- Submissions

Full Text
Surgical Medicine Open Access Journal
Correction of Posttraumatic Valgus Deformity of the Knee by Lateral Open Wedge High Tibial Osteotomy
Greta Ahrens* and Michael Hoffmann
Department of Orthopedic and Trauma Surgery, Asklepios Clinic St. Georg, Germany
*Corresponding author:Greta Ahrens, Department of Orthopedic and Trauma Surgery, Asklepios Clinic St. Georg, Hamburg, Germany
Submission: November 03, 2025;Published: November 14, 2025

ISSN 2578-0379 Volume6 Issue2
Abstract
A 33-year-old male patient presented with lateral knee pain due to a posttraumatic valgus deformity. He had sustained femoral and tibial plateau fractures 25 years ago, treated with osteosynthesis. Subsequently, a valgus deformity with limb shortening developed. Clinical examination showed a limping gait, genu valgum and recurvatum with full range of motion, stable collateral ligaments and a positive Lachman test. MRI revealed grade II chondromalacia in the lateral compartment. A lateral open wedge high tibial osteotomy (HTO) was indicated for correction of limb axis and length, along with repositioning of the proximal tibiofibular joint. The postoperative course was uneventful with improved alignment and stable fixation. A second-stage slope correction is planned after bony consolidation in six months.
Keywords:Valgus deformity; High tibial osteotomy; Arciero technique; Posterolateral corner; Tibiofibular joint reconstruction
Abbreviations:HTO: High Tibial Osteotomy; LCL: Lateral Collateral Ligament; MRI: Magnetic Resonance Imaging
Introduction
Posttraumatic deformities of the lower extremity, particularly valgus malalignments, can lead to chronic pain, altered gait mechanics and premature joint degeneration [1]. Corrective osteotomies, such as high tibial osteotomy (HTO), allow restoration of mechanical alignment and optimization of joint load distribution [2]. This case report describes the surgical management of a severe posttraumatic valgus deformity using a lateral open wedge HTO combined with posterolateral corner reconstruction.
Case Presentation
A 33-year-old male presented with lateral knee pain and gait disturbance. He had sustained femoral and tibial plateau fractures on the right side 25 years ago due to a motor vehicle accident, which were treated by osteosynthesis. Clinical evaluation revealed a valgus deformity and limb shortening. Examination showed a limping gait, genu valgum and recurvatum with full range of motion. Ligamentous stability was preserved except for a positive Lachman test. MRI confirmed grade II chondromalacia in the lateral compartment. The patient worked in a physically demanding job as a warehouseman and had no comorbidities (Figure 1).
Figure 1:A) Preoperative analysis revealed a valgus axis of 21°, a mechanical medial proximal tibial angle (mMPTA)
of 108° and a mechanical lateral distal femoral angle (mLDFA) of 89°.
B) A varus correction of 16° via lateral open wedge HTO was planned, resulting in a postoperative mMPTA of 91°
and a JLCA of 1°.

Operative Procedure
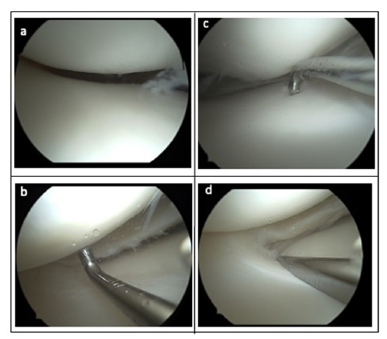
With the patient in a supine position and the right leg placed in an electric leg holder, a diagnostic arthroscopy was first performed. Arthroscopy confirmed grade II chondromalacia in the lateral compartment, with no additional intra-articular pathologies identified (Figure 2).
Figure 2:Diagnostic Arthroscopy.
A. Intact patellofemoral joint surface without signs of chondropathy; normal patellar tracking within the trochlear
groove.
B. Lateral compartment showing grade II chondropathy on probe examination.
C. Medial compartment with regular cartilage surface.
D. Mild fraying of the lateral meniscus in the lateral compartment without evidence of a tear.
Fluoroscopic examination revealed a valgus contracture of the knee associated with shortening of the lateral collateral ligament (LCL) and posterolateral corner (PLC).
