- Submissions

Full Text
Psychology and Psychotherapy: Research Studys
Psychological Modification Combining Advanced Medication and Psychotherapy: Findings from the Studies of Neuroplasticity
Rakib Miah*
Department of Anesthesiology, University of Colorado School of Medicine, USA
*Corresponding author: Department of Anesthesiology, University of Colorado Anschutz Medical Campus, 12801 E 17th Place, Research 1, South L18-4400C, Aurora, CO 80045, USA
Submission: September 29, 2025;Published: October 14, 2025

ISSN 2639-0612Volume9 Issue 3
Abstract
Before the era of advanced medicines, psychotherapy has long been recognized as an effective treatment for a range of psychological disorders, however, neuroscience has only just begun to comprehend how “talk therapies” cause measurable changes in the brain. Numerous recent studies from neurobiological and neuroimaging studies, psychotherapy promotes neuroplasticity by changing brain circuits related to memory, emotion regulation, and self-awareness. The brain regions named prefrontal cortex, hippocampus and amygdala are impacted by Cognitive-Behavioural Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), psychodynamic therapy, and mindfulness-based therapies. These insights show that psychotherapy is more than just a cognitive or behavioural exercise; it is a physically active process that can change brain connections. The neurological underpinnings of psychotherapy in comparison to pharmaceutical methods have been explored in this review, along with their implications for precision mental health care.
Keywords:Psychotherapy; Psychological disorders; Brain connections; Cognitive disorders; Mental health
Abbreviations: AI: Artificial Intelligence; CBT: Cognitive-behavioural Therapy; DMN: Default Mode Network; EEG: Electroencephalography; EMDR: Eye Movement Desensitization and Reprocessing; fMRI: Functional Magnetic Resonance Imaging; MBCT: Mindfulness-based Cognitive Therapy; mPFC: Temporal Lobes, Medial Prefrontal Cortex; PCC: Posterior Cingulate Cortex; PFC: Prefrontal Cortex; PTSD: Post-Traumatic Stress Disorder
Introduction
Although psychotherapy is sometimes referred to as “talk therapy,” new discoveries in neuroscience show that its benefits go well beyond words and feelings. Psychotherapy may alter the structure and function of the brain, resulting in detectable changes in neural networks associated with mental health problems involving depression, anxiety, and trauma, according to recent studies using neuroimaging corresponding to these discoveries, psychotherapy could potentially be just as therapeutically effective as pharmaceutical interventions, but through specific mechanisms, questioning the conventional distinction between “biological” and “psychological” interventions [1,2]. These results raise doubt on the conventional classifications between “biological” and “psychological” therapies, indicating that psychotherapy has the same biological effectiveness as pharmaceutical interventions albeit working through different methods [3,4].
The guiding principle behind these research results is neuroplasticity, which refers to the brain’s potential to transform itself in response to stimuli [5]. Through introducing patients to novel ways of thinking, feeling, and connecting, psychotherapy facilitates the adaptive rewiring of circuits related to memory consolidation, regulation of emotions, and cognition [6,7]. Upon therapeutic interventions, studies employing structural imaging, Electroencephalography (EEG), and Functional Magnetic Resonance Imaging (fMRI) consistently reveal changes in the hippocampus, amygdala, prefrontal cortex, and other important brain regions [8,1].
In order to evaluate the brain effects of various therapeutic modalities with those of medication and to address the clinical consequences for the future of integrative mental health care, this review examines the growing amount of research that links psychotherapy to neuroplastic alterations. It does accomplish by highlighting a crucial point: psychotherapy is about altering brains, instead of just minds.
Neuroplasticity and Psychopathology
The psychological concept of neuroplasticity, or the brain’s capacity to alter itself in response to experience, is at the heart of these findings. This capacity for adaptation is the basis for both normal growth and the possibility of mental health healing [5].
In psychopathology, maladaptive neuroplasticity is commonly
observed. For evidence,
a) Impaired or lower prefrontal activation and higher amygdala
reactivity are linked to depression [9].
b) Hyperactive threat-processing circuits in the amygdala and
compromised connection with regulating prefrontal areas are
hallmarks of anxiety disorders [10].
c) Impaired hippocampus function is an indicator of PTSD, which
leads to inadequacies in contextual memory and increased
reactive reactions [11].
By stimulating adaptive brain rewiring, psychotherapy is designed to restore these imbalances and improve mood, cognition, and behaviour regulation. This is the principle of psychotherapy, which tries to alleviate brain’s problems in a non-invasive way.
Evidence from Neuroimaging Studies
Neuroimaging research conducted approximately over the last 20 years has produced strong proof that psychotherapy alters the structure and function of the brain in measurable manners. An amazing principle was found where these outcomes suggest that certain brain circuits connected with memory, emotion control, and cognition are impacted by psychotherapy therapies. Crucially, there is a correlation between these brain alterations and clinical outcomes, demonstrating that psychotherapy is a physiologically proactive therapy rather than just a psychological one [6,8]. A table of brief clinical evidences of psychotherapies those have positive outcome for different brain diseases in Table 1.
Table 1:Neuroimaging clinical evidence of psychotherapy-induced brain changes.
