- Submissions

Full Text
Research in Medical & Engineering Sciences
Schizophrenia and it’s Protection against Lung Cancer: A Genetic Explanation
Alex Soloway*, Andrew Spaedy, Ramon Solhkhah, Stacy Doumas and Theodor Rais
Department of Mechanical Engineering, USA
*Corresponding author: Alex Soloway, Department of Mechanical Engineering, USA
Submission: February 04, 2019; Published: February 26, 2019

ISSN: 2576-8816Volume7 Issue4
Abstract
Introduction/Review: Although individuals with schizophrenia have a markedly higher than average rate of tobacco smoking, multiple studies have shown that their risk of lung cancer is lower than that of the general population [1-3]. There are both environmental and genetic factors that form possible explanations for the protective link between these two conditions. This study aims to shed light on the genetic aspect of this relationship.
Methodology: Two unique search queries were run through OMIM (Online Mendelian Inheritance in Man) to obtain the known genetic links of both schizophrenia and lung cancer. These results were then crossmatched. One of the common genes, the SLC6A3 gene, was selected for further research. Multiple electronic databases were then searched with results going back over the past 37 years (1981 through 2018). Per our inclusion criteria, the abstract sections as well as the titles were sorted independently by two authors. Articles were sorted into relevant and irrelevant categories, with irrelevant articles being discarded. The full text was obtained for articles deemed to be relevant and were then reviewed by both authors.
Result: One study proved a positive correlation between the DAT1 A/T polymorphism and schizophrenia among a population of Iranian males [4]. Evidence from various studies suggests that dopamine possesses tumor inhibiting effects [5-8]. The expression of DAT1 was found in both the brain and the lungs [9-11].
Conclusion: The SLC6A3 encoded DAT1 may be the source of the protective effect against lung cancer that patients with schizophrenia appear to possess. Although preliminary findings have been positive, additional high-quality research in the area of study will be needed to further delineate the relationship between the two.
Keywords: Schizophrenia; Dopamine; Lung cancer; DAT1; Dopamine Transporter gene; Cigarette smoking
Abbreviation: DAT1: Dopamine Transporter1; VPF/VEGF: Vascular Permeability Factor/ Vascular Endothelial Growth Factor; D2R: Dopamine D2 Receptor; HUVEC: Human Umbilical Vein Endothelial Cell
Introduction
Schizophrenia is a chronic mental health disorder that results in a profound burdon on the both the individual affected and the greater society [12]. Affected persons with the condition have a decreased life span by approximately 20-25 years [13]. Cancer is the second leading cause of death both globally and in the developed world. Among the various types, lung cancer ranks first in mortality [14]. It is no secret that exposure to cigarette smoke is one of the leading risk factors for the development of the condition. In fact, smoking cigarettes has been associated with a 15-30-fold increase of the subsequent development of lung cancer [15]. Patients with schizophrenia have a well-documented history of significantly higher than average rates of smoking cigarettes. At first glance, a patient population with tobacco smoking rates twice that of the general population would think to be correlated with higher than average rates of pulmonary neoplasia. Interestingly, despite their increased exposure, patients with schizophrenia have been found to have a lower overall rate of lung cancer than that of the general population [1-3].
The connection between lung cancer and schizophrenia is one that is straightforward. Like most neoplastic processes, a combination of both environmental and genetic factors likely plays a role in the ultimate development of the condition. Multiple reasonable environmental protective factors have been identified [16]. However, the question of which-if any-genetic element that links the two conditions remains to be answered. The goal of this review was to attempt to gain clarity on this topic.
Methodology
Search strategy
Initially a search for genes was carried out on OMIM with the search keyword of “schizophrenia.” The search results returned 229 unique genes. A second search was performed with key phrase “‘lung cancer’” which yielded 313 unique genes. After crossmatching the results from the two search queries, seven genes were found to be common between the two conditions. One of these seven, the SLC6A3 gene - which codes for the dopamine transporter (DAT1) - was chosen to be the focus for our study. A systematic search of the following databases was carried out: PubMed, ask MEDLINE, Google Scholar. The following keywords were used, as well as their combinations: “schizophrenia,” “lung cancer,” “DAT1.” Our search consisted of studies which were primary and secondary in nature. It was limited to publications ranging from 1988 through 2018.
Hits received from the databases were as follows: PubMed (31), ask MEDLINE (77), Google Scholar (172). Per the inclusion criteria, two authors independently examined the titles and abstract sections of the articles that were obtained in the searches. Articles found to be irrelevant were thrown out from the study. The full texts of the remaining studies were obtained by the authors and were, once again, reviewed independently and were sorted into relevant and irrelevant categories. Studies that were agreed upon as relevant were included in the study. Of the total article pool containing 280 articles, 20 were agreed upon and selected as relevant and included in our study.
