- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Calcified Chronic Subdural Hematoma
Gomez fortty mariadelos angeles1*, Gonzalez EKB1* and Esqueda LMA2*
1Neurosurgery department, San francisco clinic hospital, Ecuador
2Head of the department of neurosurgery naval medical center of mexico
*Corresponding author: Gómez Fortty María delos Angeles and González Echeverría Kléber Eduardo, Neurosurgery department, San francisco clinic hospital, Ecuador Esqueda Liquiano Mauricio Armando, Head of the department of neurosurgery naval medical center of mexico
Submission: August 13, 2020;Published: October 09, 2020

ISSN 2637-7748
Volume3 Issue4
Medical Image
Simple skull tomography
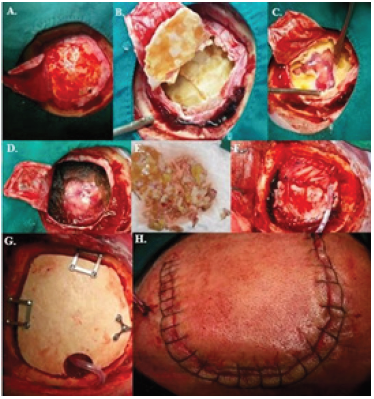
An isodensal image with a wide area of perimeter calcification of left frontoparieccipital extraxial location is observed in a 68-year-old male patient entering with generalized tonic-clonic seizure box, hemiplegia on the right side due to a reduction in brain tissue of up to 200 g, with an increase in extra-brain space by 6 to 11 % allowing parenchyma to adapt to the hematoma and that it is stood (Figure 1). The clinical presentation of this pathology is often insidious, with symptoms of decreased level of consciousness, problems in gait due to changes in balance, cognitive dysfunction, memory loss, motor deficit (hemiparesias), headache, or aphasia [1,2]. With the presumptive diagnosis, a left parietal craniotomy was performed, through which an encapsulated and calcified lesion was exposed in its entire parietal and visceral face, and that contained a granular substance of dark red color, totally avascular. Radical resection was performed without surgical complications (Figure 2). Final result, successful patient surgical ablation without seizures, regained strength 5/5 in right hemibody, oriented and conscious. It is concluded that chronic subdural hematomas calcification is a rare form of imaging presentation today, known as armoured brain or matryoska brain [3]. Since pseudomembrans are calcified, the chances of brain re-explosion are virtually non- existent [4]; Finally, the decision of the surgery conforms to the clinical or radiological evidence of mass effect. When there is evidence and the need for a craniotomy approach it could be a better option than trepanation in the management of these entities [4,5].
Figure 1:
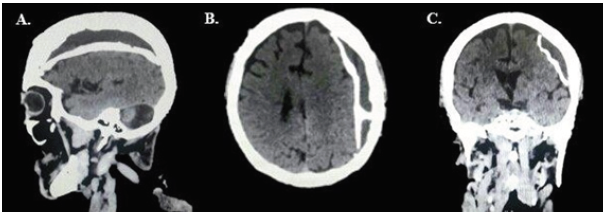
Figure 2: Craniotomy plus capsulotomy for evacuation of chronic subdural hematoma calcified in 68-yearold patient. (A) Dural opening, (B)Chronic calcified subdural hematoma, (C)Release of chronic calcified subdural hematoma of the cerebral parenchyma, (D) Surgical bed hemostasis, (E)fragments of retired calcified subdural hematoma, (F)Dural closure, (G) Placement of bone flap fixed with microplates, (H) Surgical boarding closure.
References
- Ortega SO, Gil Alfonso M, Bacallao GL, Hechevarría AJ, García DM, et al. (2019) Diagnóstico del hematoma subdural: unproceso de clínica e imágenes diná Rev Med Electrónabril 41(2).
- Balser D, Farooq S, Mehmood T (2015) Traumatismo craneoencefálico en el adulto mayor. J Neurosurg 1(7).
- Arán Echabe E, Fieiro Dantes C, Prieto Gonzales Á (2014) Hematoma subdural crónico calcificado: cerebro blindado. Rev Neurolenero 58(9).
- Santarias T, Kolias A, Hutchinson P (2012) Surgical management of chronic subdural hematoma in adults. Operative Neurosurgical Techniques pp. 1573-1578.
- García Pallero M, Pulido Rivas P, Pascual Garvi J, G Sola R (2014) Hematomas subdurales cronicos. La arquitectura interna del hematoma como predictor de recurrencia. Rev Neurol octubre 59(7).
© 2020 Bitsoev Vladimir Dodtievich. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






