- Submissions

Full Text
Research in Medical & Engineering Sciences
Left Sided Laparoscopic Cholecystectomy: Case Report and Literature Review
Ifrat IB1*, Gultakin HB2, Sultan BA3, Hasan IB4, Mohammad FL5 and Ilkin IB6
1 Consultant General and Laparoscopic Surgeon, Saudi Arabia
2 Specialist registrar General Surgery and Intensive Care, Saudi Arabia
3 Consultant General and Laparoscopic Surgeon, Saudi Arabia
4 Slovak Medical University, Slovakia
5 Specialist Registrar, Imam Abdulrahman, Saudi Arabia
6 Slovak Medical University, Europe
*Corresponding author: Ifrat Isa Bakirov, Consultant General and Laparoscopic Surgeon, Saudi Arabia
Submission: February 04, 2019; Published: February 22, 2019

ISSN: 2576-8816Volume7 Issue4
Abstract
Situs inversus totalis is the complete mirror image reversal of the thoracic and abdominal organs. It is a rare condition and can be challenging for diagnoses and treatment of surgical diseases like acute appendicitis, acute cholecystitis or gall stone disease, splenic infarction, cysts, abdominal trauma et c. Laparoscopic management of such patients is much more difficult due to ergonometric problems and need rearrangement of operating room and additional facility may required. Here we are reporting the case of laparoscopic cholecystectomy in a patient with situs inversus totalis, who managed successfully as a day case surgery.
Literature Review
Marco Severino first recognized dextrocardia in 1643. More than a century later, Matthew Baillie described the complete mirror-image reversal of the thoracic and abdominal organs in situs inversus. Situs inversus is present in 0.01% of the population [1]. Situs inversus viscerum can be either total or partial. Situs inversus totalis (SIT), also called mirror-image dextrocardia, is characterized by the presence of the heart and stomach on the right side of the midline while the liver and gallbladder are present on the left side [2].
Gall Stone Disease and its complications, like acute and chronic cholecystitis, mucocele, empyema, choledocholithiasis, obstructive jaundice, biliary pancreatitis are very common in Saudi Arabia. Laparoscopic Cholecystectomy is one of the most commonly performed elective procedures here. Despite of that truly left sided gall bladder (GB) is extremely rare and we faced once only within our long surgical experience in Saudi Arabia. While revising internet literature we found totally 40 cases of open cholecystectomy - before laparoscopic era [2] and 1 case in 2008 [3] and about 50 cases of laparoscopic cholecystectomy in patients with SIT [4]. In 1991, Campos and Sipes [5] reported the first successful laparoscopic cholecystectomy in a patient with situs inversus with a symptomatic gallstone. From Saudi Arabia 2 cases of laparoscopic cholecystectomy in patients with SIT reported. One of them is 29 years old Sudanese female patient [6], other one is Saudi national 40 years old male patient [7]. No conversion to open surgery among all reported cases. Majority of reported cases are from India. Since 2011 also few cases of single incision laparoscopic cholecystectomy in patients with SIT reported from Turkey [8], Japan [9] and Republic of Korea [10].
All patients preoperatively investigated by Ultrasound, CT and MRCP and no abnormalities found in the anatomy of liver and biliary tree. In Thailand on 2017 first time Rungsakulkij N and Tangtawee P used intraoperative fluorescence cholangiography during laparoscopic cholecystectomy in patient with SIT [11] to identify extra hepatic biliary strictures.
Case Report
Our patient is 54 years old Saudi Male (MRN 62644) known case of dextrocardia came to surgery clinic with complaints of pain in epigastrium and left hypochondrium, related to fatty food and radiating to left shoulder, since last 1 year, which is forcing patient to receive analgesics and spasmodic. Clinical examination revealed morbid obesity with BMI 45, mild tenderness in epigastrium and left hypochondrium with no rigidity, no rebound tenderness and negative Merphy’s sign. Routine ultrasound abdomen found left sided liver which is mildly enlarged and bright, suggestive of fatty changes, left sided GB containing small stones of 4-5mm in size (Figure 1 & 2). No other abnormalities detected. Portal vein, common bile duct other intra and extrahepatic biliary structures were within normal limits. Spleen was on left side but sonographically normal. Pancreas, both kidneys, urinary bladder found to be normal. We attended ultrasound study with radiologist, and we informed him that patient is known case of dextrocardia. Radiologist did initially usual ultrasound examination of abdomen and after that he did imaging of gall bladder while holding probe in 180-degree reversed position. According to radiologist it helped him to get usual position of GB and make easier to be orientated in anatomy of biliary system.
Figure 1:Ultrasound study of liver in patient with SIT.
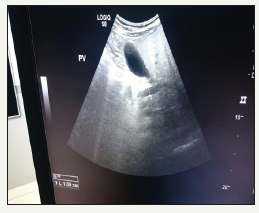
Figure 2:Ultrasound study of GB in patient with SIT.