Result/ Overview of the Studies Exploring the Relationship Between Schizophrenia and Lung Cancer
Results of gene search
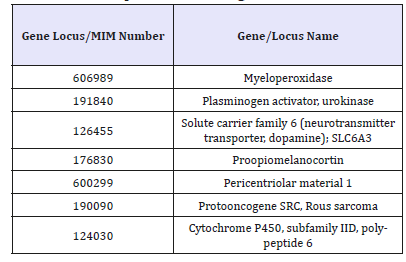
As was stated above, a system wide search was performed on OMIM to find the genes that are associated with both Schizophrenia and Lung Cancer (Table 1).
Table 1:As was stated above, a system wide search was performed on OMIM to find the genes that are associated with both Schizophrenia and Lung Cancer.
Patients with schizophrenia have a lower incidence of lung cancer
A systematic review and meta-analysis [17] of the prevalence of lung cancer in patients with schizophrenia looked at 383 articles pertaining to “schizophrenia,” “lung cancer,” and/or “lung neoplasms.” Thirty-three articles were included for further review and analysis. The study found that there is a lower overall prevalence of lung cancer at 3.84 per 1,000 persons (95% CI: 2.76 to 4.91, p< 0.001) and a lower risk of developing lung cancer (RR: 0.528, 95% CI: 0.330-0.845) in patients with schizophrenia.
Another study [10] compared the incidence of malignant neoplasms amongst schizophrenics with that of the local general population. The study identified 2,976 male and 3,202 female patients with schizophrenia in Aarhus, Denmark from 1957 to 1980. The results indicate that the incidence of lung cancer (SIR=0.58, CL 0.40-0.81) is significantly reduced in both male and female schizophrenic patients in Denmark. A cohort analysis [18] of linked hospital and death records in England was used to compare cancer rates in people with schizophrenia with a reference cohort. A total of 9,649 patients with schizophrenia from 1963 to 1999 were compared with a cohort of nearly 600,000. The study found that the risk of lung cancer was non-significantly elevated in patients with schizophrenia (rate ratio 1.18, 95% CI: 0.94-1.45) when compared to the reference cohort. There is no data on the smoking history of the patients analyzed.
Schizophrenia, the DAT1 and SLC6A3 gene
The dopamine transporter (DAT), encoded by the SLC6A3 gene, functions to reuptake dopamine in the neuronal synapse [19]. Dysfunctions of this gene have been implicated in conditions such as Tourette syndrome, attention-deficit/hyperactivity disorder, parkinsonism, and substance use [20]. While the above conditions and their relation to the DAT1 have been discussed in multiple publications, scholarly articles on its connection to schizophrenia are thin.
The first study that suggested a potential link to schizophrenia was done by Grios et al. [21] who experimentally created mice that were homozygous-null for the DAT1. These mice exhibited spontaneous hyperlocomotion which was observed despite significant adaptive changes being put in place, including decreased neurotransmitter concentrations and receptor levels. In these studies, dopamine remained in the extracellular space for a minimum of one hundred times longer than normal. Interestingly, these mice were noted to have similar behaviors that are seen in the positive symptoms of schizophrenia [21].
The DAT1’s relation to schizophrenia was once again looked at in 2004 by Khodayari et al. [5] who recognized a possible link between schizophrenia and the DAT1 gene via case control analysis of the DAT1’s gene core promoter polymorphism -67A/T. The DAT1 A/T polymorphism was found to be significantly increased in patients with schizophrenia [5].
Dopamine’s tumor inhibiting effect
Schizophrenia patients have a lower than average risk of developing lung cancer as compared to their non-schizophrenia counterparts. Dopamine provides an array of different functions in various unique tissues throughout the body. Its receptors are found in both alveolar epithelial cells and human lung tumours and functions to inhibit cellular proliferation. This is achieved via selective inhibition of vascular permeability and angiogenesis via vascular endothelial growth factor (VPF/VEGF). Campa et al was able to show that dopamine polymorphisms that result in increased dopamine bioavailability are inversely correlated with the incidence of non-small cell lung cancer [5].
Dopamine D2 receptor (D2R) agonists’ potential influences on lung cancer has also been studied. Hoepper et al found that D2R agonists were able to have an inhibiting effect in syngeneic as well as human xenograft orthotopic murine models. This was shown to be via tumor angiogenesis inhibition, by means of VEGFR-2- mediated signal nullification, as well as reduction of myeloid derived suppressor cells [6].
