- Submissions

Full Text
Trends in Telemedicine & E-health
Managing Health Risks in Remote Communities Through Advancements in e-Health and Remote Medicine
Michael G Tyshenko*
Senior Risk Analyst, Risk Sciences International, Canada
*Corresponding author:Michael G Tyshenko, Senior Risk Analyst, Risk Sciences International, Ottawa, Canada
Submission: June 24, 2024; Published: June 28, 2024

ISSN: 2689-2707 Volume 5 Issue 1
Opinion
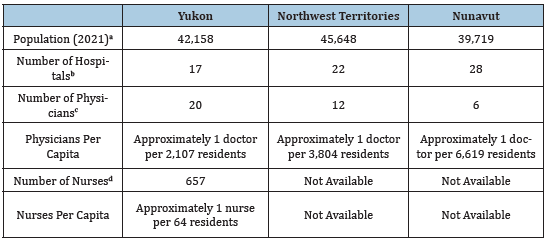
The correlation between early access to healthcare services and improved patient outcomes is undeniable. Timely and accessible healthcare saves lives by ensuring that health issues are addressed early and it results in fewer downstream costs to Canadian healthcare systems. Early interventions lead to reduced hospitalizations, less aggressive and costly treatments, and an overall decrease in healthcare expenses. This not only results in better patient outcomes but also promotes the efficient allocation of healthcare resources which benefits both patients and the healthcare system as a whole. In Canada, roughly 15% of the population in provinces do not have access to a regular medical doctor. Due to their remoteness, northern territories have considerably less access. In the Yukon 17% of residents lack a family doctor, in the Northwest Territories this jumps to 48%, and in Nunavut it is more than 80% [1,2] (Table 1).
Table 1:The dire situation when it comes to per capita access to doctors and nurses in the more remote regions of Canada: Yukon, Northwest Territories and Nunavut.
a-Statistics Canada (2023). Census Profile, 2021. Census of Population. Available
online: https://www.statista.com/statistics/440923/total-number-of-hospitalestablishments-
in-canada-by-province/.
b -Statista (2023). Number of hospital establishments in Canada as of 2021, by
province. Available online: https://www.statista.com/statistics/440923/totalnumber-
of-hospital-establishments-in-canada-by-province/.
c–CIHI. (2023). Number of physicians and nurses per 10,000 population by
health region, 2021 (All physicians). Canadian Institute for Health Information.
Available online: https://www.cihi.ca/en/number-of-physicians-and-nursesper-
10000-population-by-health-region-2021.
d-CIHI. (2023). Number of physicians and nurses per
10,000 population by health region, 2021 (All nurses).
Canadian Institute for Health Information. Available
online: https://www.cihi.ca/en/number-of-physiciansand-
nurses-per-10000-population-by-health-region-2021.
Managing health risks in remote communities through e-Health and remote medicine is one way to bridge the gap. Some e-Health programs are already unevenly established in Canada’s territories including: Telehealth consultations; virtual pharmacy consultations and E-prescriptions; Community Health Workers (local residents employed with access to telemedicine tools to provide basic care); mental health services delivered by telemedicine; and Store-and- Forward Telemedicine (patients capture images, videos, or data related to their health condition and send it to healthcare providers for review, diagnosis and guidance). Future advancements for remote medicine in Canada’s territories include a number of other devices and strategies. Advancements include wearable monitoring devices for chronic disease management; mobile health units staffed with trained medical personnel; the potential use of drones to deliver emergency medicines; tele-rehabilitation services; and the increased use of e-Health apps for healthcare information tracking and appointment scheduling.
The increased use of Collaborative Care Networks that connect local territorial healthcare providers with specialists from provincial urban centers through virtual conferences and consultations is another avenue to improve remote healthcare access. “Lab-on-chip” diagnostic platforms with mobile interfaces offer the interesting prospect of performing diagnostic tests remotely. These platforms which currently are not used for remote diagnostics can already detect infectious diseases such as influenza virus and SARS‑CoV‑2 (the COVID-19 virus), and the technology’s potential could detect a broader range of pathogens, including cancer [3].
One of the most promising areas in remote telemedicine is the development of Artificial Intelligence (AI)-powered medical avatars. An example is iCare Navigator, which draws upon a patient’s electronic medical records to build a personalized relationship, gradually determining when a patient is most receptive to learning about a health condition or care management [4]. Medical avatars using AI are still in the early stages of development but even now have the level of sophistication to provide guided telemedicine support that could consolidate most of the currently available remote telemedicine programs. In remote areas of Canada, the absence of healthcare professionals and infrastructure is acutely felt. The development of innovative remote medical services delivery will not only save lives but will also bridge critical healthcare gaps.
References
- Government of Yukon (2023) Government of Yukon increases access to primary healthcare providers.
- Giles S (2017) The North Needs More Doctors. The Walrus.
- Papamatthaiou S, Boxall-Clasby J, Douglas EJA, Jajesniak P, Peyret H, et al. (2023) LoCKAmp: lab-on-PCB technology for <3 minute virus genetic detection. Lab Chip 23(20): 4400-4412.
- Kiger P (2018) Animated Avatars Guide Hospital Patients’ Recoveries. AARP.
© 2024 Michael G Tyshenko. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






