- Submissions

Full Text
Research in Medical & Engineering Sciences
Lean Thinking from Toyota Manufacturing to the Healthcare Sector
Hisham Kelendar*
Faculty of Health Studies, University of Bradford, Kuwait
*Corresponding author: Hisham Kelendar, Faculty of Health Studies, University of Bradford, Bradford, UK. Physician, Ministry of Health, Kuwait
Submission: April 06, 2020 Published: April 29, 2020

ISSN: 2576-8816Volume8 Issue5
Abstract
Purpose: This paper aims to provide a historical overview of how lean thinking has transferred and spread from Toyota manufacturing to the healthcare sector. It aims to explain the origin of lean: how it is defined, the main tools, concepts, and principles behind it, provide some lean healthcare examples, and explore the differences between the manufacturing and healthcare systems.
Design/methodology/approach: The article reviews current literature for lean application in healthcare from five databases. More than 50 articles and books were considered according to a taxonomy suggested.
Findings: Lean originated from Toyota in the 1940s due to the need to increase production efficiency, specifically by reducing waste. Since then, lean has expanded to other industries and organisations, gradually advancing to services and, since the beginning of the twenty-first century, have also been used in the healthcare sector. While the philosophy was introduced to the world by Toyota, the term ‘lean’ was only introduced by Jon Krafcik in the late 1980s. Lean initially lacked an agreed-upon definition within the literature; any agreement reached was on the potential of lean thinking in the healthcare sector. Several lean tools and techniques were used by different organisations, mostly to reduce or eliminate waste. Some of the leading examples of lean healthcare include the United States of America’s (USA) Virginia Mason Medical Centre, Theda Care in Wisconsin (USA), Bolton Hospital in England, and the Saskatchewan health care system in Canada. Even with the encouraging success stories from adopting lean as a management approach, several challenges still remain. The healthcare sector differs greatly from the motor industry as hospitals are not factories, so the transition between the two is not straight forward.
Originality/Practical implications: This literature review is helpful for journal editors and reviewers, researchers in healthcare organisations and healthcare practitioners as it offers a comprehensive, historical overview of how lean thinking has transformed and spread from Toyota manufacturers to the healthcare sector.
Keywords: Lean; Toyota production system; Just in Time; Health services; Hospital; Patient
Introduction
Lean thinking (also referred to as lean philosophy, lean management or just lean) originated from Toyota in the 1940s due to the need to increase production efficiency by reducing waste, inventory and labour [1]. It was later integrated into the production management of companies and manufacturers (e.g. Boeing, Nike) and then spread to other service industries (e.g. Tesco, Amazon) [2-4]. Following this, its applicability rapidly extended to both the public and private service sectors-notably healthcare- and lean currently remains part of the culture of leading institutions such as the Virginia Mason Hospital or the Mayo Clinic [5,6]. The aim of this paper is to provide a historical overview of how lean thinking has transformed and spread from Toyota manufacturing to the healthcare sector. It proposes to explain the origin of lean, how it is defined, the main tools, concepts, and principles behind it, discuss lean healthcare examples, and compare differences between the manufacture and healthcare systems.
Methodology
Various databases and grey literature were used to search the relevant publications related to lean thinking among Toyota manufacturers and healthcare. The keywords used in this paper included expressions such as ‘Lean’, ‘Toyota production system’, ‘Just in Time’, ‘Health services’, ‘Hospital’, and ‘Patients’. Over 60 sources were found where reviewing the references cited in the selected publication also added important recourse.
The origin of lean
The origin of lean philosophy is linked to the industrial process. Therefore, to understand lean, it is necessary to look at Fordism, an American process of mass production, adopted worldwide, which produced high volumes of standardised and low-cost goods [7]. Inspired by the Frederick Taylor and Henry Ford models, Toyota has developed an innovative business approach to reduce costs by eliminating anything unnecessary to the Toyota Production System (TPS) [8]. This approach has changed the paradigm and management concepts of the twentieth century. According to Womack, Jones [9], the pioneers in the concept of TPS were Eiji Toyoda & Taiichi Ohno [10] of the Japanese Toyota auto industry. This production method was preceded by artisanal production and mass production. Mass production emerged in the United States of America (USA) as an alternative to artisanal production in the early twentieth century, mainly due to its high costs and lack of general accessibility. Henry Ford, with the introduction of mass production, overcame the problems inherent to artisan production by drastically reducing costs while increasing product quality [9]. The shift from mass production to TPS was largely due to the high price of machinery and poor flexibility: keeping standard models in production as long as possible, and workers attending monotonous working methods [9]. Furthermore, according to Ohno [10], the reduced market and the need to produce a variety of vehicles on the same assembly line eventually encouraged the search for improvements in the process, aiming for flexibility and low costs while still meeting the needs of its customers. In this context, the TPS paradigm has developed and stood out due to its high productivity [11]. Womack, Jones [9] argue that TPS has advantages over mass production since it allows increased productivity and flexibility without the inflated costs of artisanal production and the excessive rigidity of production.
TPS originates from the post-war period in Japan. After World War II, Japan was short on resources (people, space, materials, etc.) relative to the Western countries, which drove Toyoda and Ohno [10] to the conclusion that mass production, would be unsuitable [9]. They would have to be competitive with quality and pricing, providing product variety (unlike Western countries) and developing a whole new manufacturing system in order to survive. Thus, TPS was created to methodically eliminate waste and direct attention to customer satisfaction. Therefore, Toyota managers adapted TPS arguing that their current production methods were neither practical nor economically sustainable [12]. Increasing market instability, globalised competition and an increase in consumers no longer allowed companies to capture ‘market share’. The greater flexibility and competitiveness of Japanese production, transmitted by this new philosophy, is thus underpinned by its ability to produce many cheap models in small number and has been increasingly accepted as the solution to replace Fordism [10].