Xiaoyuan et al also experimentally studied the effects of D2R agonists effects on lung cancer. They were able to show that quinpirole, a selective D2 and D3 receptor agonist, resulted in inhibition of non-small cell lung cancer tumor growth (p< 0.0001) through inhibition of NF-κB signaling pathway [7]. These studies strengthen the previously published findings, by Baus et al. who found that angiogenesis - via VEGF‐induced HUVEC (human umbilical vein endothelial cell) proliferation and migrationmicro vessel density, permeability, and ultimately the growth of malignant tumors in murine models were the result of peripheral dopaminergic nerve ablation [8].
Location/expression of DAT1
Studies suggests that dopamine transporter (DAT) is expressed in the lungs of humans and animals. One study sought to investigate which organs in rats had a distribution of dopamine transporter [9]. It did so with an immunohistochemical method. The results of this study demonstrated staining of DAT in the central nervous system, anterior pituitary, Auerbach’s nervous system, Meissner’s nervous system of the stomach, small intestine and colon, adrenal medulla, and the lungs. The results suggest that DAT plays an important role in the dopaminergic system [22]. A double-blind, placebo-controlled, crossover study used imaging with 123I-FP-CIT to detect DAT binding in the lungs [10]. Lung uptake of 123I-FPCIT was statistically significantly lower after paroxetine intake (0.56+0.35 %IA) when compared to intake of placebo (0.97+0.44 %IA). This is the first study to show that 123I-FP-CIT binds in vivo in humans not only to DATs but also to central SERTs and SERTs in lung tissue.
Expression of DAT in the brain has been well documented by numerous studies. Chinaglia et al. [11] used quantitative ligand autoradiography to investigate dopamine transporter sites in basal ganglia of patients affected by multiple disorders. In patients suffering from schizophrenia the density of dopamine uptake sites in the basal ganglia was slightly reduced. A study conducted by Laasko et al. [12] used positron emission tomography and [G] CFT, a marker of dopamine nerve terminals, to look at striatal DAT density. Their results suggest a possible decreased expression of DAT in a subset of chronic schizophrenic patients. Markota et al. [13] measured the density of axon varicosities immunoreactive for DAT throughout the amygdala. They found statistically significant decreased DAT-immunoreactive varicosities in various locations of the amygdala [23].
Discussion
As discussed above, many studies have shown that patients with schizophrenia have a lower incidence of lung cancer when compared with the general population. Seven genes were found to be associated with both schizophrenia and lung cancer. The SLC6A3 gene associated with the expression of DAT provides the strongest potential link between the symptoms of schizophrenia and protective factors for lung cancer [24].
The Dopamine Hypothesis has long suggested that the symptoms of schizophrenia are due to an overactivation of dopamine receptors. The fact that antipsychotics successfully reduce psychotic symptoms by blocking dopamine receptors support this hypothesis. DAT functions to reuptake dopamine from the synaptic cleft; it is the main mechanism through which dopamine is removed from the synapses. Studies done on both mice and humans have proposed decreased DAT expression in the brain as a cause for symptoms of schizophrenia because of the increased dopamine in the synaptic cleft. The research has shown that DAT is not only expressed in the brain but, also in the lungs as well as other parts of the body. Decreased DAT expression in the lungs would function in a similar manner, allowing dopamine more time to exert its anti-tumor effects for longer periods of time.
Conclusion
The possibility for schizophrenia acting as a protective factor against lung cancer has long been discussed but lacked scholarly research. This review has helped to highlight the small, but growing body of evidence supporting the possibility of a causative, genetic link. While preliminary studies on the topic have yielded promising data, a more substantial body of research is needed before a more definitive conclusion is able to be drawn. With the growing push towards individualized medicine, this could hold valuable promise for future therapeutic intervention in the form of novel pharmacologic and gene editing therapy; a valuable prospect for patients who are suffering from this lifelong taxing condition.
Disclosure
The authors of this article have nothing to disclose that could be seen as a potential conflict of interest. No funding was given for this study.
Acknowledgement
The authors would like to thank the Psychiatric faculty and staff of Hackensack Meridian Health system for their assistance in the writing of this article
References
- Craig T, Lin S (1981) Cancer and mental illness. Comprehensive Psychiatry 22(4): 404-410.
- Dalton S, Mellemkjær L, Thomassen L, Mortensen P, Johansen C (2005) Risk for cancer in a cohort of patients hospitalized for schizophrenia in Denmark. Schizophrenia Research 75(2-3): 315-324.
- Gulbinat W, Dupont A, Jablensky A, Jensen O, Marsella A, et al. (1992) Cancer incidence of schizophrenic patients results of record linkage studies in three countries. British Journal of Psychiatry 161(S18): 75-83.
