- Submissions

Full Text
Significances of Bioengineering & Biosciences
Bio-fabrication for Regenerative Therapies on Corneal Tissue: A Perspective
Sankhajyoti Saha* and Moubani Dutta
Department of Vision Science, NSHM Knowledge Campus, India
*Corresponding author:Sankhajyoti Saha, Department of Vision Science, NSHM Knowledge Campus, Kolkata, India
Submission: June 30, 2025; Published: August 07, 2025

ISSN 2637-8078Volume7 Issue 4
Abstract
Tissue Engineering, an emerging interdisciplinary field of regenerative health care, is associated with constructing synthetic alternatives to preserve, enhance or restoration of biological tissues that have been degraded and/or injured. Corneal Transplantation (CT) is a restorative visual rehabilitation procedure; its success is contingent on donor tissue standard, recipient pathology and attentive postoperative care. Regenerative medicine has been employed to alleviate corneal disorders through stimulating tissue regeneration by offering the proper micro-environment, variables, cells and/or indications from the host. Degenerated tissue will be restored using a multitude of cell delivery strategies, notably the Extracellular Matrix (ECM) elements, exempted by promoting cell adherence, movement and development, imperative for tissue restoration and regeneration. Following this, the ECM imparts mechanical strength and elasticity to tissues, conveys bio-active cues which authorize cellular behavior, impacting alignment, adhesion, differentiation and upgrades their resilience and bio-availability. Different scaffolding approaches have emerged, leveraging distinct working principles and characteristics to clinically facilitate tissue repair and regeneration by providing structural support, mediating cell behavior and/or delivering bioactive cues within a biomimetic microenvironment. The field of ophthalmology is conveniently centered around bio-compatible apparatus like contact lenses for precise ocular surface regeneration, providing a non-invasive, oxygen-permeable architecture for cell adhesion and proliferation, specifically for disorders like limbal stem cell deficiency, upgrading patient satisfaction and reducing surgical hazards. These intuitive interventions in the field of eye care will be fundamental to expedite their extensive clinical accessibility and patient outcomes.
Keywords: Tissue engineering; Corneal transplantation; Extracellular matrix; Regenerative medicine; Scaffold
Introduction
The enactment of Tissue Engineering (TE) is an innovation that emerged approximately 3 decades preceding and concentrates on implementing bio-materials to construct neo-tissue. Considering its infancy and restricted tissue dimension, this nexus attempts to expand its therapeutic potential while confronting several pervasive barriers and constraints. Cell biology, material science, chemistry, molecular biology, engineering and medicine are all integrated in TE, an emerging interdisciplinary field of regenerative health care, which is associated with constructing synthetic alternatives to preserve, enhance, or restoration of biological tissues that have been degraded and/or injured [1]. A substantial financial and medical concern in contemporary times is tissue and organ dysfunction spurred by medical conditions, trauma and unusual developmental patterns. At the present time, the clinical approach used to contend with this issue is using the content of donated organs as well as tissues. Yet, reliance on provided tissues and organs has never been an effective remedy owing to the chronic shortage of prospective donors, an increasing number of receivers on transplant queues and the older demographic. More importantly, many donated tissues and organs cannot be efficiently compatible, offered and effectively transplanted to the recipient in the severely limited period available due to considerable logistical setbacks [2]. Corneal Blindness (CB) is a considerable public health concern in India, predominantly impacting geriatric groups, children and young individuals, consequently developing Disability-Adjusted Life Years (DALY).
It has evolved into the third fundamental factor of blindness in India, with key ailments that include infective keratitis, trauma, bullous keratopathy, chemical injuries, keratoconus and dystrophies. Corneal Transplantation (CT) is a restorative visual rehabilitation procedure; its success is contingent on donor tissue standard, recipient pathology and attentive postoperative care. Eye banks, crucial for tissue acquisition and dispensation, confront limitations in developing nations, including trained medical crews, equipment and public awareness. Post-transplant rejection endures a considerable concern: Endothelial rejection is the most frequent (50%), followed by mixed rejection (30%), epithelial rejection (2%) and subepithelial rejection (1%). Keratoconus cases show diverse rejection rates, with a large study reporting 22.7%. Regenerative medicine has been employed to alleviate corneal disorders through stimulating tissue regeneration by offering the proper micro-environment, variables, cells and/or indications from the host. Degenerated tissue will be restored using a multitude of cell delivery strategies, notably the Extracellular Matrix (ECM) elements exempted by competent host cells [3-7].