During the creation of TPS, Ohno [10] identified a number of flaws in the company's production system. He found that excess inventory led to increased costs, increased need for physical space and defective and obsolete products. Ohno [10] wrote, ‘All we are doing is looking at the timeline from the moment a customer gives us an order to the point when we collect the cash. And we are reducing that timeline by removing the non-value-added wastes [13]. Ohno [10] decided that employees were to be an active part of the decisions made at the company as they were keenly aware of the mechanisms and failures in production. Among other established changes, one-member work teams were set up, grouped by industry, and met periodically to make suggestions for continuous improvement: kaizen (a Japanese expression meaning ‘change for the better’). Moreover, these factory employees were instructed to stop work as soon as an error was detected. In this way, the whole team would come together to find a solution to the problem and prevent it from happening again. Ohno [10] also set up a problem-solving system known as ‘five whys’ when errors occur, in order to gain access to their cause through five levels of discussion. Until then, the errors that occurred were treated as isolated acts and simply expected to not happen again [1]. TPS is characterised by the philosophy of continuous improvement, focused on reducing waste through the involvement and participation of all, aiming to improve quality and safety and reducing costs and process times. These achievements lie on two pillars: Just in Time and autonomation (jidoka) [8]. The first is characterised by producing exactly what customers want, when they want it and the quantities they want it in. In other words, neither sooner nor later, neither more nor less: only the necessary. The second concerns automation with human characteristics. It provides the operator or the machine with the autonomy to cease processing whenever an abnormality is detected within the machine.
TPS became the model for the application of what has become a global movement known as ‘lean’ [11] that has expanded to other industries and other service sectors. Lean in the service industry was advocated by Levitt in his articles ‘Production line approach to service’ 1972 and ‘The industrialisation of service’ 1976. Lean, as a term introduced in the late 1980s, has never been historically used by Toyota itself [9, 14]. While the philosophy was introduced to the world by Toyota, the term ‘lean’ was only introduced by Jon Krafcik [15] , CEO of Hyundai Motor America, in the late 1980s. Jon Krafcik [15] introduced lean in the International Motor Vehicle Program, a study conducted at the Massachusetts Institute of Technology on the future of cars [15]. Jon Krafcik James [15], Womack, Daniel Jones & Daniel Roos [1-23] studied the success of the Japanese automobile manufacturing industry and concluded that all producers in this industry had a similar way of working from Toyota. Lean management is a generic term that includes several key practices that aim at efficiency and value preservation based on stream optimisation [7]. Lean management offers production that consumes considerably less human resources, capital investment and production space to produce the same volume in less time and with fewer defects compared to the mass production model [7]. Lean management suggests a new paradigm for the organisation of work, including the establishment of a relationship of trust with workers, suppliers and customers, promising the elimination of waste, cost reduction and improved product quality [15].
The definition of lean
As itself, lean did not have an agreed-upon definition within the literature but it is characterised by at least six features: Just in Time, resource reduction, improvement strategies, defects control, standardisation and scientific management [16]. Several definitions of lean thinking are found in the literature, however, all share the same basic principle: do more with less. This refers to reducing or eliminating waste and increasing value creation [1]. McIntosh & Cookson [17] mentioned that ‘Lean is considered a philosophy or paradigm rather than a dogmatic set of practices and procedures’. It is therefore difficult to obtain a precise definition that is universally accepted, with several possible definitions existing [17]. In his article ‘Triumph of the lean production system’, Krafcik [15], introduced the lean concept as it reflects the notion of using less of everything to enhance both organisation efficiency and productivity. The first authors to label the Toyota manufacturing philosophy as ‘lean’ to be more explicit were Womack & Jones [9]. The main notion behind this philosophy is to minimise waste and maximise the benefit for the customer using the fewest possible resources to create an efficient system [18]. Womack & Jones [1] stated that lean management is lean ‘because it provides a way to do more and more with less and less-less human effort, less equipment, less time, and less space-while coming closer and closer to providing customers with exactly what they want’. One of the most repeatedly cited lean definitions is written by Shah & Ward [19], who defined lean production as ‘an integrated socio-technical system whose main objective is to eliminate waste by concurrently reducing or minimizing supplier, customer, and internal variability’. Ohno [10] described lean differently, highlighting two concepts that were responsible for increasing production efficiency: respect the human being and consistently eliminate waste. More definitions are provided in Table 1.
Table 1: Other definitions of lean.

Broadly speaking, lean is customer focused, continually improving through reducing waste (with consequent reduction of time and costs) and perfectly adjusting processes to the value chain [11]. The pursuit of this perfection requires the continuous elimination of waste or elements without value so that the customer receives higher value care. Another possible form of definition is to describe the five established lean principles originally developed for the industry by Womack & Jones [23]: set the value, determine the value stream, establish a flow, implement the pull system and achieve the ideal of perfection. These are the lines of force for a successful implementation of lean thinking. However, before discussing the five lean principles, the next section will focus on a clarification of lean thinking activity.
The classification of lean thinking activities
According to Womack & Jones [9], lean production brings together the activities of the entire organisation - from top management to workers to suppliers-able to meet market demand, doubling production and quality while keeping costs down. Essentially, lean thinking is nothing more than a management philosophy that aims to increase customer value by eliminating waste [9].
All activities, tasks, processes or actions are classified according to Hines & Taylor [24] and Womack & Byrne [25] as:
Activities that add value (AV) increase product or service value from the customer perspective.
Activities that do not add value (NAV) are not necessary and the end customer would not pay for them. These must be eliminated in the short term because they consume resources and add costs.
Necessary activities that do not add value (NNAV) do not increase product or service value, nor would the final customer pay for them, and, if possible, are eliminated in the long term.
As determined by Womack & Jones [1], any action that absorbs resources but does not added value for the customer must be classified and treated as waste. According to Hines & Taylor [24], lean manufacturing's approach differs from traditional and mass production systems as it is aimed at eliminating waste and attacking NAV activities, while mass production is only concerned about activities that AV.
Lean principles
According to Womack & and Jones [1], lean thinking can be summarised in five principles (Figure 1). Once the principles of lean thinking become understandable, implementing their philosophy becomes easier. These principles are based on the underlying assumption that organisations are made up of processes and that by applying these principles sequentially, in stages, organisations can add value, reduce waste and continually improve processes [22].
