- Submissions

Full Text
Surgical Medicine Open Access Journal
Comparative Study of Different Planes of Dissection in Abdominoplasty
Ahmed M Abdel Modaber1*, Vusal Aliyev
1Genera! Surgery Department, Faculty of Medicine, Mansoura University
2General Surgery Department, Emsey Hospital, Istanbul, Turke
*Corresponding author: Ahmed M Abdel Modaber, General Surgery Department, Faculty of Medicine, Mansoura University, Egypt
Submission: November 06, 2017; Published: January 03, 2018

ISSN: 2578-0379Volume1 Issue2
Abstract
Background: In abdominoplasty, violation of deep lymphatics that run just superficial to the abdominal wall muscular fascia is thought to further compromise lymphatic drainage of the serous fluid produced at the surface of undermined tissue. The potential role for preserving Scarp's fascia and/or the deep fat compartment during abodminoplasty is to decrease complication rate especially seroma.
Patients and Methods: Between August 2010 to February, 45 patients were submitted to full abdominoplasty. These patients were divided into groups (according to the plane of dissection in infra-umbilical region): 15 patients of supra-fascial plane (Group I), 15 patients of subscarpal plane (Group II) and 15 patients of suprascarpal plane (Group III). Post-operative assessment was done six months through which clinical examination for postoperative complications, patient satisfaction and flap thickness via superficial abdominal U/S will be mentioned.
Results: There is a higher mean duration till drain removal in group I (7.6 days) compared to (4.8 days) in group II and (3.4 days) in group III. That's why 20% of patients of group I developed seroma. There is higher mean flap thickness after 2 weeks and until 3 months of surgery in group compared to other groups. While there is no significant difference between the three groups after 6 months. There is higher grade of satisfaction among cases in group II and group III compared to group I.
Conclusion: The superficial group of patients wasn't pleased by long hospital stay and downtime, prolonged edema formation, prolonged duration till drain removal and supra epigastric higher leveling compared to the infraumbilical level. In contrary of that, the subscarpal and suprascarpal groups of patients gave more satisfactory results.
Keywords: Abdominoplasty; Seroma; Abdominal wall flap edema; Abdominal wall lymphatics; Scarpa's fascia
Introduction
The evolution of techniques in abdominoplasty had always motivated surgeons to reach for a lesser postoperative morbidity and lower complications rates [1].
Lockwood [2] reported the high lateral tension abdominoplasty, in which he used the Scarpa fascia to decrease the tension of the skin closure.
Since the 1990s, the undermining has decreased in amplitude until 2001, where Saldanha standardized a selective undermining along the internal borders of the rectus muscles, corresponding to 30 percent of the traditional undermining, thus preserving the abdominal perforating vessels [3].
This selective undermining is maintained to this day [4]; through using a modified high-lateral-tension technique with a standard plane of elevation immediately above the abdominal wall muscular fascia for development of the abdominal skin flap [5].
The anatomy and physiology of lymphatic vessels in the abdominal wall have been described to be an important factor in the status of abdominal wall following abdominal lipectomy [6].
Violation of the deep lymphatic vessels that run just superficial to the abdominal wall muscular fascia is thought to further compromise lymphatic drainage of the serous fluid produced at the surface of the undermined tissue [7].
Fang et al. [8] have added one technical modification to flap elevation where dissection (infra-umbilical) in a more superficial plane, just below the Scarpa fascia in thin patients. In patients with thicker adipose tissue, a loose areolar tissue and a thin layer of deep fat should be preserved to avoid disturbing the major lymphatic vessels against abdominal wall.
Abu-Hijleh et al. [9] described two different fat compartments separated by fascial plane known as Scarpa's fascia or superficial fascia.
Accordingly, Costa-Ferreira et al. [10] proposed a different approach from the classical technique of abdominoplasty by suggesting that the abdominal flap should be elevated on two different surgical planes, in the supra-umbilical region a pre- muscular plane as in traditional abdominoplasty, in the infra umbilical region a supra-scarpa's (pre-scarpa's) fascia plane.
The potential role for preserving Scarpa's fascia and/or the deep fat compartment during abdominoplasty has been pointed out by Espinosa-de-los Monteros et al. [11] as a way to lower complication rate e.g. decrease in seroma formation, decrease in abdominal necrosis, decrease in the swelling of the lower abdominal flap and avoidance of discrepancy in flap thickness (between the pubic flap and the abdominoplasty flap).