Patient routinely prepared for surgery all blood investigations are found to be normal. Chest X ray confirmed dextraposition of heart (Figure 3). ECG done with leads placed as mirror image of routine practice and patient reviewed preoperatively by anaesthetist and classified as ASA 2. Patient scheduled for elective laparoscopic cholecystectomy as a day case under general anaesthesia. Consent obtained for anaesthesia, laparoscopic vs open cholecystectomy possible cholangiography, for photo and video imaging. Entire surgery recorded. Patient and surgeon stayed on the right side of patient, monitor placed on the left side, near left shoulder. Pneumoperitoneum done by Werres needle at subumbilical area after making 5mm skin incision. From same incision 5mm visiport with 5mm 30-degree scope inserted- which is standard for us most of laparoscopic procedures. Revision done, surgeon and assistant oriented in anatomy of abdominal cavity again confirmed that liver and GB in the left upper abdomen. Found multiple adhesions between liver and diaphragm and part of greater omentum was adherent to anterior abdominal wall (Figure 4).
Figure 3:Chest X ray showing dextrocardia patient with SIT.

Figure 4:Liver and GB on the left upper abdomen in patient with SIT. Adhesions between liver and diaphragm.
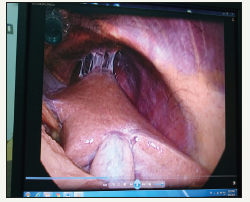
Figure 5:Left sided laparoscopic cholecystectomy. Dissecting adhesions between greater omentum and GB.

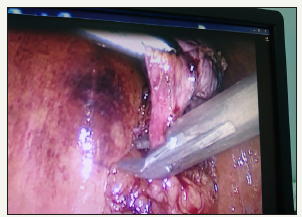
Other 3 ports are inserted under direct vision as mirror image of routine cholecystectomy- 10mm port at left subxyphoid area, 5mm port at left hypochondrium on the midclavicular line but little bit caudally in order to have access to medial part of lower GB and to Calot’s triangle, other 5 mm port inserted at left iliac fossa in the anterior axillary line. During surgery it was difficult to release the adhesions between gallbladder and greater omentum (Figure 5), also dissection of Calot’s triangle by left hand from epigastric port, so we used mainly Rt hand (Figure 6). Subsequently the subcostal port became the main working cannula. It was much easier dissecting lateral part (left side) of of neck of GB (Figure 7). Clipping of cystic duct and arteries was difficult from epigastric port so we used 5mm clip applier through subcostal 5 mm port (Figure 8). There were no anatomical variations or abnormalities. A lot of linear adhesions encountered between diaphragm and liver, between greater omentum and anterior abdominal wall (Figure 9), all of them easily and safely released
Figure 6:Dissecting fatty tissue at the GB and cystic duct junction.

Figure 7:Lateral (left side of GB) dissection, which was much easier than medial dissection.

