- Submissions

Full Text
Trends in Telemedicine & E-health
Correlation Research on Memory Deficits and Depression among Young Adults
Neethu George* and Rosalito De Guzman
The Graduate School, University of Santo Tomas, Philippines
*Corresponding author:Neethu George, The Graduate School, University of Santo Tomas, Manila, Philippines
Submission: August 28, 2023; Published: August 30, 2023

ISSN: 2689-2707 Volume 4 Issue 4
Abstract
Empirical evidence that depression can affect daily memory is a vital component of the current study. The high prevalence of depression in young adults frequently has a negative impact on their lives. In addition, depression and PRMQ were examined. Depression and PRMQ had a strong positive correlation. Early prevention is therefore necessary, and more studies are needed to increase public awareness of this problem. The extensive literature demonstrates that memory problems are caused by depression in young adults. This study investigates the relationship between young adult memory problems and depression. The correlation between depression and PRMQ was evaluated among 497 young adults from India. Data were gathered using the Beck Depression Inventory (BDl-11) and the Prospective and Retrospective Memory Questionnaire (PRMQ). The Pearson correlation coefficient showed a very strong positive correlation of .989 between the two variables. This study highlights the serious threat to public health and the expanding issue of depression and urges the implementation of an effective intervention program intended to improve young adults’ memory.
Keywords:Depression; Memory; Young adults; Correlation
Introduction
Depression is one of the most pervasive and detrimental types of psychopathology LeMoult et al. [1]. According to the WHO [2], the disorder affects 5% of adults worldwide. It ranks first in middle-and high-income countries and is the third most common disease worldwide. It is the leading global cause of disability-adjusted life years among those aged 10 to 24 Therese [3]. Depression is linked to mild-to-moderate impairment in a number of cognitive functions, including executive functioning, attention, and memory Chen et al. [4]. Cognitive deficits are a significant aspect of depression and may continue to be impaired even after recovery Priyamvada et al. [5]. Afridi et al. found that cognitive impairment affects up to two-thirds of depressed patients, including those experiencing their first episode and those who are in remission Zhou et al. [6]. Memory complaints are grouped with depressive symptoms that are used to diagnose depression, but they can also be an early sign of cognitive decline or simply part of aging. According to Mogle et al. [7], memory problems frequently have stronger associations with depressive symptoms than with objective cognition. In daily life, it is inevitable to deal with information about future actions or events that must be remembered and properly recalled at a specific time or moment. As a result, Long-Term Memory (LTM) has recently been classified in accordance with the temporal direction of memory traces Matos et al. [8].
Retrospective Memory (RetM) refers to remembering something from the past, whereas Prospective Memory (ProM) refers to having the intention to remember something in the future Gao et al. [9] our capacity to function and lead healthy lives is significantly impacted by both types of memory Uttl et al. [10]. Covich, and Hedlund also found that clinically depressed adults showed worse ProM and less effective time-monitoring behavior Jeong et al. [11]. Pathological projections from the amygdala to the Anterior Cingulate Cortex (ACC) and the Prefrontal Cortex (PFC), which are implicated in ProM, are thought to be the basis for neuropsychological dysfunctions in depression. The observed effects of depression on ProM may be mediated by the top-down cognitive control function because these brain regions are a part of widely dispersed networks of attention and executive function Chen et al. [4].
A research study Miles et al. [12] revealed that decrease in optimistic memories and expectations is associated with depression. Elliott et al. [13] suggested that depression is associated with altered cognitive and affective processing as well as other changes in memory function. For instance, people who are depressed are more likely than people who are not depressed to recall memories that are more negative. The lack of specificity in autobiographical memories is another memory phenomenon seen in depressed people. These departures from normal memory performance point to a problem with basic memory function and/ or the way affective information is processed. Affective information is better remembered compared to neutral information, according to research on memory for affective stimuli and events more typically Schweizer et al. [14].
Adults who are depressed typically exhibit impaired memory, better memory for negative material but worse memory for positive material when compared to healthy adults Dillon et al. [15]. In addition to triggering depression, major life stress may also alter the structure of the hippocampus by activating the receptors for glucocorticoids, which are prevalent in this area of the brain Dillon et al. [15]. The meta analytic study Geerlings et al. [16] have confirmed that the hippocampus of people with depression is smaller than that of healthy people. Reduced grey matter in the hippocampus, which is connected to memory and intricate cognitive functions, may be related to the negative emotions and diminished cognition in depressed patients Dillon et al. [15]; Rădulescu [17] & Royuela-Colomer et al. [18]. The neuroplasticity capacity of the brain is compromised in depressive disorders, which includes issues with the hippocampus Rădulescu et al. [17] Everyday life depends heavily on memory. Therefore, the current study’s objective is to investigate the connection between young adults’ depression and memory deficits. Method 497 adults between the ages of 18 and 25 who attended various colleges and who used purposive sampling techniques participated in the study. More specifically, the study will be conducted in Kerala, India, at various colleges. The following inclusion criteria were used to select young adults at random: young adults from the various colleges in the Indian state of Kerala, participants between the ages of 18 and 25, young adults who can communicate in English, and young adults who volunteered and expressed interest in taking part in the study. The participants gave their informed consent before completing the surveys and assessment tools. The UST Graduate School Review Ethics Committee’s (USTGS-REC) permission was obtained before the research could be conducted because of ethical concerns.