In this paper, we are going to compare between the different procedures in high lateral tension with flap elevation abdominoplasty from the point of the plane of dissection, the incidence of early and late complications, patient and surgical panel satisfaction.
Patients and Methods
This study was performed on 45 patients submitted to full abdominoplasty with umbilical transposition using the high lateral tension with flap elevation technique.
These patients were divided into groups (according to the plane of dissection in infra-umbilical region):
Group A - 15 patients who underwent abdominoplasty with flap elevation suprafascial.
Group B - 15 patients who underwent a similar type of abdominoplasty but through subscarpal plane of dissection.
Group C - 15 patients also underwent a similar type of abdominoplasty except for the preservation of Scarpa's fascia.
Inclusion criteria
o All patients are females.
o Age range between 25 years and 45 years.
o These presented with abdominal deformities marked by excess abdominal skin and adipose tissue with muscle laxity (Matarasso type III and IV) and (Toledo type IV and V).
o Body mass index (BMI) less than 35.
Exclusion criteria
o Chronic medical diseases (e.g. bleeding tendency, hepatic, renal, cardiac diseases and diabetes).
o Local abdominal wall diseases (including ventral hernias).
o Redo abdominoplasty.
o Regular drug intake (especially asprin, NSAIDs and anticoagulants).
o Alcohol consumption.
o BMI more than 35.
o Psychological disturbed patients.
Methods
After taking written informed consent all patients were subjected to:
o Full history taking (specially, medical history and drug intake).
o Thorough clinical examination and targeted examination to evaluate the abdominal wall deformity.
o Routine laboratory tests (CBC, liver functions, renal functions, coagulation profile and RBS).
o Preoperative imaging studies (abdomino-pelvic U/S).
o Preoperative broad spectrum intravenous antibiotics (3rd generation cephalosporin) were routinely administrated to all patients.
Preoperative markings
We marked the abdomen in the shape of "Bicycle handle bar", with upper (supraumbilical) horizontal line (18-19cm) then runs obliquely via traction of lateral abdominal wall medially to meet the line which runs in the lower abdominal crease as it also continuation of a lower horizontal line (14cm), the distance from the superior vulval commisure to the lower horizontal marking was 6 to 7cm (Figure 1).
Figure 1: Skin markings showing the abdominal midline extending from xiphoid process to the superior vulval commisure.

Surgical procedure Below the umbilicus
In group I was dissected in a suprafascial dissection immediately above the abdominal muscular wall (Figure 2).
In group II a modified plane of dissection deep to the Scarpa’s fascia (subscarpal) leaving a layer of areolar and adipose tissue just superficial to the muscular fascia (Figure 3).
Figure 2: The incision was made on the line drawn and deepened through the subcutaneous tissue to the underlying abdominal wall. Suprafascial Dissection was performed superiorly to the level of the umbilicus with electrocautery.
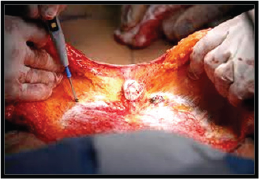
Figure 3: Subscarpal plane of dissection.
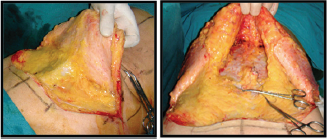
In group II a modified plane of dissection deep to the Scarpa’s fascia (subscarpal) leaving a layer of areolar and adipose tissue just superficial to the muscular fascia (Figure 3).
Figure 4: Suprascarpal plane of dissection.

The umbilicus was incised vertically and scissor dissection is performed down to the abdominal wall leaving some subcutaneous fat on the umbilical stalk to maintain vascularity. The abdominal flap was split anticipating its complete removal.
Above the umbilicus
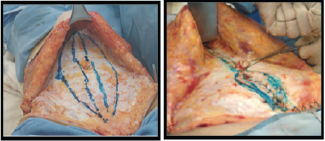
In the three groups all were dissected in a preaponerotic (premuscular) plane. The tunnel in median line of upper abdomen was undermined between the outer borders of the rectus abdominal muscles to allow a standard rectus sheath plication. The medial borders of the rectus sheath were marked with methylene blue, delineating the diastasis recti. The proposed lateral edge of the rectus sheath plication was also marked with methylene blue. The myofascial plication was performed with number 1/0 proline run from the xiphoid to just above umbilicus. Plication was resumed at the inferior angle of the umbilicus down to the level of the pubic symphysis (Figure 5).