- Campa D, Zienolddiny S, Lind H, Ryberg D, Skaug V, et al. (2007) Polymorphisms of dopamine receptor/transporter genes and risk of non-small cell lung cancer. Lung Cancer 56(1): 17-23.
- Khodayari N, Garshasbi M, Fadai F, Rahimi A, Hafizi L, et al. (2004) Association of the dopamine transporter gene (DAT1) core promoter polymorphism? 67T variant with schizophrenia. American J Medical Genetics 129B(1): 10-12.
- Hoeppner L, Wang Y, Sharma A, Javeed N, Van Keulen V, et al. (2014) Dopamine D2 receptor agonists inhibit lung cancer progression by reducing angiogenesis and tumor infiltrating myeloid derived suppressor cells. Mol Oncol 9(1): 270-281.
- Wu X, Zhang C, Zhao W (2016) Activation of dopamine receptor D2 to inhibit non-small cell lung cancer growth in vivo. J Clinical Oncology 34(15_suppl): e23197.
- Basu S, Sarkar C, Chakroborty D, Nagy J, Mitra R, et al. (2004) Ablation of peripheral dopaminergic nerves stimulates malignant tumor growth by inducing vascular permeability factor/vascular endothelial growth factor-mediated angiogenesis. Cancer Research 64(16): 5551-5555.
- Mitsuma T, Rhue N, Hirooka Y, Kayama M, Wago T, et al. (1998) Distribution of dopamine transporter in the rat: An immunohistochemical study. Endocrine Regulations 32: 71-75.
- Booij J, de Jong J, de Bruin K, Knol R, de Win M, et al. (2007) Quantification of striatal dopamine transporters with 123I-FP-CIT SPECT is influenced by the selective serotonin reuptake inhibitor paroxetine: A double-blind, placebo-controlled, crossover study in healthy control subjects. The J Nuclear Medicine 48(3): 359-366.
- Chinaglia G, Alvarez F, Probst A, Palacios J (1992) Mesostriatal and mesolimbic dopamine uptake binding sites are reduced in Parkinson’s disease and progressive supranuclear palsy: A quantitative autoradiographic study using [3H] mazindol. Neuroscience 49(2): 317- 327.
- Laakso A, Bergman J, Haaparanta M, Vilkman H, Solin O, et al. (2001) Decreased striatal dopamine transporter binding in vivo in chronic schizophrenia. Schizophrenia Research 52(1-2): 115-120.
- Markota M, Sin J, Pantazopoulos H, Jonilionis R, Berretta S (2014) Reduced dopamine transporter expression in the amygdala of subjects diagnosed with Schizophrenia. Schizophr Bull 40(5): 984-991.
- Chaiyakunapruk N, Chong H, Teoh S, Wu D, Kotirum S, et al. (2016) Global economic burden of schizophrenia: a systematic review. Neuropsychiatric Disease and Treatment 12: 357.
- Kilbourne A, Morden N, Austin K, Ilgen M, McCarthy J, et al. (2009) Excess heart-disease-related mortality in a national study of patients with mental disorders: identifying modifiable risk factors. General Hospital Psychiatry 31(6): 555-563.
- (2018) Cancer. WHO, Switzerland.
- (2019) What are the risk factors for lung cancer? Lung Cancer, USA.
- Lichtermann D, Ekelund J, Pukkala E, Tanskanen A, Lönnqvist J (2001) Incidence of cancer among persons with schizophrenia and their relatives. Arch Gen Psychiatry 58(6): 573-578.
- Crisafio, Anthony (2017) The prevalence of lung cancer in schizophrenia: A systematic review and meta-analysis.
- Goldacre M, Kurina L, Wotton C, Yeates D, Seagroatt V (2005) Schizophrenia and cancer: an epidemiological study. British J Psychiatry 187(04): 334-338.
- (2019) Solute carrier family 6 (Neurotransmitter transporter, dopamine), member 3; SLC6A3. OMIM, USA.
- Giros B, Jaber M, Jones S, Wightman R, Caron M (1996) Hyperlocomotion and indifference to cocaine and amphetamine in mice lacking the dopamine transporter. Nature 379(6566): 606-612.
- Mortensen P (1989) The incidence of cancer in schizophrenic patients. J Epidemiology Community Health 43(1): 43-47.
- Vandenbergh D, Persico A, Hawkins A, Griffin C, Li X, et al. (1992) Human dopamine transporter gene (DAT1) maps to chromosome 5p15.3 and displays a VNTR. Genomics 14(4): 1104-1106.
© 2019 Alex Soloway. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