Research Design
The study investigated the relationship between memory deficits and depression using a correlational research methodology.
Instruments
Personal information sheet: For the personal datasheet, the researcher created a demographic questionnaire. The respondents’ socio-demographic profiles were accurately described by the personal data sheet, which also made it easier to gather important data and included and excluded study participants.
Beck Depression Inventory (BDI-II): The BDI-II is a 21-item self-report scale that is used to assess how severe depression symptoms are. The total score ranges from 0 to 63, and each item is graded from 0 to 3 in accordance with general guidelines. The higher the score, the more severe the depressive symptoms. When compared to other depression measures, the BDI-II has excellent criterion validity (=0.94) and good internal consistency (Cronbach’s alpha=0.83) Lee et al. [19]
The Prospective and Retrospective Memory Questionnaire (PRMQ): Participants answered questions on the PRMQ, which rates the frequency of memory problems in daily life on a scale from 1 (“never” to “very often”). Eight items from the past and eight from the future make up the PRMQ. All analyses used the raw scores from each PRMQ item (Cronbach’s alpha = 0.94) Sheppard et al. [20].
Procedure
An approach known as correlational research was used to examine the relationship between depression and PRMQ. A form asking for informed consent was given to participants. The questionnaire was given to the students who expressed an interest in participating. The information was coded and entered into the computer after the questionnaires had been completed. SPSS software, descriptive statistics, and Pearson correlation tests were used to analyze the data.
Result and Discussion
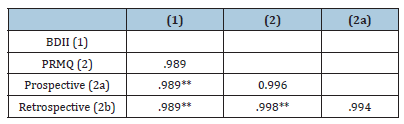
In this study, the researcher looked to see if there was any correlation between depression and PRMQ. The initial hypothesis postulated a connection between depression and PRMQ. A popular correlation metric for determining a linear correlation is Pearson’s correlation coefficient (PCC). The strength and direction of the relationship between two variables is expressed as a number between -1 and 1. Both variables change in the same way when one of them is altered. A statistically significant association between depression and PRMQ was discovered by the researcher. Table 1, shows that there was a strong, positive correlation between depression and PRMQ, which was statistically significant (r =.989, n = 497, p =.01). Table 1 also shows the mean scores and standard deviations for the variables BDI II and PRMQ. It implies that memory problems also worsen when depression does, and vice versa.
Table 1: Descriptive Statistics of Depression and
Dimensions of PRMQ.
Std. Deviation -Standard deviation
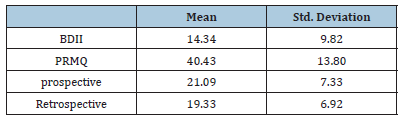
The PRMQ’s prospective memory (ProM) and retrospective memory (RetM) dimensions both have values of.989 and. 989 that are significantly positively correlated with depression. Validation of the study’s hypotheses revealed a significant and strongly positive association between BDI II and PRMQ. The mean scores and standard deviations for the BDI II and PRMQ variables are displayed in Table 2. The BDI II measure has a mean score of 14.34 and a maximum score of 55. 9.82 is the standard deviation. The PRMQ measure has a mean score of 40.43, a range of 80, and a standard deviation of 13.80.
Table 2: Correlation between Depression and Dimensions
of PRMQ.
**p<0.01 (2-tailed); n=497
The findings supported the relationship between memory problems and depression. A significant, positive correlation between the two variables depression and PRMQ showed that memory problems increased along with the risk of depression. The research’s findings supported the hypotheses. The findings showed a strong relationship between depression and young adults’ PRMQ. The findings are in line with a previous study Mogle et al. [7], which suggested that depressive symptoms and memory complaints are frequently linked and may both be signs of impending cognitive decline.
According to the findings of a different study, memory complaints also appeared to be more frequent when depressive symptoms were Mogle et al. [7]. Yoon et al. [21] came to the conclusion that reporting more frequently occurring forgetting incidents and a greater decline in memory function were related to having more depressive symptoms. Memory issues likely make depression worse Dillon et al. [15], but depression also has an impact on memory. The results of the current study concur with those of Schweizer et al. [14] who found that subclinical depressive symptoms are correlated with an increase in the frequency of selfreported memory problems.
The study’s conclusions are anticipated to offer doctors and mental health professionals’ new knowledge and a suggestion that PRMQ be taken into account when evaluating young adults who may be at risk for depression. Adults who are depressed typically exhibit impaired memory, better memory for negative material but worse memory for positive material when compared to healthy adults Dillon et al. [15]. Working memory issues are linked to depressive symptoms. This study Royuela-Colomer et al [18] looked at emotional working memory in 92 adults with depressive symptoms. According to Kizilbash et al. [22] there is a strong correlation between depression and memory loss. The study’s findings showed that depressive symptoms (without anxiety) have a negative impact on new information’s ability to be immediately recalled as well as its quantity rather than its rate of acquisition. Deficits in cognition, such as memory loss, can also lead to depression. Mild cognitive impairment (MCI) has been noted as a potential risk factor for the development of depression in a recent population-based longitudinal study, suggesting that declining cognitive function may be the root cause of the unfavorable emotions associated with depression James et al. [23].