Figure 5: The plication begins at the xiphoid and runs continuously to the symphysis pubis.
The table was flexed appropriately to reduce the tension on closure. The excess tissue was resected and temporary midline staple was placed to facilitate identification of the new umbilical location. A small vertical ellipse was drawn and excised.
Umbilicoplasty was performed using simple vertical slit technique. Umbilicus was closed by subcuticular suturing (4/0 monocryl) to minimize any visible scarring. The drain was laid across lower abdomen and brought out through the skin inferior to the incision on both sides and secured with silk suture (Figure 6).
Figure 6:The drain was laid across lower abdomen and brought out through the skin inferior to the incision on both sides and secured with silk suture.

Final skin closure was performed with interrupted subcutaneous Vicryl 2/0 & 3/0 then subcuticular Monocryl 3/0. Pressure garments were applied at the end of the operation.
Postoperative care
o The patients were motivated to ambulate on the 1st postoperative day and compression garments were used for at least 6 weeks after surgery.
o Patients were instructed to avoid strenuous activity for a full 6 weeks postoperatively.
o Patients were instructed to record drain outputs daily, and the first postoperative visit was scheduled within 1 week after surgery.
o The drain will be removed when it meats the criteria for removal (drain output equal or less than 30 cc/day).
o Postoperative assessment was done six months through which clinical examination for postoperative complications and patient satisfaction will be mentioned (contour, drain removal time, pain and scar).
o Photography: the same as preoperative photos.
This achieved through applied superficial abdominal US for all patient in the postoperative period (2 weeks, 1.5,3,6 months after the operation).
Outcome measures
Baseline characteristics, including age, weight, height, BMI and Matarasso type of abdomen were recorded for the three groups of patients.
The outcomes measured in this study included the incidence of seroma (clinical and US), resolution of edema (clinical and US), the amount and duration of closed-suction drainage, the amount of liposuction, patient satisfaction, the long lasting results and the incidence of other complications.
Statistical analysis
The data was collected, coded and entered to a personal computer (P.C.) IBM compatible 2.6 GHZ. The data was analyzed with the program (SPSS) statistical package for social science under windows version 11.0.1.
The statistical tests used in this thesis are: student t test, one way Analysis Of Variance (ANOVA) and Chi-square test. p value < 0.05 was considered to be statistically significant.
Results
Table 1: Comparison between the three studied groups as regards the mean age.
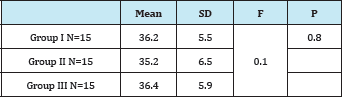
Group I Suprafascial Group II Subscarpal Group III Suprascarpal P>0.05 not significant.
Table 1 shows that, there is no significant difference statistically between the three studied groups as regards the mean age.
Table 2 shows that, there is no significant difference statistically between the three studied groups as regards the mean body mass index.
Table 2: Comparison between the three studied groups as regards the mean body mass index.
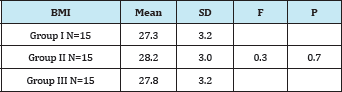
Group I Suprafascial Group II Subscarpal Group III Suprascarpal P>0.05 not significant.
There is a higher mean liposuction in group II and group III compared to group I but the difference is not significant statistically (Table 3).
Table 3: Comparison between the three studied groups as regards the mean liposuction.
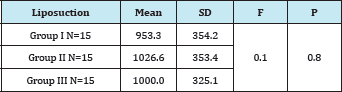
Group I Suprafascial Group II Subscarpal Group III Suprascarpal P>0.05 not significant.
There is a lower mean duration of operation in group I compared to group II and group III and the difference is highly significant statistically (Table 4).
Table 4: Comparison between the three studied groups as regards the mean Operative time in hours.
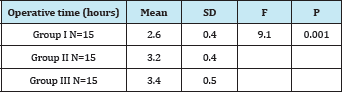
Group I Suprafascial Group II Subscarpal Group III Suprascarpal P<0.01 highly significant.
