- Submissions

Full Text
Research in Medical & Engineering Sciences
Nanotechnology as an Alternative to Chemotherapy
Dalvinder Singh Grewal*
Department of English, Guru Nanak Dev Engineering College, India
*Corresponding author: Dalvinder Singh Grewal, Department of English, Guru Nanak Dev Engineering College, Ludhiana, India
Submission: October 14, 2021Published: November 16, 2021

ISSN: 2576-8816Volume9 Issue4
Introduction
“I would better die than lose my hair”, said one of my close relatives. She had cancer and she was advised chemotherapy. She has seen bald heads of men and women having gone through chemotherapy. Not only this; they were found fatigued, feeling and being sick, getting frequent Infections, anaemia, bruising and bleeding, sore mouth, loss of appetite, memory loss, concentration problem, sleep problem, sex and fertility issues, diarrhoea and constipation, emotional problems and much more. Being a learned woman; she knew that the drugs used for chemotherapy are powerful, highly toxic and they can still cause damage to healthy cells. This damage causes the side effects as do all the sulpha drugs.
Most chemotherapy (chemo) drugs are strong medicines that have a narrow range for dose safety and effectiveness. Chemo drugs kill fast-growing cancer cells. Even normal, healthy cells that are fast-growing too, affected because these drugs travel throughout the body. Damage to healthy cells causes side effects. The normal cells most likely to be damaged by chemo are Blood-forming cells in the bone marrow, hair follicles, Cells in the mouth, digestive tract, and reproductive system. Some chemo drugs can damage cells in the heart, kidneys, bladder, lungs, and nervous system.
Drug will not treat the cancer if it is taken too little but life-threatening side effects can be caused if it taken in large quantities. It is also not sure that even after chemotherapy the cancer patient would survive. There are many in her neighbourhood who died after chemotherapy treatment. “I dread this most inhuman treatment. Please find some alternative for it”, she said. Bathinda is a hotbed for cancer. You will find cancer patient in every alternative village. Train goes to Bikaner daily taking cancer patients to Government Cancer Hospital and is known as cancer train.
Alternative Treatments to Chemotherapy
As I studied the material available on net and books and found that alternative therapies to chemotherapy include photodynamic therapy, laser therapy, immunotherapy, targeted therapy, and hormone therapy. There were 10 other options to consider but it was also mentioned that the alternative cancer treatments can’t cure your cancer, but they may provide some relief from signs and symptoms. Alternative cancer treatments may help you cope with signs and symptoms caused by cancer and cancer treatments, but they may not play a direct role in curing your cancer. Alternative treatments may lessen anxiety, fatigue, nausea and vomiting, pain, difficulty sleeping, and stress the common signs and symptoms. Alternative cancer treatments may offer some feeling of control, but many alternative cancer treatments are unproved as these may be turned out to be dangerous. Ten alternative cancer treatments generally found safe as these may provide some benefit. To get her some relief, I read out to her: “If you are feeling anxiety try hypnosis, massage, meditation or relaxation techniques. If you feel fatigued do exercises, massage, relaxation techniques
and yoga. If you feel nausea and vomiting try acupuncture,
aromatherapy, hypnosis and music therapy. If you have pain, try
acupuncture, aromatherapy, hypnosis, massage and music therapy.
If you have sleep problems do exercise, relaxation techniques,
yoga and if you feel stressed try aromatherapy, exercise, hypnosis,
massage or, meditation.” I researched further to find an answer to
her questions and found that: “The majority of cancers cannot be
avoided by simple exercises, yoga or behavioural changes. They
require technological innovation to improve outcomes”.
As I was discussing this with her, she told me, “These allalternative
treatments appear to be for the aftereffects of
chemotherapy which I said I do not want. Why not try your
Nano medicine? You used to talk about your research on burning
the cancerous cells directly through heated gold nanoparticles
without affecting any other part of the body. Why not elaborate
on that?” I remembered our discussions with Director Cancer
Hospital, Muktsar whenever he came to teach M.Tech classes in
nanotechnology from 2006-2011. This lady was the professor in
Biology who also participated in discussion. We tried in laboratory
firing of heated gold-headed nano-arrows on to the dummy cancer
cells and burning these. This was an effort to localise cancer cell
burning rather than chemotherapy treatment which had many
problems for the patients.
