- Submissions

Full Text
Research in Medical & Engineering Sciences
Clinical Case -Post-Traumatic Lower Lip Angiofibroma
Igumnov VA1* and Kasyanov AA2
1Department of Plastic Surgery of the Center for Plastic Surgery and Cosmetology, Russia
2Department of Plastic Surgery of the multidisciplinary medical center, Russia
*Corresponding author: Igumnov Vitaliy Aleksandrovich, Candidate of medical sciences (PhD), Full member of the Society of Plastic, Reconstructive and aesthetic surgeons-SPRAS, Surgeon of the Department of plastic surgery of the center for plastic surgery and cosmetology, Novosibirsk city, Russia
Submission: October 27, 2020Published: November 20, 2020

ISSN: 2576-8816Volume9 Issue1
Case Report
Quite often the reason for seeking medical care is about the consequences of injuries to the facial area. And, as plastic surgeons, we are working to eliminate these consequences. Correction of aesthetic lip defects is one of the most common reasons for such appeals.Lip trauma is often the result of motor vehicle collisions, contact sports, interpersonal violence, occupational and domestic accidents, and bite wounds[1].In addition, the number of aesthetic procedures in the lip area is increasing, which is associated with the youth and beauty(Figures 1-3). According to ISAPS, the number of procedures using hyaluronic acid fillers in soft tissues increased from 2.69 million in 2014 to 3.3 million in 2017. Complications that require subsequent correction may also be associated with these procedures [2,3].Our clinical case is associated with the consequences of trauma and the formation of a hematoma in the lower lip.
Figure 1: Ultrasound image demonstrating the course of the cyst.
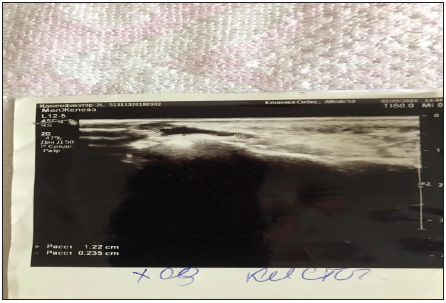
Figure 2:Lumen of the cyst.

Figure 3: Preoperative markup.

A 61-year-old female patient complained of a dense neoplasm and swelling in the left half of the lower lip. As reported by the patient, about 20 years ago she had a lower lip injury that resulted in a large hematoma formation. Reabsorption of the hematoma was incomplete. After 3 weeks, a moderately dense formation appeared in the lower lip. She did not see the doctor about it.Six months ago, she went to an oral facial surgeon to remove the formation. The ultrasound examination of the soft tissues of the lower lip and chin was performed(Figures 3-6).
Figure 4: Large vessels fixed with clamps.

Figure 5: After suturing a postoperative wound.

Figure 6: Angiofibroma removed in operation.

Submitted ultrasound: On the lower lip on the left, under the mucous membrane, a fluid formation of 6.6 mm, with a thickened capsule and anechoic course 12.7x2.3mm. In the chin area, subcutaneously, fibrous tissue. Conclusion: a cyst of the soft tissues of the lower lip with mucosal hyperplasia with its own course. Fibrosis of soft tissues in the area of injury. After the study, there was an attempt at resection. Intraoperatively, the surgeon assessed the feeding vessel resection as risky and did not remove the neoplasm. In the projection of the left corner of the lower lip, an arterial vessel with a diameter of 3.3mm is determined, the course is arcuate, with the apex at the red border of the lip. Higher (by 1.2mm), a single-chambered rounded formation with thin walls, hypoechoic homogeneous structure, moderately compensated by 3.1mm (mucocele).In July, she came to us. On examination, in the area of the lower lip on the left, on the border with the vermilion, there is an elevation of the mucous membrane of a dark color, softelastic consistency. On the border with the vermilion, to the left of the middle of the lip to the corner of the mouth, a scar is visible, thin, pale pink, painless with moderate compaction. A weak ripple is detected. After examining the patient, taking into account the results of ultrasound, we decided to respect the neoplasm
Operation protocol
The operation was performed under local anesthesia with 2% lidocaine solution. The first surgical step is done in wet-dry mucosal passage of the lower lip. incision was made in the area of the old scar, at the border of the vermilion of the lip and mucous membrane, and the formation was isolated. The vessels were bluntly and sharply highlighted, the vessels carrying out both the inflow and outflow of blood, up to 3mm thick, were fixed with clamps, their pulsation was visible. The neoplasm was resected; for the purpose of hemostasis, large vessels were stitched with Vicryl 5-0, small capillaries were coagulated. Suturing of the postoperative wound was carried out with Vicryl 5-0, the suture was inside the mucosa. Removal of stitches was on the 7th day. During 6 months of follow-up, there is no relapse.
Histological picture: a nodular formation of elements of the fibroblastic row in the edematous stroma with areas of myxomatosis, disseminated lymphoplasmacytic infiltration, plethora, stasis in small and medium-sized vessels, areas of diapedetic hemorrhage, fibrosis. Diagnosis: Angiofibroma.
Conclusion
Early visit of patients to the doctor after injuries or invasive procedures can prevent or minimize the consequences.
References
- Grunebaum LD, Smith J, Hoosien G (2010) Lip and perioral trauma. Facial Plastic Surgery 26(6): 433-444.
- Jonathan M, Travis T (2019) Management of lip complications. Facial Plastic Surgery Clinics of North America 13(1): 157-167.
- ISAPS International survey on aesthetic/cosmetic procedures (2018).
© 2020 Igumnov VA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