LSD test shows significant difference between Group I vs. group II, Group III.
There is a higher mean duration till drain removal in group I 7.6 days compared to 4.8 days in group II and 3.4 days in group III and the difference is highly significant statistically (Table 5).
Table 5: Comparison between the three studied groups as regards the mean time till drain removal in days.
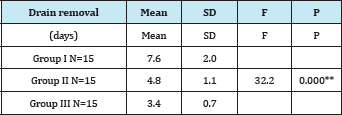
Group I Suprafascial Group II Subscarpal Group III Suprascarpal P<0.01 highly significant.
LSD test shows significant difference between Group I vs. II, III Group II vs. III.
Higher mean operative time in obese subjects compared to normal subjects and the difference is highly significant statistically. Higher mean time till drain removal in obese subjects 9.5 days compared to 6.4 days among normal subjects and the difference is highly significant statistically (Table 6).
Table 6: Comparison between obese and normal subjects in group I as regards the time till drain removal and operative time.
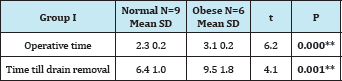
P<0.01 highly significant.
There is no significant difference statistically between obese and normal subjects in group II as regards operative time. There is a higher mean time till removal of drain in obese subjects compared to normal subjects in group II and the difference is highly significant statistically (Table 7).
Table 7: Comparison between obese and normal subjects in group II as regards the time till drain removal and operative time.
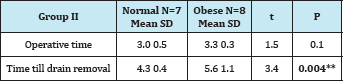
P<0.01 highly significant.
There is a higher mean operative time in obese compared to normal subjects and the difference is highly significant statistically. There is a higher mean time till removal of drain in obese subjects compared to normal subjects in group III and the difference is highly significant statistically (Table 8).
Table 8: Comparison between obese and normal subjects in group III as regards the time till drain removal and operative time.
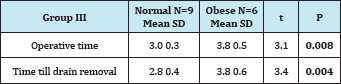
P<0.01 highly significant.
Table 9: Comparison between the three studied groups as regards Seroma Formation.
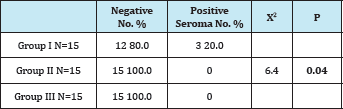
P<0.01 highly significant.
Table 9 shows that, there is a higher percentage of seroma formation among cases in group I 20 % compared to 0% among group II and 0% among group III and the difference is significant statistically.
There is a higher percentage of seroma formation 50% among obese subjects in group I compared to 0% among normal subjects and the difference is significant statistically (Table 10).
Table 10: Comparison between obese and normal subjects in group I as regards seroma formation.
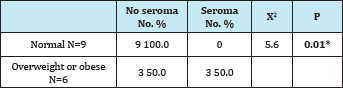
Group I Suprafascial
Overweight or obese above 29 BMI
*P<0.05 significant.
Table 11: Comparison between the three studied groups as regards patient late assessment of the operation (6 months follow up).
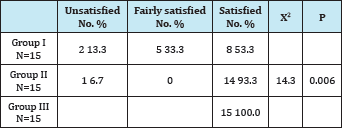
Group I Suprafascial Group II Subscarpal Group III Suprascarpal
P<0.01 highly significant.
Table 11 shows a higher grade of satisfaction among cases in group II and group III compared to group I and the difference is highly significant statistically.
Lower level of satisfaction in group I, 13.3% were totally dissatisfied and 33.3% were fairly satisfied and the difference is highly significant statistically.
Table 12: Comparison between the three studied groups as regards surgical panel assessment of the operation after 6 months
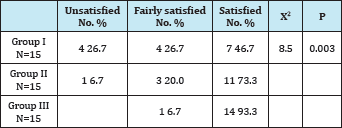
Group I Suprafascial Group II Subscarpal Group III Suprascarpal
P<0.01 Highly Significant.
Table 12 shows a higher rate of dissatisfaction among surgical panel for outcome of surgery in group I 26.7% compared to 6.7% for group II and 0% for group III and the difference is highly significant statistically. A higher rate of satisfaction of the surgical panel for outcome of patients in group III 93.3% compared to 73.3% in group II and 46.7% in group I and the difference is highly significant statistically.
