- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Intramedullary Mature Teratoma in an Adult Patient
Velinov N1*, Petrov M1, Dochkova M2, Kamenova M2 and Gabrovsky N1
1Department of Neurosurgery, Bulgaria
2Department of Pathology, Bulgaria
*Corresponding author: Velinov N, Department of Neurosurgery, Bulgaria
Submission: December 21, 2020;Published: January 15, 2021

ISSN 2637-7748
Volume4 Issue1
Abstract
Teratoma is a type of tumor that contains a mixture of multiple germinal layers. Mature teratomas are relatively less common than the immature form and contain fully differentiated adult type tissue elements from the three germinal layers. Only 0.15-0.18% of spinal tumors are classified as teratomas. Until now only around 40 cases have been reported and most of them located in the thoracolumbar region. Preservation of neurological function is of utmost importance during the surgical removal of these lesions. Therefore, the application of intraoperative electrophysiological monitoring is mandatory. The drop in electrical potentials during surgery might lead to only partial resection of the intramedullary teratomas, which is documented in around one third of the cases so far. However, even with a partial resection the recurrence rate of these lesions is very low.
Keywords: Intramedullary teratoma; Rare spinal cord tumors; Mature teratoma
Introduction
Teratoma is a type of tumor that contains a mixture of multiple germinal layers. Teratomas are classified as mature, immature, or malignant depending on the degree of differentiation. Immature teratomas contain neuroepithelial cells that retain embryonal characteristics. Mature teratomas are relatively less common than the immature form and contain fully differentiated adult type tissue elements from the three germ layers. Only 0.15-0.18% of spinal tumors are classified as teratomas. In the pediatric population 5-10% of the intraspinal tumors are represented by the intraspinal teratomas [1-4]. In 1863 Virchow described for the first time a teratoma within the spine [5]. Since then only a few cases have been reported. In 1931 the first proven case of an intramedullary mature teratoma was presented by Hosoi. Until 2006 only 29 (20 males/9 females) adult intramedullary mature teratomas were identified in the literature [1]. Until now only around 40 cases have been reported. The lesions were mainly located in the thoracolumbar region.
Case Report
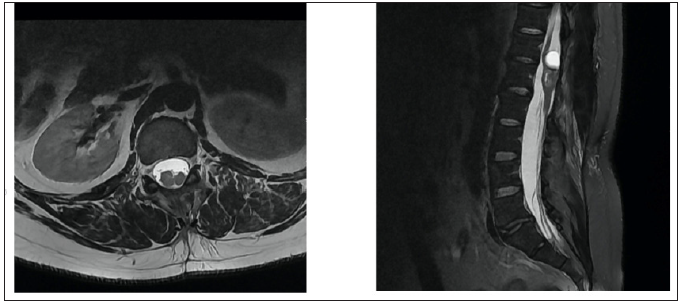
A 34-year-old male patient presented with a few months’ history of back pain. The patient had been treated with non-steroidal anti-inflammatory drugs (NSAIDs) for a few weeks in an outpatient clinic by a neurologist. Despite the treatment the back pain became constant and the patient started experiencing weakness in both legs while climbing stairs. The patient was referred for magnetic resonance imaging (MRI) of the thoracolumbar region (Figure 1 & 2). The MRI scan showed a multicompartmental heterogeneously enhanced intramedullary lesion located along Th12 and L1 vertebral bodies. A computed tomography angiography scan was also conducted and revealed neither spinal dysraphism, nor pathological vascular nidus. The patient was admitted to the Department of Neurosurgery in our hospital with spastic lower paraparesis (3 out of 5 on the muscle strength scale), bilateral positive Babinski sign, bilateral hypoesthesia below L1 dermatome, proprioceptive dysfunction in the lower extremities. Surgical treatment was suggested aiming for neural decompression, histologic verification and resection of the lesion. Laminectomies of Th12, L1 and partially on Th11 and L2 were conducted. Motor evoked potentials (MEPs) were monitored during the operation (Figure 3). The tumor was partially removed due to its adherence to the surrounding spinal cord and temporary deterioration of MEPs during surgical resection (Figure 4). The dura mater was closed with a watertight running suture and sealed with autologous fibrin glue. The histological examination revealed a mature teratoma (Figure 5). The patient had an uneventful postoperative period and was ambulating independently/muscle strength 5 out of 5/ on the 7th postoperative day. Control MRI was conducted 1 month postoperatively (Figure 6).
Figure 1: Preoperative axial reconstructions or T I -weighed MR-images with contrast enhancement and T2 -weighted M R-images of the spine at L1 vertebral body. A heterogenous cystic lesion with scarce contrast enhancement is observed is Th12-Ll level
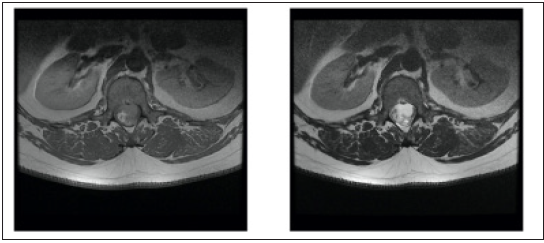
Figure 2: preoperative sagittal reconstructions of T1-weighted MR-images with contrast enhancement and T2 weighted MR-images of the lumber spine region. An intramedullary lesion with multiple cysts is observed end considerable compression of tbc medulla.