Figure 1: The five principles of lean thinking.
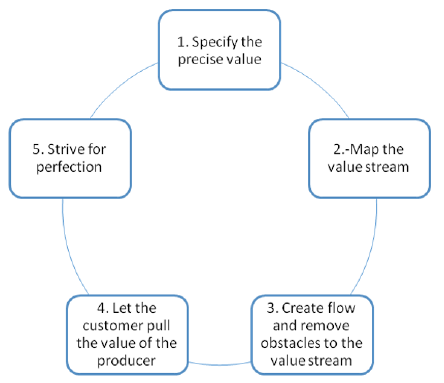
Value
Identify the value for the customer and determine what actually yields results the customer is willing to pay for. Work must be done to optimise the processes that give the product the characteristics the customer expects, and eliminate or optimise other processes so as not to invest resources in areas the client does not value.
Value stream
The value stream represents the steps within the processes that deliver value to the customers [26]. Typically, the value steps in a process will be a small proportion of the whole system and the rest of the activities and steps are considered as waste. Activities could be divided into three types according to how much they vary: runners, repeaters and strangers [27]. The runner’s activities are those that form the majority of total activity within the process, while the repeaters are less frequent in comparison to runners. The strangers are those activities that do not have consistent patterns. In healthcare, the value stream is the care pathway that patients experience as they travel throughout the system and runners are typical patients whereas strangers are unusual patients [28,29].
Flow
Align the remaining steps into a continuous flow. Reduce product design, order processing and inventory times. Manufacture products or services at the rate they are ordered by the customer.
Pull
In pulled production, where it is not possible to deploy continuous flow, only produce as much as the customer process requires, avoiding overproduction and excess inventory. Let the customer pull the value of the company. Reverse the push methods used by companies with extensive response times that aim to convince customers that they want what the company has designed or produced. Provide what the customer wants when they need it: neither sooner nor later.
Perfection
This principle is the equivalent to turning the four previous principles into a habit of searching for continuous improvement. When following a culture of continuous improvement, the potential for improvement is always endless. In other words, lean production strives for perfection- an unreachable goal -and thus is always amenable to improvement activities. Therefore, once the value, the value chain, the flow and the pull have been established, it starts over again its quest for perfection where the ideal value is created with zero waste. At this point, only the activities that add value are present in the processes. It is important to retain progress and do everything possible to continue to improve; it is a battle for continuous improvement (kaizen).
The National Health Service (NHS) Institute for Improvement and Innovation gave examples of the significance of each principle in the context of healthcare [30]: obtaining a high standard service, no delays, best results and fewer incidents and adverse events. Thus, value comes as any activity that improves your health, welfare or experience. It is, however, necessary to define ‘customer’. In relation to the value stream, this means identifying the core actions that add value to patient care, corresponding to the optimisation of the entire circuit from beginning to end and identifying the steps with value in the care provided [30]. Identifying this value chain also means recognising activities that are NAV (i.e., are waste) and should be eliminated. Once the value stream is set, it follows the establishment of a flow, which is the principle that ensures a smooth course and minimal delays. Standardisation of processes according to best practices ensures smoother flows, freeing up room for creativity and innovation [22]. In healthcare facilities, this means minimising obstacles through fast and safe care, for example, by minimising waiting times or patient accumulation [30]. In this regard, the traditional healthcare system often has healthcare facilities function as a sort of silo in which the patient is transferred from one to wait for care in another. Lean in the healthcare context advocates the implementation of the pull system, which means provision of the service according to patient demand. Using the example of emergency service: it is usual for emergency service professionals to be obliged to search for vacancies for patients requiring hospitalisation, a task that consumes considerable resources. With the pull system, it is the inpatient service that communicates to the emergency department that there are vacancies available to receive patients who are urgently waiting to be admitted [30]. Finally, the last lean principle relates to the persistence required to achieve perfection and to be able to provide a service of excellence through continuous improvement cycles (kaizen), while meeting customer needs [31]. For the patient, this means receiving healthcare with the best results, without mistakes, on time and with no delays.
Lean and waste
The foundation of lean thinking is to amplify value for customers. This goal can be achieved in two ways: by offering the customer more AV features at the same cost and/or by reducing the NVA and therefore the cost to the consumer [32]. The elimination of waste is a central theme in the production system characterised by continuous improvement, as in lean philosophy. Muda is the Japanese term for ‘waste’: specifically, any human activity that absorbs resources but creates no value, resulting in a waste of effort, materials and time [9]. There are several types of waste and they exist everywhere. According to Womack & Jones [1], lean thinking is a powerful antidote to waste as it offers a method to do more with less (less time, less equipment, less human effort and less space). Waste can be classified, according to Ohno [10], into seven categories:
Overproduction: Manufacturing when there is no demand. This increases storage costs and extra handling of products to sell.
Inventory: Excess or lack of materials, stock in process or finished products, causing longer lead times, obsolescence, damaged products, transportation costs, storage and arrears. This waste hides problems such as lack of sales perspective, imbalance of production, late deliveries of suppliers, lack of equipment reliability, lack of synchronisation between people, equipment under repair and long setup times.
Defective products: Fix defects, reprocess defective parts or replace production and inspect equivalent to handling losses, time, effort and resources.
Transportation: Moving the item in progress, materials, parts or finished products within facilities, inside or outside stock, or between processes. Inefficient or long transport distances.
Unnecessary or inefficient process: A tool or procedure that causes unnecessary operations and/or defects. Also, when quality products are offered at a higher cost than necessary due to using unnecessarily complex and inefficient tools, and bottlenecks that arise to stop stations of work.
Wait: Periods of inactivity in which employees watch or wait for the next process, tool, input, part, etc. Alternatively, when there is no work due to lack of material, delays, interruptions or bottlenecks. This results in reduced flow and extended delivery times.
Movement: Unnecessary movements are any wasted movement employees have to make during the course of their work, such as searching for something, reaching for something or stacking parts and tools. Unnecessary walking due to poor layout is also a waste. Inefficient processing due to poor tooling and product design results in unnecessary movement and defect production.