Conclusion
According to the current research, there is a significant positive correlation between depression and PRMQ. Although the results are constrained by the small sample size and cannot be generalized to the entire population, they may be useful in directing future research on young adults’ depression and PRMQ. The results of our study highlight the urgent need for effective intervention.
References
- LeMoult J, Gotlib IH (2019) Depression: A cognitive perspective. Clinical Psychology Review 69: 51-66.
- (2021) World Health Organization (WHO).
- Therese W (2018). Depression among adolescents and young adults: social and gender differences. Solna pp. 1-99.
- Chen S, Zhou R, Cui H, Chen X (2013) Deficits in cue detection underlie event-based prospective memory impairment in major depression: An eye tracking study. Psychiatry Research 209(3): 453-458.
- Priyamvada R, Ranjan R, Chaudhury S (2015) Cognitive rehabilitation of attention and memory in depression. Industrial Psychiatry Journal 24(1): 48-53.
- Zhou FC, Wang YY, Zheng W, Zhang Q, Ungvari GS, et al. (2017) Prospective memory deficits in patients with depression: A meta-analysis. Journal of Affective Disorders 220: 79-85.
- Mogle J, Hill NL, Bhargava S, Bell TR, Bhang I (2020) Memory complaints and depressive symptoms over time: A construct-level replication analysis. BMC Geriatrics 20(1): 57.
- Matos P, Albuquerque PB (2021) From retrospective to prospective memory research: A framework for investigating the deactivation of intentions. Cognitive Processing, 22(3): 411-434.
- Gao H, Xia Q, Zhang X, Chen Y, Yan J, et al. (2023) Intermediary roles of prospective memory and retrospective memory in the comorbidity of depression and pain. General Psychiatry 36(1): e100895.
- Uttl B, White CA, Cnudde K, Grant LM (2018) Prospective memory, retrospective memory, and individual differences in cognitive abilities, personality, and psychopathology. Plos One 13(3): e0193806.
- Jeong JM, Cranney J (2009) Motivation, depression, and naturalistic time-based prospective remembering. Memory 17(7): 732-741.
- Miles H, MacLeod AK, Pote H (2004) Retrospective and prospective cognitions in adolescents: Anxiety, depression, and positive and negative affect. Journal of Adolescence 27(6): 691-701.
- Elliott R, Rubinsztein JS, Sahakian BJ, Dolan RJ (2002) The neural basis of mood-congruent processing biases in depression. Archives of General Psychiatry 59(7): 597-604.
- Schweizer S, Kievit RA, Emery T, Henson RN (2018) Symptoms of depression in a large healthy population cohort are related to subjective memory complaints and memory performance in negative contexts. Psychological Medicine 48(1): 104-114.
- Dillon DG, Pizzagall DA (2018) Mechanisms of Memory Disruption in Depression. Trends in Neurosciences 41(3):13-149.
- Geerlings MI, Gerritsen L (2017) Late-life depression, hippocampal volumes, and hypothalamic-pituitary-adrenal axis regulation: A systematic review and meta-analysis. Biological Psychiatry 82(5): 339-350.
- Rădulescu I, Drăgoi AM, Trifu SC, Cristea MB (2021) Neuroplasticity and depression: Rewiring the brain’s networks through pharmacological therapy (Review). Experimental and Therapeutic Medicine 22(4): 1131.
- Royuela-Colomer E, Wante L, Orue I, Braet C, Mueller SC (2022) Comparing emotional working memory in adolescents and young adults with and without depressive symptoms: Developmental and psychopathological differences. BMC Psychology, 10(1): 134.
- Lee K, Kim D, Cho Y (2018) Exploratory factor analysis of the beck anxiety inventory and the beck depression inventory-ii in a psychiatric outpatient population. Journal of Korean Medical Science 33(16): e128.
- Sheppard DP, Gallagher MW, Morgan EE, Outlaw AY, Naar S, et al. (2022) “Do i have a memory problem? i can’t recall”: An evaluation of measurement invariance in subjective reporting of memory symptoms among persons with and without objective HIV-associated memory impairment. Journal of the International Neuropsychological Society : JINS 28(2): 166-176.
- Yoon JA, Kong IJ, Choi J, Baek JY, Kim EJ, et al. (2019) Neural compensatory response during complex cognitive function tasks in mild cognitive impairment: A near-infrared spectroscopy study. Neural Plasticity 1-8.
- Kizilbash AH, Vanderploeg RD, Curtiss G (2002) The effects of depression and anxiety on memory performance. Archives of Clinical Neuropsychology 17(1): 57-67.
- James TA, Weiss-Cowie S, Hopton Z, Verhaeghen P, Dotson VM, et al. (2021) Depression and episodic memory across the adult lifespan: A meta-analytic review. Psychological Bulletin 147(11): 1184-1214.
© 2023 Neethu George. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