The Intricate Structure of the Cornea
The outermost epithelium, stroma and innermost endothelium are the three transparent layers that constitute the cornea, along with two membranes, Bowman’s membrane and Descemet’s membrane, distinct the stroma and endothelium and the epithelium and stroma, respectively. The most suitable scaffold for tissue engineering needs to resemble the inherent Extracellular Matrix (ECM), yet this proves complicated with regard to its dynamic orientation and intricate configuration [8] (Table 1). Exploring the cornea anatomically and physiologically is essential to comprehend the visual system’s scarcity and insufficiency, with an emphasis on personalized medicinal and surgical regenerative interventions. Multiple ailments, such as keratoconus, dry eye disease, bacterial keratitis, chemical and light damage and trauma, may compromise the integrity of the corneal surface. Due to thinning, inflammation, infection or mechanical injury, these pathological conditions disrupt the integrity of different layers, contributing to symptomatic visual distortion. To reclaim corneal efficiency and transparency, advanced stages might necessitate either regenerative intervention [8]. The Extracellular Matrix (ECM) contributes an indispensable impact on tissue architecture and execution with clinical considerations.
Table 1:The intricated structure of the cornea and the barriers to TE.
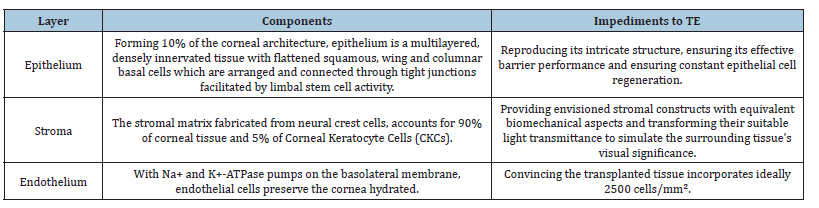
The first point to enquire is that it acts as a scaffold that reinforces cell adherence, movement and development, imperative for tissue restoration and regeneration. Following this, the ECM imparts mechanical strength and elasticity to tissues, which is essential for activities such as the tensile strength of tendons and the adaptability of skin. Another important aspect is, it conveys bioactive cues which authorize cellular behavior, impacting alignment, adhesion, and differentiation. In addition, the concept that the ECM performs as a reservoir for growth-promoting components, upgrading their resilience and bioavailability, is significant for facilitating wound healing and tissue regeneration. Ultimately, its degradable inclination enables dynamic remodeling, authorizing neovascularization and tissue restructuring in the course of development, repair and pathological alterations [7].
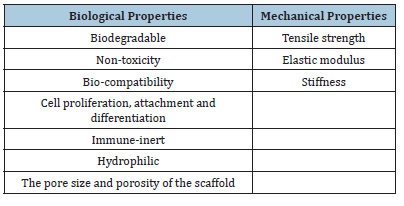
The Properties of Scaffold
Biodegradability is important for scaffold integration, enabling it to be substituted with biological tissue. Sterilization is integral to circumvent infection and the scaffold has to encourage cell adhesion for tissue regeneration. Mechanically, tensile strength, elastic modulus and stiffness are pivotal for structural integrity and durability, preferably resembling its predecessor’s traits to assure efficient execution and prevailing tissue engineering culminates [9- 15] (Table 2).
Table 2:The properties of scaffold.
Scaffold material types
Determining resources for biomedical scaffolds is important and entails implementing certain criteria that involve form and structure, molecular weight, material chemistry and surface properties like surface energy, solubility, lubricity, hydrophobicity and hydrophilicity. Additionally, the material’s erosion and degradation framework and hydrophilic capacity have to be maintained with the intended application. Multiple components, such as polymers, ceramics, glasses, metals, alloys and their synthetic materials, are extensively explored considering their distinctive attributes associated with such essential instances [9,16,17].
