- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Applications of the AnastoClip® for Neurosurgical Interventions
Wolff Kirsch* and Justin Brier-Jones2
Director, Neurosurgery Center for Research, Training and Education, Loma Linda University, USA
*Corresponding author: Wolff Kirsch, Director, Neurosurgery Center for Research, Training and Education, Loma Linda University, 11234 Anderson Street, Room A537, Loma Linda, CA 92354
Submission: February 03, 2018; Published: March 06, 2018

ISSN 2637-7748
Volume1 Issue3
The AnastoClip Closure System: Technology
The concept of an easily applied non-penetrating microclip was born from the frustrations of attempting neurosurgical microvascular anastomoses with needle and suture for bypass procedures. The doubts, failures and frustrations associated with suturing the thick-walled superficial temporal artery to a thin- walled brain cortical artery to increase brain oxygenation stimulated development of this device. A non-penetrating titanium microclip for joining vessels 1-3 mm in diameter was readily constructed with precision electrolytic metal cutting technology originally developed by Swiss watchmakers. The problem was developing an easily loaded applier to enable rapid and reproducible clip application. My patent for this vascular closure system was issued to the University of New Mexico, and taken over by the United States Surgical Corporation for preclinical testing, production and marketing. The patent was subsequently sold to the LeMaitre Vascular Corporation. Though originally designed for microvascular surgery, the greatest application has been for microvascular anastomoses:arteriovenous fistulas for hemodialysis. The microclip marketed by LeMaitre Vascular has been found to be a valuable technical resource for difficult neurosurgical cases and is FDA approved for closure of all tubular structures. The AnastoClip® Closure System is now proven to be a unique tactical advancement for the treatment of emerging neurosurgical issues. Though the superficial temporal to middle cerebral artery bypass is not a universally accepted or popular procedure as compared to coronary bypass, the Anasto Clip system can be helpful for treating certain neurosurgical problems. These include the treatment of difficult blister-like aneurysms, tears of the internal carotid artery, dural tears during spinal surgery, treatment of cerebrospinal fluid rhinorrhea after trans-sphenoidal surgery, and dural repair after skull-based surgery. Titanium AnastoClips, although originally designed as nonpenetrating, have been modified into two forms: one with blunt tips and another with sharpened tips making them in a sense "grippier". A description of the instruments is given followed by examples of unique neurosurgical interventions (Figure 1-4).
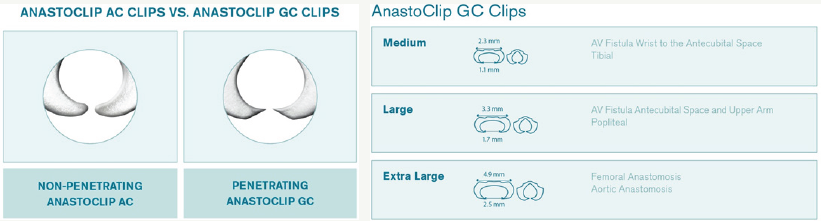
Figure 1: The Dimensions of the AnastoClips and Differences in Clip Tip Sharpness. The gap between clip tips is varied depending upon the thickness of the flanged tissue. The clip forms a flange-closure which is the optimal closure system for vessels under pressure. The clips do not interfere with MR imaging or CT scanning. Problems with clip security after application resulted in a design change in the tip to allow penetration into thick structures such as dural tissue. The non-penetrating clip was developed for fragile microvascular anastomoses. The clip applicators are identical.
AnastoClip Treatment of a Blister Aneurysm
Current neurosurgical literature maintains that an optimal treatment for blister aneurysms of the supraclinoidal internal carotid artery is yet to be defined [1]. Blister-like aneurysms are unusual in that they arise from an unbranched site, have fragile walls, and a broad based neck. The treatment options usually cited are microsurgery, endovascular therapy, or trap ligation with internal carotid sacrifice. There is a report of a successful direct repair of a blister aneurism using the non-penetrating AnastoClips [2]. The author first attempted to close the aneurysm with microsuture, which failed because of back-bleeding. The vessel wall was successfully repaired with the large size 2 mm AnastoClips and the patient made a full recovery. Blister aneurysms still represent a significant surgical challenge. There are no randomized controlled clinical trials, though there are systematic reviews of microsurgical endovascular and combined treatment options [1,3]. There is an excellent article describing the repair of an intraoperative intracavernous carotid tear caused by clinoidectomy during the extradural removal of the anterior clinoid [4]. The base of the intracavernous aneurysm was repaired by titanium AnastoClips (AnastoClip® closure system, 1.4mm, LeMaitre Vascular, Burlington MA) after being torn by a rongeur bite. The senior author Dr. Juha Hernesniemi of the Romani paper has extensive experience dealing with the challenges posed by intracranial aneurysms and concluded that the non-penetrating clips will most likely replace microsutures for intracranial vascular repair complications [4]. The most frequent neurosurgical application of the AnastoClip® was closing the internal and common carotid artery after endoarterectomy before intracranial applications emerged. In 1993, Kirsch reported the first case series for which AnastoClips were used for microvascular anastomosis in cranial base surgery, cavernous sinus repair, internal carotid laceration during vagal nerve neuroganglioma removal, and reconstruction of the P1 segment during basilar tip aneurysm clipping [5]. Blister aneurysms are rare and considered to have very poor prognosis. The AnastoClip offers another therapeutic possibility.