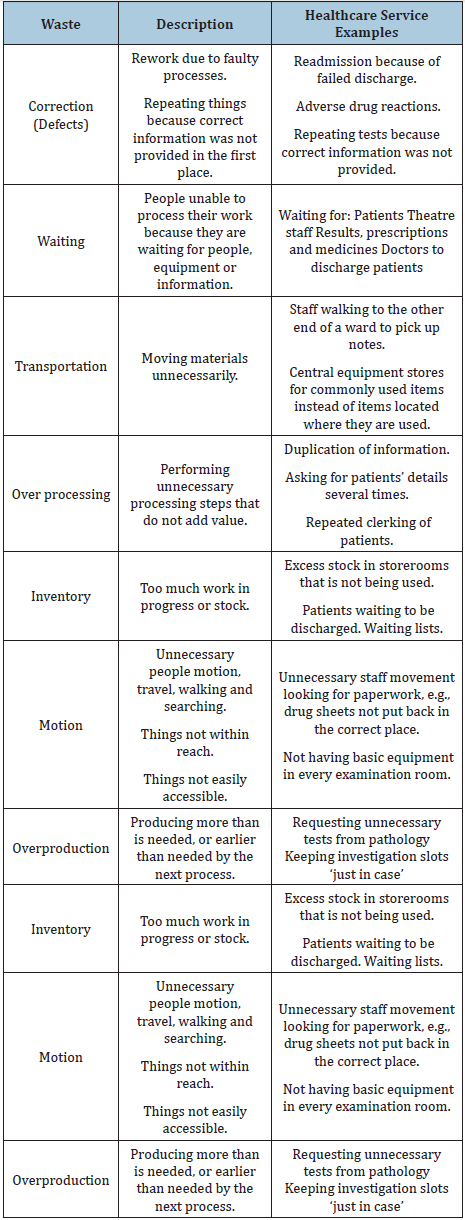
Liker [33] adds another form of waste: unused employee creativity. That is, wasted skills, ideas, time, improvements and learning opportunities by not getting involved with or listening to employees. Also Womack & Jones [1] added additional source of waste: design of products and services that do not meet customer needs. Hines & Taylor [24] conclude that the seven wastes demand greater amount of effort compared to AV. Westwood & James-Moore [30] translated the seven-manufacture waste categories to suit healthcare environments and some examples are shown in each category in Table 2.
Table 2:
Lean tools
Lean uses a set of tools and techniques that can contribute to activity evaluation and the reconfiguration of organisational processes [22]. The purpose of the activity evaluation is to review the performance of existing processes in an organisation in terms of waste, flow or the ability to add value. There are many lean tools to apply-over 100-but their application only makes sense when aligned with a correct implementation strategy [26]. In the first phase, it is important to know how to identify and quantify the problems of organisations; that is, to identify where the losses and opportunities for improvement lie, as well as to determine the root causes [34]. After this diagnosis, it is necessary to choose which improvement tools should be employed, but it is not always easy to select the best tools to address the issues [35]. Where healthcare is dealing with the management of diseases through diagnosis and treatment, lean management is about diagnosing and treating the processes’ or the system’s imperfections. Maccoby [36] indicated that for lean implementation, there is no one best way to be followed. Exploring lean tools can help healthcare organisations select the right set of tools. The challenge is to use the correct combination of these tools and methods in the correct manner by the correct personnel for the correct problem at the correct time. Consequently, tools need to be chosen and customised based on the improvement initiative requirements. The lean tools are overlapped and interconnected; the nature of improvement and the maturity level of the systems could be factors that influence the selection of the tools [16]. In healthcare, the most common lean tools used for process improvement are VSM, 5S, Kaizen and A3 [6,16,37]. A brief description of some of these tools is provided below.
Tools for process improvement
Just in time (JIT): JIT is one of the pillars of the TPS. It refers to the production and transportation of only what it is needed and in the necessary quantities. This improves efficiency and allows quick response to changes. It presupposes a level of production (Heijunka) and is based on three basic principles: pull systems, continuous flow and Takt Time [25].
Continuous Flow: Continuous flow is based on production without interruptions, where the flow of the item runs from supplier to client, directly avoiding overproduction, accumulation and waiting [25].
Pull systems: In this system, when the operation requires material, it sends a signal to the supplier operation to prompt production. The signal acts as a production order; if the signal is not sent, the production does not begin. Pull logic is used where it is not possible to perform continuous flow [1].
Lead and takt time: Lead time is the waiting time from acceptance of the order to delivery to the customer [25]. Takt time is the heartbeat of the lean system, calculated by dividing the available time by demand. Its objective is to align the production of the service to the demand.
Tools for capacity development
Jidoka: Jidoka, together with JIT, are the main pillars of the TPS [38]. Jidoka refers to the ability to stop the service provided in case of complications such as equipment malfunction, quality issues or schedule delays [1]. Anomaly sensors or collaborators within the process give the signal to halt the service. This automatically avoids defects, which in turn results in reprocessing savings [38]. Jidoka can be explained as automation with a human touch [10].
Poka-yoke: This is an error-proof system that prevents defects in processes and/or in the use of products. It allows the detection of abnormalities and provides immediate feedback. The poka-yoke allows 100% inspection through physical or mechanical control and avoids work errors such as wrong choice of input, incorrect assembly and forgetting components [38].
Andon System: This system alerts for problems within the provision of hospital services. It automates the ability to halt service when a defect arises and to continue when it is resolved [33]. This visual management tool shows the status of operations in a given area of a premises. White indicates provision of normal service, red indicates a quality problem, amber indicates lack of material and blue indicates a problem with medical tools or equipment [38].
Tools for management systems
Kaizen Event: Kaizen is an event of rapid implementation of improvements [13]. This is a short-term project, usually a lasting week, to improve a process with the aim of adding value and reducing waste. This tool emphasises the use of human effort when working in teams [1].
Root cause: This methodology focuses on solving the underlying problem instead of applying quick solutions that only deal with the immediate symptoms. One technique is to ask ‘why’ five times (referred to as ‘five whys’) [39].