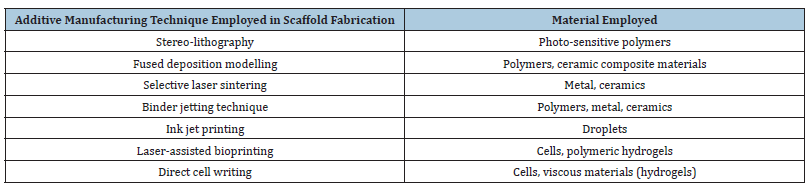
Fabrication method
Distinctive fabrication innovations were initially constructed to obtain a scaffold framework, traditionally organized as conventional techniques and additive manufacturing techniques. Every kind of method contributes distinctive elements of architecture to the scaffold, concerning essential components like pore size, structure, inter-connectivity and mechanical characteristics [9] (Table 3 & 4).
Table 3:List of material employed in various conventional technique in scaffold fabrication.
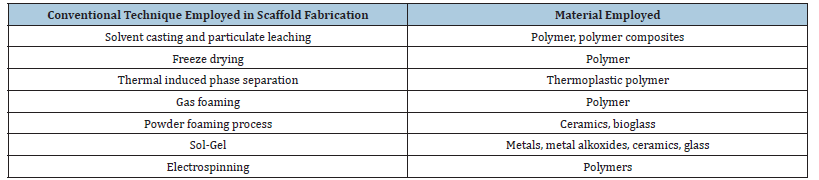
Table 4:List of material employed in various additive manufacturing technique in scaffold fabrication.
The Approach of Scaffolding
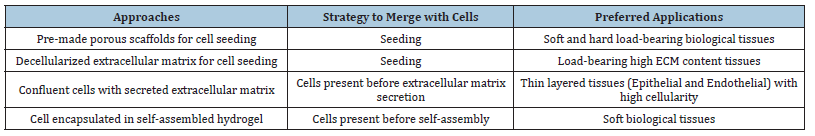
There can be numerous impediments to conventional organ and tissue restoration methods like auto-grafting and allografting, for instance, constrained accessibility and availability, immune system resistance factors and the opportunity for transmission of infectious diseases. An attainable approach using the scaffolds is to provide a structural and functional framework by resembling the Extracellular Matrix (ECM). In clinical terms, effective scaffolds need to stimulate new tissue development and neovascularization by promoting redesigning to integrate with the host tissue. In recognition of the reconstruction of tissues, they additionally need form stability and mechanical strength. For reliable and productive regeneration, it is imperative to ensure the biomaterials employed are biocompatible with biological cells and fabricated tissues. Tissue engineering scaffolds can be extensively characterized about multiple attributes like properties, material type, fabrication method and whether they are cell-seeded or acellular [9]. Over the past two decades, four major scaffolding approaches in tissue engineering have emerged, each leveraging distinct working principles and characteristics to clinically facilitate tissue repair and regeneration by providing structural support, mediating cell behavior and/or delivering bioactive cues within a biomimetic microenvironment [7,18,19] (Table 5).
Table 5:Scaffolding approaches.
Future Perspective
The prospect of regenerative medicine offers promising insights transcending the standard scaffolds. Expansive tissue engineering initiatives prioritize on industrial-scale fabrication and appropriate material attributes, the field of ophthalmology is conveniently centered around bio-compatible apparatus like contact lenses for precise ocular surface regeneration, providing a non-invasive, oxygen-permeable architecture for cell adhesion and proliferation, specifically for disorders like limbal stem cell deficiency, upgrading patient satisfaction and reduction of surgical hazards. Therefore, by confronting the constraints associated with conventional interventions, such as the prospect of immune rejection and donor tissue limitations, bio-fabrication modalities suggest significant potential in corneal regeneration interventions. Scaffold-based innovations, particularly hydrogels and electrospun nanofibers, closely resemble the Extracellular Matrix (ECM), providing a favorable environment for cell adhesion, migration and differentiation while preserving the rigidity and optical transparency of the cornea. The synthesis of mesenchymal and limbal stem cells into the intended scaffolds enhances regeneration efficacy through offering supportive structures and synergistic biochemical activation. Cell sections and media are examples of scaffold-free cell transport systems that have therapeutic significance due to their reduced interference and enhanced biocompatibility.