Imaging tests like X-rays, CT scans, and MRIs are ofter orders
by doctors to help diagnose cancer these days. However, these
tests are only when the tumours are big enough to be seen. But
by that time the cancer cells would have copied themselves many
times and spread to other parts of the body. These scans also can’t
show whether a tumour is cancer or not for which biopsy is the
answer. Being of nanoscale, Nanotechnology can detect very minute
changes in cells and difference between normal and cancer cells
can be found. Getting at the cancer cells at the earliest stages, while
cells just start dividing, cure of cancer is easier.
Seeing tumours on Nanotechnology imaging tests makes these
cells easier to identify. Nanoparticles with antibodies or other
substances coatings help them find and stick to the cancer cells.
When signals about cancer are received, nanoparticles can be coated
with substances. As an example of this, iron oxide nanoparticles
bind to cancer cells sending off a strong signal that lights up the
cancer on MRI scans. Doctors can be helped by nanotechnology
to locate cancer in blood or tissue samples. Pieces of cancer cells
or DNA that are too small for current tests to pick up can also be
spotted. Cancer treatments can be made safer and more precise
by nanotechnology. Medicines like chemotherapy can be delivered
straight to the tumour by specially designed nanoparticles. On
reaching the target only, they release the medicine and not before
that. Healthy tissues around the tumour are saved from drugs from
damaging the harming. Side effects which otherwise occur from
this damage are thus avoided [1].
Now it is a decade since the doctors have used nanotechnology
to treat cancer. Abraxane and Doxil are the two approved treatments
which help chemotherapy drugs work better. Nanoparticle made
from the protein albumin Abraxane is attached to the chemo
drug docetaxel which stops cancer cells from dividing. Breast and
pancreatic cancers that have spread, and non-small-cell lung cancer
are treated by Abraxane. Wrapped inside a liposome, a fatty sack,
Doxil is the chemo drug doxorubicin which disrupts cancer genes so
the cancer cells can’t divide [2]. Ovarian cancers, multiple myeloma,
and Kaposi’s sarcoma are treated by Doxil. Other nanotechnology
treatments in clinical trials include the treatments wrap toxic drugs
in nanoparticles to make them safer. They may also help the drug
survive the trip through the bloodstream. Nanoparticles might also
be able to deliver radiation to cancer after some time.
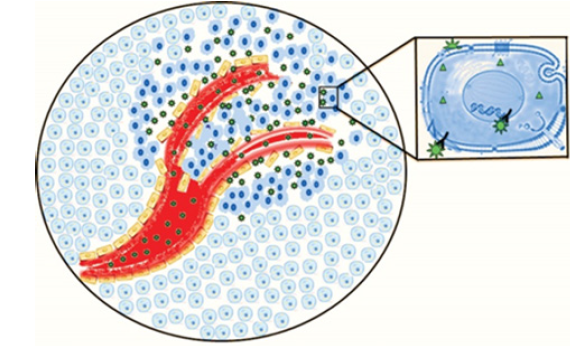
Figure 1
Abraxane and Doxil the current nanotechnology-based
treatments do cause some side effects like weight loss, nausea,
and diarrhoea which may be from the chemotherapy drugs which
they contain. Side effects of these treatments need further research
through clinical trials [3]. Cancer caused by viral infections [e.g.,
Human Papilloma Virus (HPV) has been limited successfully [4–
6]. Using more widespread implementation of existing vaccine
technologies, by using nanotechnology and other technologies
for improving vaccination efficiency this success could be further
enhanced [7]. Early diagnose through improved imaging through
nanotechnology may increase the percentage of treatred cancers.