A lateral approach to the knee joint was utilized. After skin incision and neurolysis of the common peroneal nerve, the iliotibial tract was incised and detached from the Gerdy’s tubercle. A tenotomy of the markedly shortened and scarred LCL was then performed. The proximal tibiofibular joint was carefully exposed and the interosseous membrane was released while preserving the anterior tibial artery.
Following height marking under fluoroscopic control, an infratuberositary lateral open wedge high tibial osteotomy was executed. The osteotomy was stabilized using a locking plate and the osteotomy gap was filled with allogenic cancellous bone graft (Figure 3).
Figure 3:Intraoperative Fluoroscopic Images. a) Osteotomy height marking using two parallel inserted Kirschner wires (2.0 mm diameter). b) Osteotomy result with the fixation plate in situ. c) Marking for the Arciero reconstruction using Kirschner wires to identify the popliteal sulcus and the lateral femoral epicondyle; the implanted TightRope for stabilization of the proximal tibiofibular joint is also visible. d) Marking of the drill canal through the proximal fibula for the Arciero reconstruction using a targeting device.
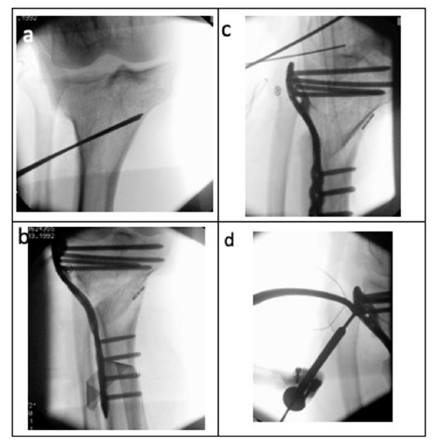
After correction, anatomical realignment of the previously proximalized fibular head within the tibiofibular joint was achieved. The proximal tibiofibular joint was stabilized using a syndesmotic TightRope fixation.
Subsequently, an Arciero-type reconstruction of the posterolateral corner was performed using a peroneus longus tendon graft and a neo-capsule was created using a second peroneus longus graft. The Arciero reconstruction followed standard technique [3,4]: Fixation of the popliteus tendon graft using a SwiveLock anchor within the popliteal sulcus and fixation of the LCL limb with an interference screw. The neo-capsule was secured to the dorsolateral tibial plateau using an additional SwiveLock anchor (Figure 4).
Final intraoperative fluoroscopic imaging confirmed correct implant placement and satisfactory osteotomy alignment (Figure 5).
Figure 4:Intraoperative Findings. a) Positioning of the leg in an electric leg holder with an applied tourniquet. The valgus limb alignment with intact soft tissues is visible. b) Lateral view after positioning of the leg, demonstrating the genu recurvatum deformity. c) Lateral approach to the tibial head; the finger indicates the proximal tibiofibular joint after mobilization. The common peroneal nerve is looped with a blue vessel loop. d) Status post insertion of the fixation plate following lateral varus-producing HTO. The forceps indicate the Arciero reconstruction and the created “neo-capsule.”
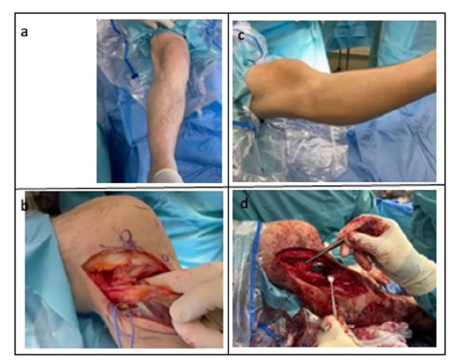
Figure 5:Postoperative Radiographic Evaluation. a. Lateral radiograph demonstrating plate osteosynthesis of the proximal tibia and TightRope fixation of the proximal tibiofibular joint. b. Anteroposterior postoperative radiograph showing the same plate osteosynthesis and TightRope fixation in situ.

