. Findings indicate that telemedicine, including video telemedicine, app-based monitoring, virtual intensive treatment programs, and home-based hospitalization holds substantial promise as a viable alternative to traditional inperson treatment modalities. Studies highlighted that telemedicine can effectively deliver key therapeutic components such as Cognitive-Behavioral Therapy (CBT), nutritional counseling, and Family-Based Therapy (FBT), comparable to traditional care. Studies focusing on video telemedicine reported similar, if not enhanced, clinical outcomes including symptom reduction, weight stabilization, and improved psychological well-being. For instance, patients receiving app-based monitoring combined with therapist sessions demonstrated high adherence to self-monitoring, which correlated with significant improvements in managing symptoms and mood [20]. Virtual ITP also showed positive outcomes, offering structured support that maintained treatment intensity and provided comprehensive care remotely [22]. Moreover, homebased hospitalization allowed for intensive care in a less restrictive environment, yielding positive clinical outcomes while minimizing the disruption to the patient’s daily life and family dynamics, allowing for culturally considerate care [18].
Engagement levels with telemedicine interventions were generally high, with several studies reporting increased accessibility and convenience as major advantages [19,20,22,23]. The flexibility of telemedicine allowed patients and families to access care without the logistical challenges associated with traditional in-person visits, such as travel time and geographic barriers. Virtual family therapy in particular enhanced family involvement in the treatment process, facilitating better communication and support within the family unit. These findings underscore the potential of telemedicine to enhance patient and family engagement, a critical factor in the successful management of pediatric EDs.
Challenges and limitations
Despite these promising results, this review also identified notable challenges associated with telemedicine interventions. Technological issues, including connectivity problems and the need for reliable internet access presented as common barriers that could hinder the effective delivery of telemedicine services. Privacy and security concerns were also significant, as the sensitive nature of eating disorder treatment requires stringent measures to ensure confidentiality. Additionally, maintaining therapeutic rapport and monitoring physical symptoms remotely posed challenges, particularly in severe cases where in-person assessment might be critical. Some studies reported difficulties in achieving the same depth of therapeutic interaction through virtual means as compared to face-to-face sessions.
Methodological considerations
The methodological quality of the included studies varied. While studies were all rated highly by standardized quality assessment checklists, some studies exhibited strong designs such as randomized controlled trials while others were limited by small sample sizes and lack of control groups. The heterogeneity in study designs and outcome measures also posed challenges for synthesizing findings. Future research should aim to standardize outcome measures and incorporate larger, more diverse samples to enhance the generalizability of results.
Conclusion
The findings of this review suggest that telemedicine can be a valuable component of a comprehensive treatment strategy for pediatric eating disorders. Its ability to provide flexible, accessible, and effective care makes it a particularly suitable option in contexts where traditional treatment approaches are limited or unavailable. However, addressing technological and methodological limitations is crucial for optimizing the delivery and efficacy of telemedicine interventions. Future research should focus on refining telemedicine models, exploring hybrid approaches that combine digital and in-person care, and investigating long-term outcomes to better understand the sustainability and impact of telemedicine on patient recovery.
In conclusion, telemedicine presents a promising avenue for treating eating disorders in children and adolescents, offering a range of benefits including enhanced accessibility, patient engagement, and the potential for effective clinical outcomes. While challenges remain, particularly concerning technology and privacy, the integration of telemedicine into eating disorder care holds potential for improving treatment delivery and addressing barriers associated with traditional in-person care. Ongoing research and innovation will be essential to fully realize the benefits of telemedicine and ensure that it can effectively complement and, in some cases, replace traditional treatment modalities.
References
- Hornberger LL, Lane MA, The Committee on Adolescence (2021) Identification and management of eating disorders in children and adolescents. Pediatrics 147(1): e2020040279.
- Kaye WH, Fudge JL, Paulus M (2009) New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci 10(8): 573-584.
- Levinson CA, Spoor SP, Keshishian AC, Pruitt A (2021) Pilot outcomes from a multidisciplinary telehealth versus in‐person intensive outpatient program for eating disorders during versus before the Covid‐19 pandemic. Int J Eat Disord 54(9): 1672-1679.