Plan, do, check, Act (PDCA)
An iterative methodology for the implementation of improvements, known as the Deming cycle [40], with steps as follows:
Plan: establish a plan and expected results.
Do: implement the plan.
Check: verify that the results achieved are as expected.
Act: review and evaluate; do it again.
Tools that drive the lean healthcare transformation through level workload
Levelling of the production (Heijunka): This refers to the programming of the provision of the hospital services based on the sequence of orders in a repetitive pattern and the levelling of daily changes of all orders to correspond to long-term demand [13]. It allows for a combination of different services but maintains a continuous flow while also levelling the resources and workforce [1]. Its objective is the levelling of production and cost reduction.
Tools that drive the lean healthcare transformation through standard processes
Job standardisation: This is the establishment of precise work procedures for each of the operators in a production process [13]. Continuous improvement depends on the standardisation of work. Any task or process performed by a person must be documented, consistent and safe in order to generate products as planned. It is the clear definition of employee activity. Takt time must be known, the sequence of tasks to run within takt time and standardised materials. In this way, the levels of quality, productivity, safety and ergonomics can be sustained [41].
Tools that drive the lean healthcare transformation through visual management
Value stream map (VSM): This is a tool that consists of graphing material flows, information, etc. as the patient or other object of study traverses the flow of value. It is a simple, yet powerful tool that provides a systemic view of the value stream [13]. It allows easy identification of stream waste, renders flow decisions visible, prioritises the implementation of activities with global scope, shows the relationship between information and material flow and provides information on how production units should operate to create this optimised flow [42].
5S: The 5S program is based on five fundamental principles, the Japanese terms for each all starting with the letter ‘S’: seiri, seiton, seisou, seiketsu and shitsuke [43]. 5S, as translated into English, stands for sort, set in order, sweep and shine, standardise and sustain. The aim of the 5S tool is to provide the best work environment through a systematic approach where the employee does not waste time in searching for objects or information [30]. In this way, it achieves various objectives including creating an environment containing only necessary equipment and materials, recognising any disorganisation, reducing wasted time and avoiding potential mistakes. The 5S improves an environment by making employee lives easier, more productive and safer, consequently increasing employee self-motivation [30].
Visual management and layout: This encourages the visual display of all tools, parts, production activities and production system performance indicators so that the immediate situation can be quickly understood. An example is Kanban, a Japanese term meaning ‘cardboard’ [13]. This visual communication tool authorises the production or movement of material indicating the need for inputs. The Kanban is a visual system that, based on demand from the customer, triggers the production of a specific item in defined quantities [25]. Kanban is frequently found in pull systems. The physical layout, or simply layout, is a sequential arrangement of people, medical equipment, materials and methods in order of process, so that tasks are able to be processed in a continuous flow or in small batches. When planning the layout, decisions are made on the optimal distribution of resources and jobs to facilitate the transit of people and material.
A3 report: A3 report is considered to be a problem-solving tool where problem analyses, corrective actions, and action plans are described on an A3-size sheet of paper, preferably accompanied by graphs and value stream maps [44]. Its reports are used to promote continuous improvement, align initiatives and implement strategic measures in the organisation, processes and activities.
Figure 2: A historical overview of how lean has spread from the automotive industry to the healthcare sector is presented in (Developed by the author). Adapted from Laursen ML [54].
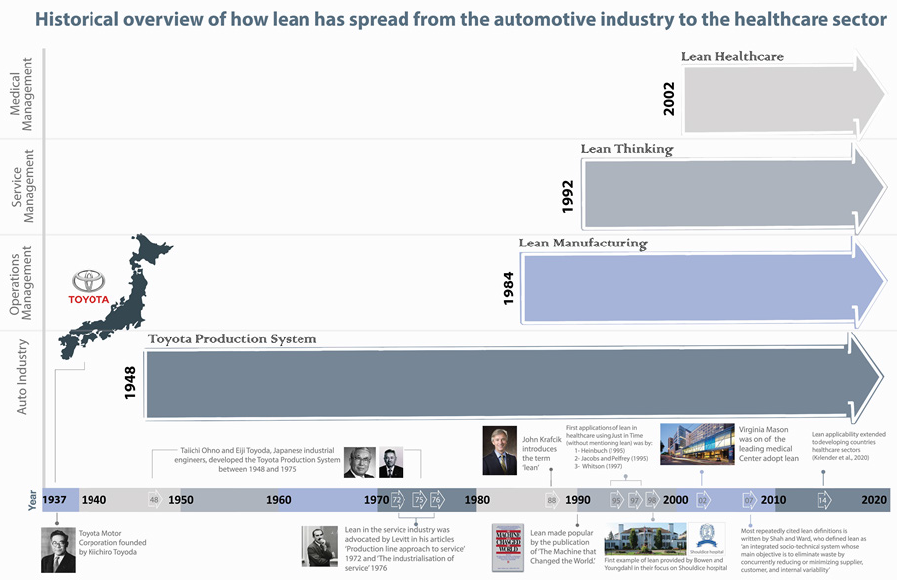
Lean from Toyota to healthcare
Lean has been implemented in many industries and organisations [17], gradually expanding to services and, since the beginning of the twenty-first century, has also been used in the healthcare sector [45]. Lean in healthcare aims to define and eliminate wasted resource by rationalising and streamlining processes to focus on flow and value creation for end consumers [46,47]. According to Brandao de Souza [47], it is not clear what the first work of implementation of lean philosophy in healthcare was. However, lean utilisation in the healthcare sector has grown rapidly in the last decade [48]. The early applications of lean in healthcare using Just in Time (without mentioning lean) was by Whitson [47]. The first example of lean provided by Bowen & Youngdahl [49] in their focus on Shouldice hospital [49]. The lean healthcare initiatives occurred in the USA in the twenty-first century [45] and in Europe from 2002 [45]. Among one ofthe first publications on this topic are the work of the British NHS [50] and research by Allway & Corbett [51] which speculate on potential gains in lean healthcare. Furthermore, the publications of Bushell & Mobley [52] and Feinstein & Grunden [53] reported gains from lean application in US hospitals. A historical overview of how lean has spread from the automotive industry to the healthcare sector is presented in Figure 2.