There is a higher rate of dissatisfaction of the operation results in obese patients compared to normal subjects 33.3% complete dissatisfaction compared to 0% in normal subjects, 50% rate of fair satisfaction compared to 0% among normal subjects and the difference is highly significant statistically (Table 13).
Table 13: Comparison between obese and normal subjects in group I as regards patient early assessment of the operation 3 months.
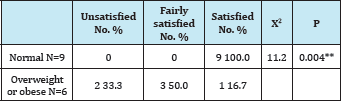
Group I Suprafascial
Overweight or obese above 29 BMI
P<0.01 Highly Significant
There is a higher rate of dissatisfaction of the operation results after 6 months in obese patients compared to normal subjects 66.7 % complete dissatisfaction compared to 0% in normal subjects, 33.3% rate of fair satisfaction compared to 22.2% among normal subjects and the difference is highly significant statistically (Table 14).
Table 14: Comparison between obese and normal subjects in group I as regards patient late assessment of the operation 6 months.
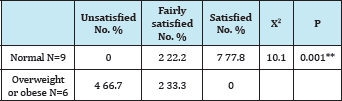
Group I Suprafascial Overweight or obese above 29 BMI
P<0.01 Highly Significant
There is a higher rate of dissatisfaction of the operation among the surgical panel after 6 months in obese patients 66.7% complete dissatisfaction compared to 0% in normal subjects, 33.3% rate of fair satisfaction compared to 22.2% among normal subjects and the difference is highly significant statistically (Table 15).
Table 15: Comparison between obese and normal subjects in group I as regards surgical panel assessment of the operation after 6 months.
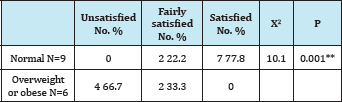
Group I Suprafascial Overweight or obese above 29 BMI
P<0.01 Highly Significant
Discussion
Abdominoplasty is among the most popular procedures in esthetic surgery generating high levels of patient satisfaction. There are three layers should be identified in the subcutaneous tissue of the abdomen: a superficial adipose layer (SAT), a membranous layer, and a deep adipose layer (DAT). The term “superficial fascia” should only be used as a synonym for the membranous layer, and all other eponyms for it should be abandoned [12].
Despite the good results obtained with a full abdominoplasty, significant complications and secondary surgical revision rates are still reported. Multiple surgical strategies have been described to lower the complication rate, such as lipoabdominoplasty, selective undermining, internal fixation techniques, and avoidance of electrocautery, use of pressure dressings, and use of fibrin glue. The fact is that overall complication rates as high as 30 percent have been recently reported. Seroma alone is still reported with frequencies as high as 30 percent [10].
The most frequent complication following an abdominoplasty procedure remains the occurrence of seromas. Although seromas usually resolve uneventfully with multiple aspirations, some can often become frustrating in their persistence and can lead to the development of a pseudocyst or pseudobursa. Progression to this chronic state generally requires reoperation for successful management [8].
The exact pathogenesis of postabdominoplasty seromas remains unclear. Elevation of the skin flap necessarily results in a large elevated surface area that produces serous fluid secondary to the inflammatory stimulus of injury. Both the process of flap elevation and redundant skin resection also disrupt lymphatic vessels, resulting in a compromised state of lymphatic drainage in the immediate postoperative period. In addition, the presence of any dead space promotes the formation of acute fluid collections [8].
Robert et al. [13] mentioned that Patients should be counseled regarding an increased risk of seroma formation following abdominoplasty when combined with liposuction of the flanks. In addition, patients who are overweight are at increased risk for developing a postoperative seroma compared with patients with normal body mass indices.
It seems possible that reducing the rate of seroma after abdominoplasties may be achieved by increasing the duration of postoperative immobilization up to 48 hours. It is recommended that immobilization for 48 hours after abdominoplasty, together with the administration of low molecular weight heparin and compression stockings. Alternatives for the prevention of shearing forces and thus the prevention of seroma, such as special compression garments or limited activities after mobilization, are not evidence-based [14].
In our experience, liposuction can be a safe and effective adjunct when per-formed conservatively across the anterior abdominal wall and when excessive undermining is not performed.
Lipoabdominoplasty is based on the selective undermining of the abdominal flap on the superior medial line, preserving the great majority of the arteries, lymphatic vessels, veins, and nerves, which reduces the incidence of complications [5].