Figure 2: AnastoClip applicators. The pre-loaded applicator system is fired by simple finger compression. Clip application is rapid, reproducible, and facile. Applicators have various neck lengths to suit the operating window. Applicators contain between 25 and 40 clips depending on the size of the AnastoClip System in use.
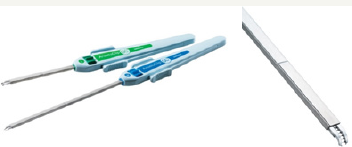
Figure 3: Clip Application, Tissue Eversion and Approximation. It is necessary to evert the tissue to be approximated in the clip-formed flange with an atraumatic everting forceps depicted above remembered with a mnemonic device, "no lips, no clips". The position of the clip applier performing an arteriovenous anastomoses is illustrated.

Figure 4: Clip removal. In the event of a malpositioned or misfired clip, a clip remover should always be available. The device consists of a wedge that widens as the clip is removed.

AnastoClip Treatment for Dural Closure
Figure 5: Dura Closure Using the AnastoClip System. Dural closure is rapidly facilitated by the clips. Dural grafts are necessary and readily applied in the absence of dural approximation. The dura shrinks with drying during craniotomy and a graft is usually necessary to avoid space compromise.
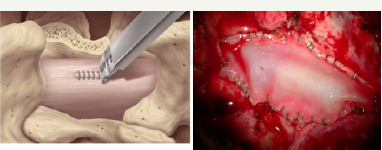
Dural tears are a frequent complication of spine, skull base, and neurotrauma surgery. These dural breaches can be associated with long term problems. Dural closure is particularly vexing in pediatric neurosurgical procedures involving congenital tissue defects. Conventionally sutured duraplasties are complicated by meningoneural adhesions, CSF leakage, as well as infection [6-13]. Duraplasties can be technically difficult because of confined space, quality of the residual dura and the size of the defect. The ideal dural closure should be CSF-tight, avoid meningoneural adhesions or interfere with future radiological imaging. Minengoneural adhesions are often implicated in the pathogenesis in postoperative neural deficits and complicate the event of dural reopening. Since dural repair with needle and suture poses hazards to both the patient and the surgeon, a nonhazardous repair with clips has an advantage. Palm et al. [14] in an experimental study compared clips to suture for dural repair in a relevant animal model and found that clips displayed significantly less extensive acute and chronic inflammation, foreign body reactions and meningoneural adhesions than did with suture. There are been recent reports of clip closure for duratomy repair in emerging orthopaedic and neurosurgical procedures. For example, the minimally invasive transforaminal lumbar body fusion (MIS-TLIF) is performed through a small cannula which restricts the use of needle and suture. The incidence of dural tears in lumbar surgery varies from 1 to 17% and results in poor outcome [15]. The long term outcomes of a dural defect can include pseudomengineoceal, CSF fistula, and nerve root injury. Early closure of the dural leak is necessary to avoid postoperative medical complications that would translate to prolonged bed rest to resolve the CSF leak. The non-penetrating AnastoClip has proven to be an excellent instrument for rapidly and effectively repairing the dura after a tear during the MIS-TLIF procedure [16] (Figure 5).
With skull base surgery, significant dural repair is necessary in all three cranial fossae. Duraplasty can prove to be a technically difficult procedure and present with a significant CSF leak if not successful. The usual repair may have to be obtained by utilizing paracranial tissue flaps in attempts at suturing this or graft material - a difficult procedure. The AnastoClips have recently been reported as a new technique for repair in a cohort of 53 skull based cases [17].
There is a particular need for water-tight dural closures in pediatric spinal surgery. A retrospective review of 27 pediatric cases (26 patients) utilizing application of the AnastoClip system for dural closure discusses unique issues associated with pediatric cases [18]. Authors conclude that the AnastoClip system provides an effective pediatric dural closure with no complications or interference with postoperative imaging. These authors have subsequently reported the use of these clips for dural closure in over 150 cases with technical observations [19]. Studies evaluating the metallic artifacts caused by the AnastoClips in postoperative neuroimaging have concluded that no significant alterations in evaluation quality occurs postoperatively [20]. Comparison of the hydrostatic strength of clipped vs. sutured standard spinal duratomies have been made and established that clips provide a leak-proof far better closure. Clips provided duratomy closure with immediate hydrostatic strength, equivalent to intact dura [21]. Sutured dura leaked and did not have equivalent hydrostatic strength in comparison to the clip method.
There have been isolated reservations regarding dural closure with the AnastoClips. These include laceration of the dura after clip closure, clip slippage off of the dura to become lost in irrigating fluid, and difficulty in removing malposition clips [22]. These authors describe a novel titanium clip for dural closure that resembles an aneurysm clip and applier. There have been no further reports of this applicator or marketing of this device since first described in 1994. There is no question that there is a learning curve for AnastoClip application. Both training and practice in AnastoClip technology are required to accomplish the desired results [23].