Lean healthcare application examples
The healthcare sector is an expanding market where it is necessary to improve quality while reducing cost [54,55]. According to Tucker & Heisler [56], concerns that drive healthcare organisations to adhere to lean principles and tools are often delays, duplicate information, rework, staff attrition, unnecessary patient and staff movements and missing equipment and supplies. Lean healthcare applications have focused on improving the efficiency, quality and safety of service delivery, improving the flow of information and communication, innovations to drive continuous improvement, redesigning the patient entry and exit process, improving access and reducing waiting time, implementation of IT solutions, medical supply chain management and policy implications ranging from the local organisational level to national health policy decisions [57]. Lean implementations appear to be an effective method to improve health organisations and there is evidence of widespread consensus on the potential of lean in healthcare [58]. Many of the published articles highlight various tangible and intangible results such as reducing waiting times, increased quality through reduction of errors, costs reduction, increased worker motivation and increased consumer satisfaction [22]. In that sense, several success stories of lean healthcare have already demonstrated numerous benefits for hospitals [58,59].
The USA, a pioneer in the implementation of lean healthcare concepts, collects a series of studies with significant results. A 2009 survey in the USA showed that 53% of hospitals are engaged in some type of continuous improvement initiative and had implemented lean to some extent [4]. The da Care Inc., Wisconsin, as an example, reports earnings 10 million dollars per year through cost reduction and productivity increase [25]. The Virginia Mason Medical Center in Seattle has adapted the lean philosophy and successfully reduced system inefficiencies and waste, increasing profit margins and decreasing mortality and the frequency of errors associated with medication [60]. According to Bush [40], a Jidoka-based alert system and source inspection led to zero patients presenting with pneumonia during an in-hospital infection. Kim & Spahlinger [61] describe the case of the University of Michigan hospital, USA, where the process was redesigned with aid of a value flow map, reducing setup and standardising activities, saving 36% of catheter positioning time.
Relevant studies on lean healthcare are also presented in the United Kingdom (UK) and Canada. The Royal Bolton NHS Foundation Trust in the UK is cited as the prime example [22]. This organisation was a pioneer institution in lean implementation to respond to a financial deficit and problems related to long waiting times for diagnosis and treatment. Through the implementation of Rapid Improvement Events, significant improvements in financial and operating results were achieved, including reducing 42% of bureaucracy to trauma service staff, cutting 38% of transport waiting times for patients with a diagnosis of hip fracture, decreasing length of stay by 33% and seeing a 36% drop in mortality rate [7]. Fillingham [62] reports that Bolton Hospitals involved more than 650 officials in Kaizen events, the 5s, the value flow map, standardised work, pulls systems and continuous flow. Another multi-million-dollar investment attempt using comprehensive lean approach was started in 2010 by the Saskatchewan Ministry of Health in Canada [63]. The goal was the transformation of the entire healthcare system to produce better health, better care, better teams and better value [64]. The Saskatchewan government claimed to accomplish saving of 125 million Canadian dollars through adopting lean [65,66].
Most healthcare providers tend to promote small lean projects, creating ‘best practice scholarships’ rather than adopting a broader organisational approach [22,47]. According to Womack & Byrne [25], when compared to other industries, hospital management has been slow to identify who the client really is. Due to the complexity of the healthcare system, processes are often designed to meet the needs of internal clients - doctors, hospitals, insurers, government and taxpayers. The author points out that it is extremely important that the value be defined by the main client: the patient. Despite these examples of success, as mentioned, there is as of yet no fully lean health organisation.
Discussion
Lean has spread rapidly from the manufacturing industry to the service industry and healthcare organisations [61]. In healthcare, concerns in safety and efficiency are more important than cost [66], and this fact could explain the reason for the 10-year delay in applying lean principles to health in comparison to other service organisations. Of the quality improvement models used in healthcare, lean has shown the largest increase in the number of publications over the past two decades [67]. Several authors underline various perspectives of lean management, and the definitions used as a part of this practice may be fluid and unclear. A lean implementation is intended to make processes more stable. One of the more favourable arguments for lean implementation is that it leads to fewer interruptions and, therefore, to greater stability. Stability starts with visual management and organisation of the 5S work environment, supported by standardisation of processes [68].
The service sector-or more precisely, the healthcare sector- is different from industry and from the production line model of Toyota, so the transition is not straightforward. We can always argue that the service sector is different from industry and that hospitals are not factories [7]. By definition, a service is a process that takes place frequently in the customer's presence and does not produce the modification of the physical properties and shape of materials, as opposed to the industrial sector [31], where the product is visible on the production line and is produced in the absence of the client. Although the lean philosophy was developed in manufacturing, Womack & Byrne [25] argue that its application is much broader. Womack & Byrne [25] mentioned that: ‘Lean thinking is not a manufacturing tactic or a cost reduction program, but rather a management strategy that is applicable to all organizations because it has to do with process improvement. All organizations - including health sector organizations-are composed of a series of processes, or sets of actions aimed at creating value for those who use or depend on them (clients/patients).'
A perfect process creates value focused on the patient's needs. It should be noted that from sector to sector things change, and that applying principles and tools in the manufacturing sector is not the same as applying them in the services sector, (i.e., healthcare). Particular attention should be paid to these differences and adaptations should be made in accordance with the characteristics of each context [69]. The root cause of the problems is usually the same for industry and healthcare. Kalong & Yusof [70] found in a literature review that all seven categories of waste in the manufacturing industry also exist in the healthcare industry. Snowball [71] claims that in terms of waste and improved efficiency, the differences between the manufacturing industry and the healthcare industry are minor: just as in the manufacturing industry, healthcare work with lean aims to create better value for the customer. However, Young & McClean [58] argue that the healthcare sector differs from other sectors in that the definitions of ‘customer’ and ‘value’ are more complicated. These concepts need to be clear to determine the steps required in the improvement work. Other major differences are that healthcare is usually not profit-driven and that it is difficult to measure value because the ultimate goal is to cure patients and prevent diseases. Examples of value for the patient can be short waiting times, good service and high quality treatments.