- Giel KE, Bulik CM, Fernandez AF, Phillipa H, Anna KR, et al. (2022) Binge eating disorder. Nat Rev Dis Primer 8(1): 16.
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR (2011) Prevalence and correlates of eating disorders in adolescents: results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry 68(7): 714-723.
- Tsuboi K (2005) Eating disorders in adolescence and their implications. Jpn Med Assoc J 48(3): 123-129.
- Momen NC, Plana RO, Yilmaz Z, Laura M T, John J M, et al. (2022) Comorbidity between eating disorders and psychiatric disorders. Int J Eat Disord 55(4): 505-517.
- Patel K, Tchanturia K, Harrison A (2016) An exploration of social functioning in young people with eating disorders: A qualitative study. In: Manalo (ed.) Plos One 11(7): e0159910.
- Kass AE, Kolko RP, Wilfley DE (2013) Psychological treatments for eating disorders. Curr Opin Psychiatry 26(6): 549-555.
- Reiter CS, Graves L (2010) Nutrition therapy for eating disorders. Nutr Clin Pract 25(2): 122-136.
- Zhu AJ, Walsh BT (2002) Pharmacologic treatment of eating disorders. Can J Psychiatry 47(3): 227-234.
- Hamilton A, Mitchison D, Basten C, Byrne S, Goldstein M, et al. (2022) Understanding treatment delay: perceived barriers preventing treatment-seeking for eating disorders. Aust N Z J Psychiatry 56(3): 248-259.
- Norman S (2006) The use of telemedicine in psychiatry. J Psychiatr Ment Health Nurs 13(6): 771-777.
- Steinberg D, Perry T, Freestone D, Bohon C, Baker JH, et al. (2023) Effectiveness of delivering evidence-based eating disorder treatment via telemedicine for children, adolescents, and youth. Eat Disord 31(1): 85-101.
- Gorrell S, Reilly EE, Brosof L, Le Grange D (2022) Use of telehealth in the management of adolescent eating disorders: patient perspectives and future directions suggested from the covid-19 pandemic. Adolesc Health Med Ther 13: 45-53.
- Whittemore R, Knafl K (2005) The integrative review: updated methodology. J Adv Nurs 52(5): 546-553.
- (2023) Critical Appraisal Skills Programme.
- Latzer Y, Herman E, Ashkenazi R, Atias O, Laufer S, et al. (2021) Virtual online home-based treatment during the covid-19 pandemic for ultra-orthodox young women with eating disorders. Front Psychiatry 12: 654589.
- Yaffa S, Adi EL, Itai P, Marit JM, Doron G, et al. (2021) Treatment of eating disorders in adolescents during the COVID-19 pandemic: A case series. J Eat Disord 9(1): 17.
- Anastasiadou D, Folkvord F, Brugnera A, Laura CV, Eduardo ST, et al. (2020) An mhealth intervention for the treatment of patients with an eating disorder: A multicenter randomized controlled trial. Int J Eat Disord 53(7): 1120-1131.
- Graell M, Morón NMG, Camarneiro R, Ángel V, Silvia Y, et al. (2020) Children and adolescents with eating disorders during COVID‐19 confinement: Difficulties and future challenges. Eur Eat Disord Rev 28(6): 864-870.
- Brothwood PL, Baudinet J, Stewart CS, Simic M (2021) Moving online: young people and parents’ experiences of adolescent eating disorder day programme treatment during the COVID-19 pandemic. J Eat Disord 9(1): 62.
- Stewart C, Konstantellou A, Kassamali F, Natalie M, Darren C, et al. (2021) Is this the ‘new normal’? A mixed method investigation of young person, parent and clinician experience of online eating disorder treatment during the COVID-19 pandemic. J Eat Disord 9(1): 78.
- Pereira J, Boachie A, Shipley C, McLeod M, Garfinkel S, et al. (2023) Paediatric eating disorders: exploring virtual family therapy during a global pandemic. Early Interv Psychiatry 17(7): 743-746.
© 2024 Katelin A Crane. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