Adequate tissue recovery and adaptation are additionally facilitated by pharmacological and immunomodulatory aspects of new biomaterials, especially decellularized tissues and foundation derived from amniotic membranes. Considering the clinical use of entirely bioengineered corneal conceptualization to be effective and adaptable, subsequent experiments should involve constraints with sterilization and regulatory authorization. Comprising contact lenses with growth factor-rich solutions, such as autologous serum, additionally enhances their regenerative potential, promoting corneal integrity and transparency [7,18,19]. These intuitive interventions in the field of eye care will be fundamental to expedite their extensive clinical accessibility and patient outcomes.
References
- Sharma P, Kumar P, Sharma R, Bhatt VD, Dhot PS (2019) Tissue engineering; current status & futuristic scope. J Med Life 12(3): 225-229.
- Lanza R, Langer R, Vacanti JP, Atala A (2020) Principles of tissue engineering. Academic Press, New York, USA.
- Gupta V, Vashist P, Sarath S, Gupta N, Senjam SS, et al. (2025) Burden of blindness and visual impairment associated with corneal opacities in India. Br J Ophthalmol 109(7): 829-836.
- Anitha V, Tandon R, Shah SG, Radhakrishnan N, Singh S, et al. (2023) Corneal blindness and eye banking: Current strategies and best practices. Indian Journal of Ophthalmology 71(9): 3142-3148.
- Gurnani B, Czyz CN, Mahabadi N, Shane JH (2023) Corneal graft rejection. StatPearls.
- Rahimzadeh M, Hajizadeh E, Feizi S (2010) Cure rate following rejection in bilateral corneal grafts for keratoconus. J Ophthalmic Vis Res 5(3): 145-150.
- Mahdavi SS, Abdekhodaie MJ, Mashayekhan S, Baradaran RA, Djalilian AR (2020) Bioengineering approaches for corneal regenerative medicine. Tissue Eng Regen Med 17(5): 567-593.
- Orash MA, Heidari KS, Poursamar SA, Zarrabi A, Sefat F, et al. (2022) Bioprinted membranes for corneal tissue engineering: A review. Pharmaceutics 14(12): 2797.
- Suamte L, Tirkey A, Barman J, Jayasekhar BP (2023) Various manufacturing methods and ideal properties of scaffolds for tissue engineering applications. Smart Materials in Manufacturing 1: 100011.
- Babensee JE, Anderson JM, Larry VM, Mikos AG (1998) Host response to tissue engineered devices. Advanced Drug Delivery Reviews 33(1-2): 111-139.
- Brown BN, Valentin JE, Stewart AM, George P, Badylak SF (2009) Macrophage phenotype and remodeling outcomes in response to biologic scaffolds with and without a cellular component. Biomaterials 30(8): 1482-1491.
- Lyons FG, Amir AM, Kieran SM, Toner ME, Ciara MM, et al. (2010) The healing of bony defects by cell-free collagen-based scaffolds compared to stem cell-seeded tissue engineered constructs. Biomaterials 31(35): 9232-9243.
- Shigley JE, Mitchell LD, Saunders H (1985) Mechanical engineering design. J Mech Trans and Automation 107(2): 145.
- Kenar H, Kocabas A, Aydinli A, Hasirci V (2008) Chemical and topographical modification of PHBV surface to promote osteoblast alignment and confinement. Journal of Biomedical Materials Research Part A 85(4): 1001-1010.
- Siritientong T, Srichana T, Aramwit P (2011) The effect of sterilization methods on the physical properties of silk sericin scaffolds. AAPS PharmSciTech 12(2): 771-781.
- Nikolova MP, Chavali MS (2019) Recent advances in biomaterials for 3D scaffolds: A review. Bioactive Materials 4: 271-292.
- Ribas RG, Schatkoski VM, Amaral ML, Menezes BR, Cristiane S, et al. (2019) Current advances in bone tissue engineering concerning ceramic and bioglass scaffolds: A review. Ceramics International 45(17): 21051-21061.
- Chan BP, Leong KW (2008) Scaffolding in tissue engineering: General approaches and tissue-specific considerations. Eur Spine J 17(4): 467-479.
- Wang M, Li Y, Wang H, Li M, Wang X, et al. (2023) Corneal regeneration strategies: From stem cell therapy to tissue engineered stem cell scaffolds. Biomedicine & Pharmacotherapy 165: 115206.
© 2025 Sankhajyoti Saha*, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