Previous anatomical and imaging studies described two different fat compartments in the lower abdominal wall: a superficial compartment and a deep compartment separated by a fascial plane known as the Scarpa fascia or superficial fascia [10].
Moore et al. [15] mentioned that most superficial lymphatic vessels superior to the umbilicus drain to the axillary lymph nodes; a few drain medially and deeply to the parasternal and anterior diaphragmatic lymph nodes. Superficial lymphatic vessels inferior to the umbilicus drain to the superficial inguinal lymph nodes.
It was found that the lymphatic vessels below the umbilicus were superficial to the scarpa fascia layer and drain to the inguinal region. While those above the umbilicus was drained towards the rectus in the premuscular plane accompanying the perforators and not directing to the axilla [16].
In the unresected abdomen, the supraumbilical flap drains its lymphatic superiorly in the axilla and the infraumbilical flap drains into the inguinal region. After flap resection, the only remaining tissue is the supraumbilical flap, which still drains in the axilla. At this point, the lymphatic of the subscarpal fat are disconnected from the tissues they originally drained, the infraumbilical resected flap, and thus are not likely to contribute to the drainage of the resected tissues. It is possible that these potentially intact subscarpal lymphatic would simply pick up any free fluid produced in the wound, thus reducing the risk of seroma [16].
We believed this was a flawed assumption because Lymphatic clear fluid through intact lymphatic vessels that, when injured by surgery, lead to the universally encountered postoperative swelling, anywhere in the body. Swelling subsides when these lymphatic vessels are reconstituted, a process that takes weeks to months to occur [16].
In this study 45 cases had done abdominoplasty (high lateral tension with flap elevation technique). 15 cases had done suprafascial plane of dissection in the infraumbilical region. While 15 cases had done subscarpal plane of dissection in the infraumbilical region. The rest 15 cases had done suprascarpal plane of dissection in the same region.
The aim of our study is to compare different plane of dissection in abdominoplasty from the point of outcome, early and late complication and patient and surgical panel satisfaction.
According to our results, there is marked lower mean duration of operation in suprafascial plane of dissection compared to other planes of dissection, as technically it is the easiest plane to find and to be dissected.
Moreover, patients of suprafascial dissection have significantly highest mean duration till drain removal. It was clear that duration was profound in obese patient. That's why seroma formation still recorded only when dissection was suprafascially.
We noticed that abdominal wall flap thickness (detected by superficial abdominal US) in suprafascial dissection have the thickest measurements (indicating sever edema) among other planes of dissection throughout the first 3 months postoperatively. While it records the least thickness when measured at the 6th months postoperatively (indicating edema subsided). Exactly At this point, there were comments from patients especially obese patients who underwent suprafascial dissection because of abdominal wall flap and mons pubis discrepancy (infraumbilical region showed scaphoid nature); that brought patient to show higher rate of late dissatisfaction.
On the other hand, we observed that in the subscarpal and suprascarpal planes of dissection gave more satisfactory results in the patients who were younger in age, non smoker, and no alcohol consumption, lower BMI than 30, didn't have any chronic medical conditions. Surprisingly, these patients didn't show any morbidity in there abdominoplasty, with the benefits of decreased down time, shorter hospital stay, faster return to work, rapid resolution of edema, earlier removal of drain and in some patients we were motivated not to put any drain intraoperatively.
We noticed that, the higher the amount of liposuction, the higher the incidence of seroma and prolonged edema especially in suprafascial and subscarpal planes of dissection, but this wasn't significant statistically.
It was clear that subscarpal and suprascarpal planes of dissection showed marked higher mean duration of operation when compared against suprafascial dissection that because of reasons e.g. sophisticated plane of dissection, more effort exerts in heamostasis, difficulty in obtaining symmetrical level on both sides in the same plane of dissection.
Whereas the mean duration till drain removal experienced a significant drop among patients of subscarpal dissection and extremely dropped in patients of suprascarpal dissection when we compared them against suprafascialy dissected patients. As we said before, this was encouraging us to perform an extra cases with both subscarpal and suprascarpal techniques (in patients with their BMI are less than 30) but without drain insertion anymore. The results came very potential as there wasn't any patients has been developed any complications. But this needs further research works.