Disclosure
Dr. Wolff Kirsch, the inventor of the AnastoClip clip, is a stockholder in the LeMaitre Corporation. Justin Brier-Jones has no financial interest in the LeMaitre Corporation.
References
- Meling TR (2017) What are the treatment options for blister-like aneurysms? Neurosurg Rev 40(4): 587-593.
- Yanagisawa T, Mizoi K, Sugawara T, Suzuki A, Ohta T, et al. (2004) Direct repair of a blister like aneuyrsm on the internal carotid artery with vascular closure staple clips. Technical note. J Neurosurg 100(1): 146-149.
- Regelsberger J, Matschke J, Grzyska U, Ries T, Fiehler J, et al. (2011) Blister-like aneurysms-- a diagnostic and therapeutic challenge. Neurosurg Rev 34(4): 409-416.
- Romani R, Kivisaari R, Celik O, Niemela M, Perra G, et al. (2009) Repair of an alarming intraoperative intracavernous carotid artery tear with anas- toclips: technical case report. Neurosurgery 65(5): E998-E999.
- Kirsch WM, Zhu YH, Hardesty RA, Petti G, Furnas D (1993) Nonpenetrating clips successfully replacing sutures in base of skull surgery. Skull Base Surg 3(4): 171-181.
- Adams CB (1995) "I've torn it: how to repair it”. Br J Neurosurg 9(2): 201-204.
- Aoki N (1988) Acute subdural hematoma during tack-up suture of the dura mater--case report. Neurol Med Chir (Tokyo) 28(10): 994-995.
- Burres KP, FK Conley (1978) Progressive neurological dysfunction secondary to postoperative cervical pseudomeningocele in a C-4 quadriplegic. Case report. J Neurosurg 48(2): 289-291.
- Cohen AR, Aleksic S, Ransohoff J (1989) Inflammatory reaction to synthetic dural substitute. Case report. J Neurosurg 70(4): 633-635.
- Fontana R, Talamonti G, D'Angelo V, Arena O, Monte V, et al. (1992) Spon-taneous haematoma as unusual complication of silastic dural substitute. Report of 2 cases. Acta Neurochir (Wien) 115(1-2): 64-66.
- Jr, R.A., General and micro-operative techniques. , in Neurological Surgery, Y. JR, Editor. 1995, Saunders: Philadelphia. p. 724-766.
- Keener EB (1959) Regeneration of dural defects; a review. J Neurosurg 16(4): 415-423.
- Nash CL Jr, Kaufman B, Frankel VH (1971) Postsurgical meningeal pseudocysts of the lumbar spine. Clin Orthop Relat Res 75: 167-178.
- Palm SJ, Kirsch WM, Zhu YH, Peckham N, Kihara S, et al. (1999) Dural closure with nonpenetrating clips prevents meningoneural adhesions: an experimental study in dogs. Neurosurgery 45(4): 875-881.
- Saxler G, Kramer J, Barden B, Kurt A, Pfortner J, et al. (2005) The longterm clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976) 30(20): 2298-2302.
- Cheng YP, Lin PY, Huang AP, Cheng CY, Chen CM, et al. (2014) Durotomy repair in minimally invasive transforaminal lumbar interbody fusion by nonpenetrating clips. Surg Neurol Int 5: 36.
- Glenn CA, Baker CM, Burks JD, Conner AK, Smitherman AD, et al. (2017) Dural Closure in Confined Spaces of the Skull Base with Nonpenetrating Titanium Clips. Oper Neurosurg (Hagerstown).
- Kaufman BA, Matthews AE, Zwienenberg-Lee M, Lew SM (2010) Spinal dural closure with nonpenetrating titanium clips in pediatric neurosurgery. J Neurosurg Pediatr 6(4): 359-363.
- Lew SM, Matthews AE, Kaufman BA, Zwienenberg M (2016) Letter to the Editor: Nonpenetrating titanium clips for dural closure during spinal surgery. J Neurosurg Spine 24(6): 997-998.
- Ito K, Seguchi T, Nakamura T, Chiba A, Hasegawa T, et al. (2016) Evaluation of Metallic Artifacts Caused by Nonpenetrating Titanium Clips in Postoperative Neuroimaging. World Neurosurg 96: 16-22.
- Faulkner ND, Finn MA, Anderson PA (2012) Hydrostatic comparison of nonpenetrating titanium clips versus conventional suture for repair of spinal durotomies. Spine (Phila Pa 1976) 37(9): E535-E539.
- Levy DI, Sonntag VK (1994) Titanium dural clip testing. Technical note. J Neurosurg 81(6): 947-949.
- Timothy J, Hanna SJ, Furtado N, Shanmuganathan M, Tyagi A, et al. (2007) The use of titanium non-penetrating clips to close the spinal dura. Br J Neurosurg 21(3): 268-271.
© 2018 Wolff Kirsch, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