The researcher’s reflection based on literature review is that lean could be described simply as a philosophy that consists of a set of tools and principles to improve the system in a continuous manner with an aim to reach perfection. This method of thinking can function as a framework for the implementation of a programme change within the organisational setting. Lean emphasises on maximising value by minimising waste in energy, time and resources [25]. As a result, lean can create a culture in the healthcare context characterised by an increase in the satisfaction of patients and stakeholders by allowing all areas to eliminate waste and improve service quality [72]. Conducting research with rigorous methodology in the healthcare system is essential, while still acknowledging that there is no agreed-upon definition of lean management [33,73].
Conclusion
Since the introduction of lean thinking to the healthcare sector, that has been little effort to provide a comprehensive historical overview of how lean thinking has transferred and spread from Toyota manufacturing to healthcare. This paper aims to fill that gap. It explains the origin of lean, how it is defined, the main tools, concepts, and principles behind it and provides some lean healthcare examples as well as discussing the differences between manufacturing and the healthcare system. Lean originated from Toyota in the 1940s due to the need to increase production efficiency, notably by reducing waste. Since then, lean has been implemented in many industries and organisations, gradually expanding to services and, since the beginning of the twenty-first century, has also been used in the healthcare sector. Even then, lean alone did not have an agreed-upon definition within the literature; any agreement was on the potential of lean thinking in the healthcare sector. Several lean tools and techniques were used by different organisations, mostly to reduce or eliminate waste. Some of the leading examples of lean healthcare services are Virginia Mason Medical Centre (USA), Theda Care (Wisconsin), Bolton Hospital (England) and the Saskatchewan health system (Canada). Even with the encouraging success from adopting lean as a management approach, challenges continue to arise. The service sector differs from industry in that hospitals are not factories, so any transitions are not straightforward. The lean journey is just starting in the healthcare sector, and more is effort required to appreciate its full potential.
References
- Womack JP, Jones DT (2003) Lean thinking: Banish waste and create wealth in your corporation. Simon & Schuster, London.
- Onetto M (2014) When Toyota met e-commerce: Lean at amazon. Mckinsey Quarterly, USA.
- Distelhorst GJ, Hainmueller, Locke RM (2016) Does lean improve labor standards? Management and social performance in the Nike supply chain. Management Science 63(3): 707-728.
- Holden RJ (2011) Lean thinking in emergency departments: A critical review. Ann Emerg Med 57(3): 265-278.
- Toussaint JS, Berry LL (2013) The promise of lean in health care. Mayo Clinic Proceedings 88(1): 74-82.
- Lawal AK, Rotter T, Kinsman L, Sari N, Harrison L, et al. (2014) Lean management in health care: definition, concepts, methodology and effects reported (systematic review protocol). Systematic Reviews 3(1): 103.
- McIntosh B, Sheppy B, Cohen I (2014) Illusion or delusion-Lean management in the health sector. International Journal of Health Care Quality Assurance 27(6): 482-492.
- Monden Y (2011) Toyota production system: an integrated approach to just-in-time. Productivity Press, USA.
- Womack JP, Jones DT, Roos D (1988) Machine that changed the world. Simon and Schuster, USA.
- Ohno T (1988) Toyota production system: beyond large-scale production. CRC Press, USA.
- Liker JK, Morgan JM (2006) The Toyota way in services: the case of lean product development. Academy of Management Perspectives 20(2): 5-20.
- Emiliani ML (2006) Origins of lean management in America: The role of connecticut businesses. Journal of Management History 12(2): 167-184.
- Graban M (2018) Lean hospitals: improving quality, patient safety, and employee engagement. Productivity Press, USA.
- Liker JK (2008) Toyota culture. McGraw-Hill Publishing, USA.
- Krafcik JF (1988) Triumph of the lean production system. MIT Sloan Management Review 30(1): 41.
- Pettersen J, Dahlgaard (2009) Defining lean production: Some conceptual and practical issues. The TQM Journal 21(2): 127-142.
- McIntosh B, Cookson G (2012) Lean management in the NHS: Fad or panacea. British Journal of Healthcare Management 18(3): 130-135.
- Simon RW, Canacari EG (2012) A practical guide to applying lean tools and management principles to health care improvement projects. AORN Journal 95(1): 85-103.
- Shah R, Ward PT (2007) Defining and developing measures of lean production. Journal of Operations Management 25(4): 785-805.
- Scoville R, Little K (2014) Comparing lean and quality improvement. IHI White Paper, Institute for Healthcare Improvement, Massachusetts, Cambridge, USA.
- Mann D (2009) The missing link: Lean leadership. Frontiers of Health Services Management 26(1): 15.
- Radnor ZJ, Holweg M, Waring J (2012) Lean in healthcare: The unfilled promise? Social Science & Medicine 74(3): 364-371.
- Womack JP, Jones DT (1996) Beyond Toyota: how to root out waste and pursue perfection, USA.
- Hines P, Taylor D (2000) Going lean. Cardiff, UK: Lean enterprise research centre cardiff business school, pp. 3-43.
- Womack JP (2005) Going lean in health care. Institute for Healthcare Improvement, Cambridge, USA.
- Rother M, Shookv J (2003) Learning to see: Value stream mapping to add value and eliminate muda. Lean Enterprise Institute, USA.
- Eaton M (2013) The Lean Practitioner's Handbook. Kogan Page Publishers, UK.
- Balushi S (2014) Readiness factors for lean implementation in healthcare settings--a literature review. J Health Organ Manag 28(2): 135-153.
- Joosten T, Bongers I, Janssen R (2009) Application of lean thinking to health care: issues and observations. International Journal for Quality in Health Care 21(5): 341-347.
- Westwood N, James M, Cooke M (2007) Going Lean in the NHS. NHS Institute for Innovation and Improvement, UK.
- Asnan R, Nordin N, Othman SN (2015) Managing change on lean implementation in service sector. Procedia-Social and Behavioral Sciences 211: 313-319.