Postoperative Management
A. Partial weight-bearing for 6 weeks
B. Range of motion restriction: 0–0–0 for 2 weeks, followed
by 0–0–60° for 4 weeks
C. Vitamin D supplementation
D. Thromboprophylaxis according to current clinical
guidelines
Postoperative Outcome
Following the osteotomy, a significant improvement in the mechanical limb axis was achieved. Proper anatomical repositioning of the proximal fibula within the tibiofibular joint was verified. During the inpatient stay, the patient was able to mobilize independently using forearm crutches. A full-length standing radiograph is scheduled for postoperative outpatient follow-up.
Due to the anticipated risk of delayed bone healing, an initial block correction was performed in the anteroposterior plane. A secondary slope correction is planned after radiographic evidence of bony consolidation in approximately six months.
Discussion
Posttraumatic valgus deformities are challenging to correct, especially when associated with soft-tissue contractures and posterolateral instability. A lateral open wedge HTO allows precise axis correction with length restoration. In line with the findings of Nuelle et al., precise correction of mechanical alignment and control of the posterior tibial slope are essential to achieve optimal long-term results following lateral open-wedge high tibial osteotomy. Their work supports the importance of individualized planning and careful slope adjustment in preventing recurrence of valgus deformity and maintaining joint function over time [5]. The combination with an Arciero-type reconstruction provides stability to the posterolateral complex, addressing both bony and ligamentous deficiencies. Kiliçli and Taşkiran report a rare but severe complication following open-wedge high tibial osteotomythe development of a progressive secondary deformity. They emphasize that such cases highlight the importance of accurate intraoperative correction, stable fixation and careful postoperative monitoring. Inadequate fixation, technical error, or premature weight-bearing may lead to loss of correction, nonunion and secondary deformity [6]. The authors stress that regular radiographic follow-up and early recognition of alignment changes are crucial to prevent further deterioration and to allow timely revision or slope correction.
This case demonstrates a successful single-stage correction with promising early postoperative results and no documented secondary deformity. Further follow-up will assess long-term outcomes after completion of the planned slope correction.
Conclusion
The presented case highlights the successful correction of a severe posttraumatic valgus deformity of the knee using a lateral open-wedge high tibial osteotomy combined with posterolateral corner reconstruction. This approach allowed restoration of the mechanical axis, limb length and stability of the proximal tibiofibular joint, resulting in improved alignment and early functional recovery.
Accurate preoperative planning, meticulous intraoperative execution and stable fixation are key to achieving favorable outcomes and preventing complications such as secondary deformity or loss of correction, as emphasized in recent reports. Regular postoperative follow-up and staged correction of the posterior tibial slope are essential to ensure long-term joint preservation and optimal function. This case underscores the importance of an individualized, stepwise treatment strategy that addresses both osseous and soft-tissue components in complex posttraumatic knee deformities.
Acknowledgements
We thank the surgical and nursing teams of Asklepios Klinik St. Georg for their assistance in patient care and intraoperative support.
Conflict of Interest
The authors declare no conflict of interest.
References
- Visscher LE, McCarthy C, White J, Tetsworth K (2024) Asymmetric post-traumatic knee arthritis is closely correlated with both severity and time for lower limb coronal plane malalignment. Cartilage 1;15(2): 100-109.
- Liu X, Chen Z, Gao Y, Zhang J, Jin Z, et al. (2019) High tibial osteotomy: Review of techniques and biomechanics. J Health Eng 2: 8363128.
- Grimm NL, Levy BJ, Jimenez AE, Bell R, Arciero RA, et al. (2020) Open anatomic reconstruction of the posterolateral Corner: The arciero technique. Arthrosc Tech 9(9): e1409-e1414.
- Coppola C, Sigloch M, Hoermann R, Schlumberger M, Schuster P, et al. (2025) Posterolateral knee ligament reconstruction using the arciero technique provides greater rotational stability than the modified larson technique: A biomechanical study. American Journal of Sports Medicine 53(1): 147-153.
- Nuelle CW, Albuquerque JBD, Kfuri M (2024) Knee valgus deformity: Indications and outcomes for a high tibial medial closing-wedge osteotomy. Journal of Cartilage and Joint Preservation 4(4): 100212.
- Kiliçli B, Taşkiran E (2024) A rare complication: Severe valgus deformity after open-wedge high tibial osteotomy. J Orthop Case Rep 14(4): 84-89.
© 2025 Greta Ahrens. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