This can be further developed in conjunction with more aggressive
implementation of existing screening technologies leading to
improved outcomes for cancer patients [8,9]. Types of cancer
are stated to be of over 700 types for which new approaches for
treating established disease are required. For this, nano-sized
molecular tools capable of distinguishing between malignant and
non-malignant cells and for delivering a lethal payload should
be developed. Tumour targeting is the most studied for cancer
treatment (Figure 1). Both active and passive targeting of NP
targeting of malignant cells are depicted above [10]. NPs (green
stars) accumulate in tumour tissue via the EPR – a form of passive
targeting. Inset – shape-specific interaction of the NPs with cellsurface
receptors is indicated by “Y-star” interactions that represent
active targeting of NPs to cancer cells based upon specific molecular
interactions.
In this first the malignant cancer cells are detected and then
selectively eradicated. Passive and active targeting is done to detect
the malignant cells. To increase the concentration of Nanoparticles
(NPs) in the tumour, advantage of the Enhanced Permeability and
Retention (EPR) effect helps passive targeting [11,12]. Selective
molecular recognition of antigens, frequently proteins that are
expressed on the surfaces of cancer cells to localize NPs to malignant
cells helps Active targeting [13]. It may involve or, alternatively,
exploit biochemical properties associated with malignancy such
as matrix metalloproteinase secretion [14]. The two approaches
may be combined, or Passive and Active targeting may be deployed
independently. Both strategies minimize uptake by the Macrophage
Phagocytic System (MPS) and maximizing time in circulation there
by giving the benefit from surface modifications of NPs that [15].
Review
For more than a decade now doctors have used nanotechnology to treat cancer with Abraxane and Doxil, the two approved treatments. The active and passive targeting techniques have been tested only in laboratory and are available for treatment hence may take some time to be effectively used at medical level globally. Thus, alternative to chemotherapy has been provided by nanotechnology.
References
- Laura J, Martin MD (2020) Nanotechnology for cancer treatment and management, National center for biotechnology information, US National Library of Medicine8600 Rockville, USA.
- Op Cit.
- Op Cit.
- Moniz M, Ling M, Hung CF, Wu TC (2003) HPV DNA vaccines. Front Biosci 8: d55-d68.
- Parkin DM, Bray F (2006) The burden of HPV-related cancers. Vaccine 24(Suppl 3): 11-25.
- Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, et al. (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1): 12-19.
- Paavonen J, Naud P, Salmeron J, Wheeler CM, Chow SN, et al. (2009) Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 374(9686): 301-314.
- Nystrom L, Rutqvist LE, Wall S, Lindgren A, Lindqvist M, et al. (1993) Breast cancer screening with mammography: overview of Swedish randomised trials. Lancet 341: 973-978.
- Winawer S, Fletcher R, Rex D, Bond J, Joseph F, et al. (2003) Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology 124(2): 544-560.
- William HG, Supratim G (2013) Nanotechnology for cancer treatment. Nanotechnol Rev 3(2): 111-122.
- Maeda H (2001) The enhanced permeability and retention (EPR) effect in tumour vasculature: the key role of tumour-selective macromo-lecular drug targeting. Methods Mol Biol 624: 25-37.
- Maeda H (2012) Macromolecular therapeutics in cancer treatment: the EPR effect and beyond. J Control Release 164(2): 138-144.
- Byrne JD, Betancourt T, Brannon PL (2008) Active targeting schemes for nanoparticle systems in cancer therapeutics. Adv Drug Deliv Rev 60(15): 1615-1626.
- Hongmei Li SSY, Miteva M, Nelson CE, Werfel T, Giorgio TD, et al. (2013) Matrix metalloproteinase responsive, proximity-activated polymeric nanoparticles for siRNA delivery. Adv Funct Mater 23(24): 3040-3052.
- Nie S (2010) Understanding and overcoming major barriers in cancer nanomedicine. Nanomedicine (Lond) 5(4): 523-528.
© 2021 Dalvinder Singh Grewal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