- Hines P, Holweg M (2004) Rich, Learning to evolve: A review of contemporary lean thinking. International Journal of Operations & Production Management 24(10): 994-1011.
- Liker JK (2004) The Toyota way: 14 management principles from the world's greatest manufacturer. McGraw-Hill, New York, USA.
- Machado VC, Leitner U (2010) Lean tools and lean transformation process in health care. International Journal of Management Science and Engineering Management 5(5): 383-392.
- Langstrand, J, Drotz E (2016) The rhetoric and reality of Lean: a multiple case study. Total Quality Management & Business Excellence 27(3-4): 398-412.
- Maccoby M (1997) Is there a best way to build a car? Harvard Business Review 75(6): 161-167.
- Mazzocato P (2012) How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children's hospital, Stockholm, Sweden. BMC health services research 12(1): 28.
- Grout JR (2010) Toussaint, mistake-proofing healthcare: Why stopping processes may be a good start. Business Horizons 53(2): 149-156.
- Iedema RM (2006) A root cause analysis of clinical error: confronting the disjunction between formal rules and situated clinical activity. Social Science & Medicine 63(5): 1201-1212.
- Bush RW (2007) Reducing waste in US health care systems. Jama 297(8): 871-874.
- Bowerman J, Fillingham D (2007) Can lean save lives? Leadership in Health Services, UK.
- Teichgräber UK, Bucourt M (2012) Applying value stream mapping techniques to eliminate non-value-added waste for the procurement of endovascular stents. European Journal of Radiology 81(1): e47-e52.
- Kanamori (2015) Implementation of 5S management method for lean healthcare at a health center in Senegal: a qualitative study of staff perception. Glob Health Action 8: 27256.
- Harmon P (2019) Business process change: a business process management guide for managers and process professionals. Morgan Kaufmann, USA.
- Kadarova, J, Demecko M (2016) New approaches in lean management. Procedia Economics and Finance 39: 11-16.
- Kollberg B, Dahlgaard JJ, Brehmer PO (2007) Measuring lean initiatives in health care services: Issues and findings. International Journal of Productivity and Performance Management 56(1): 7-24.
- Brandao de Souza L (2009) Trends and approaches in lean healthcare. Leadership in Health Services 22(2): 121-139.
- Nicola B, Zoe R (2013) Evaluating Lean in healthcare. International Journal of Health Care Quality Assurance 26(3): 220-235.
- Bowen DE, Youngdahl WE (1998) “Lean” service: in defense of a production‐line approach. International Journal of Service Industry Management, USA.
- NHS (2002) Modernisation Agency Ideal Design of Emergency Access (IDEA) Programme NHS: UK.
- Allway M, Corbett S (2002) Shifting to lean service: Stealing a page from manufacturers' playbooks. Journal of Organizational Excellence 21(2): 45-54.
- Bushell S, Mobley J, Shelest B (2002) Discovering lean thinking at progressive healthcare. Journal for Quality and Participation, p. 20-25.
- Feinstein KW, Grunden N, Harrison EI (2002) A region addresses patient safety. American Journal of Infection Control 30(4): 248-251.
- Laursen ML, Gertsen F, Johansen J (2003) Applying lean thinking in hospitals-exploring implementation difficulties in 3rd . International Conference on the Management of Healthcare and Medical Technology, USA.
- Kelendar H, Faisal M, Mohammed MA (2020) The need for lean thinking in the Kuwaiti healthcare system. Health Science Journal 14(2:700): 1-6.
- Tucker AL, Heisler WS, Janisse LD (2013) Organizational factors that contribute to operational failures in hospitals. Harvard Business School Working Paper, pp. 14-23.
- Sloan T (2014) Lean in healthcare–history and recent developments. Journal of Health Organization and Management 28(2): 130-134.
- Young TP, McClean SI (2008) A critical look at lean thinking in healthcare. Qual Saf Health Care 17(5): 382-386.
- Mazzocato P (2010) Lean thinking in healthcare: A realist review of the literature. Quality & Safety in Health Care 19(5): 376-382.
- Nelson P, Leppa CJ (2007) Creating an environment for caring using lean principles of the virginia mason production system. Journal of Nursing Administration 37(6): 287-294.
- Kim CS (2006) Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 1(3): 191-199.
- Fillingham D (2007) Can lean save lives? Leadership in Health Services 20(4): 231-241.
- Sari N (2017) An economic analysis of a system wide Lean approach: cost estimations for the implementation of Lean in the Saskatchewan healthcare system for 2012-2014. BMC Health Services Research 17(1): 523.
- Kinsman L (2014) Largest lean transformation in the world': The implementation and evaluation of lean in saskatchewan healthcare. Healthcare Quarterly 17(2): 29-32.
- Cohen RI (2018) Lean methodology in health care. Chest 54: 1448-1454.
- Patwardhan A, Patwardhan D (2008) Business process re-engineering–saviour or just another fad? One UK health care perspective. International Journal of Health Care Quality Assurance 21(3): 289-296.
- Sun GH (2014) Health care quality improvement publication trends. American Journal of Medical Quality: The Official Journal of the American College of Medical Quality 29(5): 403-407.
- Duggan KJ (2007) Lean Production simplified: A plain-language guide to the world's most powerful production system. Productivity Press, USA.
- Kelendar H, Mohammed MA (2019) Hospital bed occupancy and utilisation: Is Kuwait on the right track? Journal of Hospital & Medical Management 5(2:3): 1-11.
- Kalong NA, Yusof MM (2013) Understanding waste for lean health information systems: A Preliminary review. Studies in Health Technology & Informatics 192: 749-753.
- Snowball A (2012) Turning the NHS into a lean, mean, healthcare machine. The Health Service Journal 122(6308): 18-21.
- Dahlgaard JJ, Pettersen J, Dahlgaard-Park SM (2011) Quality and lean health care: A system for assessing and improving the health of healthcare organisations. Total Quality Management & Business Excellence 22(6): 673-689.
- Graban M (2011) Lean hospitals: improving quality, patient safety, and employee satisfaction. CRC Press, USA.
© 2020 Hisham Kelendar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