Figure 8:5mm clip applier inserted from left subcostal port to clip the cystic duct.
Epigastric port used for specimen retrieval. Surgery time was 40minutes. Patient discharged home same day. Postoperative period was uneventful. Port site wounds are healed by primary intention (Figure 10). Further follow up within 1-year period patient remains asymptomatic. In literature we did not find laparoscopic cholecystectomy in SIT done as day case. Reported cases in literature all of them had MRI or CT prior surgery, our case we did not. And we recommend that routine MRI and CT is not to be done unless there are specific indications. Also, probably we are the first using 5mm clip applier in left sided laparoscopic cholecystectomy.
Figure 9:Adhesions between greater omentum and anterior abdominal wall, between liver and diaphragm. They are released easily from left subcostal port.
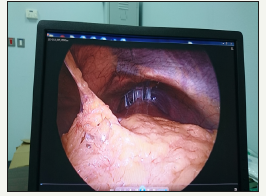
Figure 10:Port side wounds are healed by primary intention. Note that left subcostal port is placed caudally than usual.

Conclusion
A. Left sided cholelithiasis in adult patients could be safely treated like routine Gall Stone disease as day case surgery.
B. MRCP and CT studies are not indicated routinely in adult patients with situs inversus totalis, unless there are specific indications, like deranged liver functions, jaundice or CBD dilatation or doubtful US findings et c.
C. Surgery should be done by experienced surgeon as there are a lot of ergonometric difficulties during dissection of Calot’s triangle, applying clips and even during dissecting lower medial part of gall bladder from liver.
D. 5mm clip applier may be needed. If it is not available, we recommend inserting 10mm port at left subcostal area (not 5 mm), and left sub xyphoid port can be 5 mm only.
Contributor
IIB is the surgeon of the case. SBA is the second surgeon, MFL the surgeon who followed patient postoperatively, GHB is the author of manuscript, IIB and HIB are contributed in the literature review and pictures management.
References
- Annamaria W, John K (2018) Situs inversus imaging medscape. Drugs & Diseases Radiology.
- Kumar S, Fusai G (2007) Laparoscopic cholecystectomy in situs inversus totalis with left-sided gall bladder. Ann R Coll Surg Engl 89(2): W16-W18.
- Rosen H, Petrosyan M, Mason RJ (2015) Cholecystitis in situs inversus totalis. Radio Case Rep 3(4): 226.
- Ibrahim AS, Mohammed HA, Mohammed H (2013) Laparoscopic cholecystectomy in situs inversus totalis: Feasibility and review of literature. Int J Surg Case Rep 4(8): 711-715.
- Campos L, Sipes E (1991) Laparoscopic cholecystectomy in a 39-year old female with situs inversus. J Laparoendosc Surg 1(2): 123-125.
- TS Malatani (1996) Laparoscopic cholecystectomy in situs inversus totalis: a case report and a review of literature. Annals of Saudi Medicine 16(4): 458-459.
- Jamal H, Omar AH (2008) Laparoscopic cholecystectomy in situs inversus totalis. Saudi J Gastroenterol 14(1): 31-32.
- Suleyman B, Halil C, Tuba A, Huseyin K (2012) Single incision laparoscopic cholecystectomy in situs inversus totalis. J Surg Tech Case Rep 4(2): 129-131.
- Deguchi Y, Mitamura K, Omotaka S, Eguchi J, Sakuma D, et al. (2015) Single-incision cholecystectomy in a patient with situs inversus totalis presenting with cholelithiasis: A case report. Asian J Endosc Surg 8(3): 347-349.
- Han HJ, Choi SB, Kim CY, Kim WB, Song TJ, et al. (2011) Single-incision multiport laparoscopic cholecystectomy for a patient with situs inversus totalis: report of a case. Surgery Today. 41(6): 877-80.
- Rungsakulkij N, Tangtawee P (2017) Fluorescence cholangiography during laparoscopic cholecystectomy in a patient with situs inversus totalis: a case report and literature review. BMC Surg 17(1): 43.
© 2019 Ifrat IB. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