The abdominal wall flap thickness (detected by superficial abdominal US) in subscarpal and suprascarpal dissection showed marked lower thickness (indicating lower edema) during first 3 months postoperatively (especially suprascarpal patients) when compared to suprafascial dissection. Strangely, the records up sided down at the 6th month postoperatively (indicating edema subsided) as both subscarpal and suprascarpal patients showed thicker flap thickness than suprafascial patients. That was because of the scarpa’s fascia and infrascarpal fat that has been left under the flap where it gives the infraumbilical bulge; this was approved from the patients as it gives natural smoothness along with mons pubis curve, leading to extreme affection to the late patient satisfaction.
This infraumbilical bulge was slightly higher in obese patients; that brings us to add a technical modification when performing suprascarpal plane of dissection in the form of either liposucted this bulge at the end of the operation, or meticulous some surgical excision of infrascarpal fat during rectal muscle plication.
From the data supplied from the patients, we noticed that they in the first three months postoperatively were very pleased by short hospital stay and downtime, earlier return to work, faster body reshaping and contouring in the suprascarpal plane of dissection and to lesser extend in the subscarpal plane. In addition to that, they were satisfied by the slightly elevated infraumbilical bulge that was elicited after six months from the operation.
In contrary of that, the patient of suprafascial plane of dissection were not pleased by the long hospital stay and downtime, later return to normal daily activity, prolonged duration till drain removal that sometimes reached up to twelve days, prolonged edema formation as it took up to six months recovery time and especially in patients that developed seroma where needed repeated needle aspiration till complete resolution. After six months some patients showed dissatisfaction of supraepigastric leveling compared to the infraumbilical level; it was higher in the epigastric area. This was due to decreased flap thickness in the infraumbilical area. After presenting the digital photos to the panel, they recommended further liposuction in the epigastric area.
Superficial system of lymphatic structures within the superficial fat and a deep system of lymphatic vessels along the muscular fascia, typically situated near perforators. Preservation of a thin layer of deep adipose tissue along the muscular fascia not only minimized injury to these lymphatic vessels but also maintained a bed of well- vascularized tissue as the foundation for the skin flap [8].
This subscarpal dissection plane appeared to be equally effective in allowing earlier drain removal as a more superficial dissection plane cause significant decrease in the postoperative drain amount, this trend toward a decrease seroma formation. No complaints regarding the contour of the abdominal wall with respect to the lymphatic-preserving technique [8].
Al Aly [17] declared that in his experience, elevating the abdominal flap at a more superficial level. (Not always maintain Scarpa fascia intact, but elevate at or just below it) seems to reduce our seroma rate. However, this is an empirical impression not yet verified by hard scientific data. Although the reduced drain output and time to drain removal have some benefit, these improvements have limited value in clinical practice, especially in the United States, where patients are not kept in the hospital until their drains are removed.
Al Aly [17] mentioned that leaving behind the lymphatic vessels in the subscarpal fat leads to better lymphatic clearance and thus a reduction in collected fluid. This mechanism, which he called "lymphatic preservation" he did not believe that it is logical.
Costa-Ferreira et al. [10] proposed a different approach from the classic technique of abdominoplasty by suggesting that the abdominal flap should be elevated on two different surgical planes: in the supraumbilical region, a premuscular plane as in a traditional abdominoplasty; and in the infraumbilical region, a pre-Scarpa fascia plane. The goal of the surgical modification proposed by Le Louarn, Va'sconez and de la Torre, and Saldanha et al. was to decrease complications (i.e. seroma).
Several possible reasons for preservation of the Scarpa fascia may include decrease in seroma formation, decrease in abdominal necrosis, allowance for safer liposuction at the same time as limited abdominoplasty, decrease in swelling of the lower abdominal flap, and avoidance of discrepancy in flap thickness (between the pubic flap and the abdominoplasty flap). Scarpa fascia preservation on the infraumbilical area better respects the physiology of the abdominal wall, as it also implies the preservation of the deep fatty layer along with its connective tissue, lymphatic vessels, arteries, and veins [10].
Another possible explanation for this result is better tissue healing and adhesion. This can be the result of two healing surfaces with better vascularization than the ones that are opposed after a traditional abdominoplasty, which is known to produce a profound devascularization of the abdominal wall [10].