Figure 3: (3.1) Preoperative control MEPs. (3.2) MEPs at the end of the operation.

Figure 4: Intraoperative finding cartilage-like lesion.
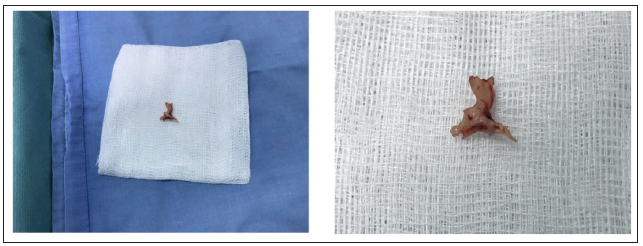
Figure 5: Histoloyical specimens from the removed intramedullary teratoma. A&B Well differentiated glandular structures surrounded by mesenchymal cells and adipose tissue. HE, 4x and 10x magnification. C Synaptophysin staining, 4x magnification, positive reaction in mature neural tissue. D: Cartilage and adipose tissue, HE, 4x magnification.

Figure 6: Post-operative axial reconstruction of T2-weighted MR-image of the spine at L1 vertebral body level and sagittal reconstruction Df T2-weighted MR-image of the spine.
Discussion
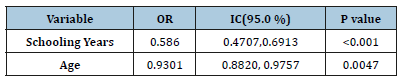
Spinal teratomas are uncommon lesions. According to the current classification they are composed of derivatives from all three primitive germ layers. So far two theories try to explain the origin of the spinal teratomas-disembryogenic theory that is widely accepted and the misplaced germinal cell theory that was proposed by Barahona [3]. The main difference between them is that the first is associated with spinal dysraphism while the latter is not. Magnetic resonance imaging is the most valuable imaging modality for establishing the diagnosis, but it cannot readily differentiate teratomas from other intramedullary lesions. Definitive diagnosis is only possible with histopathological examination. The primary treatment for spinal teratomas is surgery. Spinal teratomas are usually composed of solid and cystic components. Special attention should be kept while dissecting the cystic component. The spillage of the contained liquid in the subarachnoid space could be the cause of aseptic meningitis /a.k.a Mollaret’s meningitis due to the large mononuclear cells called Mollaret cells/ [3]. Total surgical removal should be the goal but cannot always be achieved due to the adherence of the lesion to the surrounding spinal cord tissue. According to Li et al from 2013 for the period 1928-2013 have been reported only 28 cases of mature spinal teratoma and around 30% of them have been partially resected [6]. According to Ak H [1] until 2006 only 29 cases of intramedullary teratoma have been reported including some found at autopsies. Of those again around 30% have been incompletely resected. In our review of the literature 19 out 42 cases were partially removed (Table 1). Preservation of the neural structures and their function should always be a main goal during such operations. Thus, application of intraoperative electrophysiological monitoring is mandatory. It is essential to resect the tumor as extensive as possible according to the electrophysiological findings – removal of the tumor should be stopped whenever there is a risk for loss of neurological function. According to the literature, recurrence rates for mature teratomas are very low even in cases with subtotal resection. In the series of Sharma [7-9] for the period 1987-2001 they operated on 10 cases and had only 1 recurrence 9 years after the first operation. Whenever there is a malignant component in the histopathological specimen, radiotherapy could be considered as an adjuvant treatment [4]. However, radiotherapy is not recommended for mature teratomas [10].
Table 1:
References
- Ak H, Ulu M, Sar M, Albayram S, Aydin S, et al. (2006) Adult intramedullary mature teratoma of the spinal cord: review of literature illustrated with an unusual example. Acta Neurochir 148(6): 663‑66
- Ariñez BE, Esqueda LMA, Navarro OJL (2016) A special case of intramedullary teratoma in an adult: case report and literature review. Rev Mex Neuroci 17(5): 124-133.
- Borlot, Felippe S, Matheus E, Adriana M, Hamilton T, et al. (2009) Intramedullary spinal teratoma: A rare condition with a good outcome. Arquivos de neuro-psiquiatria 67: 733-735.
- Ariñez B, Navarro O, Esqueda L, Muñoz C, González E, et al. (2018) A special case of intramedullary teratoma in an adult. Literature review. Revista Médica del Hospital General de México 81(4): 237-242.
- Li Y, Yang B, Song L, Yan D (2013) Mature teratoma of the spinal cord in adults: an unusual case. Oncol Lett 6(4): 942-946.
- Nsir AB, Hammouda KB, Said IB, Kassar AZ, Kchir N, et al. (2015) Spinal intradural mature teratoma in an elderly patient. J Cancer Metastasis Treat 1: 106-110.
- Saridakis N, Koumantzia C, Libard S, Marklund N, Eleftheriou A (2020) Intramedullary holocord mature teratoma in an adult- case report and review of the literature. Clin Neurol Neurosurg 195: 105925
- Sharma, Minakshi, Aggarwal M, Ralte A, Vaishya V, et al. (2003) Clinicopathological study of spinal teratomas a series of 10 case. Journal of Neurosurgical Sciences 47(2): 95-100.
- Vanguardia MK, Honeybul S, Robbins P (2014) Subtotal resection of an intradural mature teratoma in an adult presenting with difficulty initiating micturition. Surg Neurol Int 5: 23.
- Virchow, Rudolf (1863) Die krankhaften geschwulste.
© 2020 Velinov N. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