Preservation of the Scarpa fascia in the infraumbilical region lead to apposition of fat to fat when the flap is approximated in position and that this decreases seroma, rapid reconstruction of the lymphatic vessels results in rapid reconstruction of the lymphatic drainage than in traditional abdominoplasty where the superficial lymphatic vessels are cut completely [16].
It is not clear why fat-to-fat apposition should reduce seromas, but it can be conjectured that a fat-to-fat interface leads to less shear movement and/or more "stickiness" between the opposing surfaces, especially when compared with apposing fat to the shiny smooth surface of the rectus fascia, which is the case in more traditional flap elevation [16].
The implication of scarpa's fascia preservation technique does not affect the clinical outcome regarding the aesthetic look, patient satisfaction, edema of the flap. It may has minimal effect on the drain output and seroma formation [16].
Conclusion
The superficial group of patients wasn't pleased by long hospital stay and downtime, prolonged edema formation, prolonged duration till drain removal and supra epigastric higher leveling compared to the infraumbilical level. In contrary of that, the subscarpal and suprascarpal groups of patients gave more satisfactory results.
References
- Avelar JM (2000) Abdominoplasty: A new technique without undermining and fat layer removal. Arq Catarinense Med 2000; 291:147-149.
- Lockwood T (1996) The role of excisional lifting in body contour surgery. Clin Plast Surg 23(4): 695-712.
- Saldanha OR (2007) Lipoabdominoplastia. Caracas, Venezuela: Amolca.
- Mustoe TA, Kim P, Schierle CF (2007) Outpatient abdominoplasty under conscious sedation. Aesthetic Surg J 27(4): 442-449.
- Saldanha OR, Federico R, Daher PF, Malheiros AA, Carneiro PRG, et al (2009) Lipoabdominoplasty. Plast Reconstr Surg 124(3): 934-942.
- Andrades P, Prado A (2007) Composition of postabdominoplasty seroma. Aesthetic Plast Surg 31(5): 514-518.
- Khan UD (2008) Risk of seroma with simultaneous liposuction and abdominoplasty and the role of progressive tension sutures. Aesthetic Plast Surg 32(1): 93-99.
- Fang RC, Lin SJ, Mustoe TA (2010) Abdominoplasty Flap Elevation in a More Superficial Plane: Decreasing the Need for Drains. Plast Reconstr Surg 125(2): 677-682.
- Abu-Hijleh MF, Roshier AL, Al-Shboul Q, Dharap AS, Harris PF (2006) The membranous layer of superficial fascia: evidence for its widespread distribution in the body. Surg Radiol Anat 28(6): 606-619.
- Costa-Ferreira A, Rebelo M, Vasconez LO, Amarante J (2010) Scarpa's fascia preservation during abdominoplasty: a prospective study. Plast Reconstr Surg 125(4): 1232-1239.
- Espinosa-de-los-Monteros A, de la Torre J, Rosenberg LZ, Ahumada LA, Stoff A, Williams EH, et al. (2006) Abdominoplasty with total abdominal liposuction for patients with massive weight loss. Aesthetic Plast Surg 30(1): 42-46.
- Lancerotto L, Stecco C, Macchi V, Porzionato A, Stecco A, et al. (2010) Layers of the abdominal wall: anatomical investigation of subcutaneous tissue and superficial fascia. Surg Radiol Anat 33(10): 72-78.
- Robert CF, Samuel JL, Thomas AM (2011) Abdominoplasty Flap Elevation in a More Superficial Plane: Decreasing the Need for Drains. Plast Reconstr Surg 125: 677.
- Beer GM, Wallner H (2010) Prevention of Seroma After Abdominoplasty. Aesthet Surg J 30(3): 414-417.
- Moore, Keith L, Dalley, Arthur F (2006) Clinically Oriented Anatomy, abdomen (5th edn). Lippincott Williams & Wilkins, USA pp. 192-340.
- Atta AT, Ismail M, Hosny H, Abbas S (2012) The implication of the abdominal wall lymphatic pattern on postoperative sequelae of abdominoplasty (MD thesis). pp. 156-163.
- Al Aly A (2010) Discussion scarpa fascia preservation during abdominoplasty Plast. Reconstr. Surg 125: 1240-1241.
© 2018 Ahmed Hammad, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