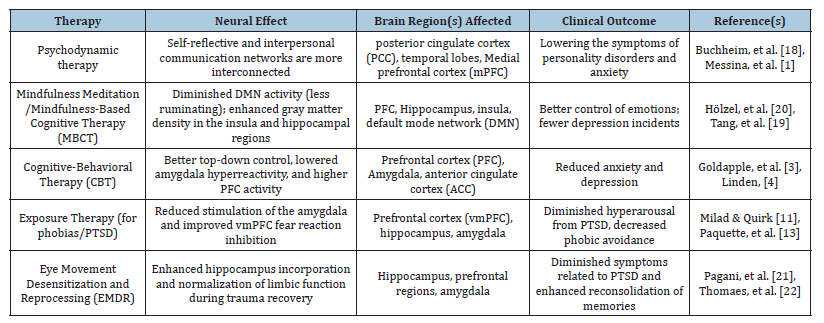
Expansion of Narratives
Psychodynamic therapy has been demonstrated to improve connection in networks that promote emotional control and self-awareness [18]. Despite having a limited range of evidence, the findings point to brain substrates that support therapeutic improvement.
Mindfulness-Based Cognitive Therapy (MBCT) improve the areas of the brain linked to emotional equilibrium and interoception. Hölzel, et al. [20] showed that mindfulness prevents rumination by lowering activity in the default state system and increasing structural activity in the hippocampus gray matter.
Cognitive-Behavioural Therapy (CBT) has continuously demonstrated prefrontal-limbic circuit modulation. For instance, Goldapple, et al. [3] reported that Cognitive Behavioural Therapy (CBT) for depression enhanced prefrontal activation and decreased amygdala hyperactivity, promoting better cognitive control over depression.
Exposure Therapy (for phobias/PTSD) decreases phobia avoidance and PTSD hyperactivity symptoms by increasing vmPFC-mediated extinction processes and decreasing fear-related amygdala activity [13].
Eye Movement Desensitization and Reprocessing (EMDR) encourage adaptive reconsolidation of traumatic memories by regulating abnormal limbic activation during traumatic memories [21].
Medication vs. Psychotherapy: Converging and Diverging Paths
Whether both therapies work through different or overlapping brain pathways is one of the main areas of discussion in clinical neuroscience. Although the processes behind these benefits may differ, either approach can result in clinical improvements in disorders like anxiety and depression.
For converging pathway, neuroimaging evidence shows that antidepressant medication and psychotherapy both impact the activity in the prefrontal-limbic circuitry, specifically in the hippocampus, amygdala, Anterior Cingulate Cortex (ACC), and Prefrontal Cortex (PFC). These areas are linked to stress responses, emotional regulation, and cognitive control [4,9] which showed prominent relations.
Antidepressant drugs like SSRIs restore balanced PFCamygdala connection and normalize amygdala hyperactivity [10,12]. On the other hand, Cognitive Behavioural Therapy (CBT) by strengthening prefrontal cortical control over limbic regions, has been established to improve top-down regulation and decrease amygdala hyperactivity [3,13].
Therefore, the goal of both modalities remains identical: to improve better emotion regulation by recalibrating impaired neural networks. This convergence implies that the most recent shared neuronal pathway may entail reestablishing efficient communication between the PFC and limbic areas, despite conflicting surface-level processes (biochemical modulation vs. discourse) [14].
For the diverging pathways, at the same time, numerous notable
variations exist.
A. Biochemical vs. Cognitive Focus: Psychotherapy addresses
reorganizing inappropriate cognitive processes and developing
new strategies for coping, whereas medicine directly targets
the systems that produce neurotransmitters.
B. Temporal dynamics: While psychotherapy changes require
time and depend on learning, memory consolidation, and
neuroplasticity, medications frequently trigger quick changes
in neurotransmitter activity (e.g., dopamine, serotonin) [5,12].
C. Neuroplasticity mechanism: Through repeated practice and
fresh learning, psychotherapy seems to activate mechanisms
of experience-driven plasticity, which reshape brain circuits
[15]. Pharmacotherapy, on the other hand, indirectly promotes
plasticity through molecular adjustments in receptor
modulation and synaptic transmission [4].
D. Sustainability: Though medication-related psychological
changes frequently reverse after quitting unless behavioural
improvements are integrated, long-term studies indicate
psychotherapy may result in more enduring brain adjustments
[6].
Clinical Outcomes
There are various implications for comprehending how
psychotherapy modify the brain:
a) Therapy optimization: By showing which approaches result
in the most profound brain benefits, neuroimaging may help
with boosting therapies.
b) Personalized treatment: The most suitable candidates for
CBT, mindfulness, or EMDR may be determined by neural
indicators.
c) Reduction of stigma: The concept of mental illness is only
“in the mind” is dismissed by demonstrating the physiologic
impacts of psychotherapy.
Future Direction
In the age of Artificial Intelligence (AI), nowadays, we are having
a thought that almost every approach can be optimized and boosted
to reduce systematically compromised situations. So do clinical
therapies and practices. A few approaches can lead to significant
potent windows to combine and improve both medication and
therapies.
A. Long-term meta-analysis: For the better understanding of
brain functions sustainability, more longitudinal studies to
track responses.
B. Precision practices for psychology: Integrating advanced
clinical practices like neuroimaging biomarkers into decisionmaking
or altering therapies for better outcomes.
C. Combine practices: Both medication and therapy can
be combined with a goal of synergistic outcome, such
as neuromodulation technique, Transcranial Magnetic
Stimulation (TMS) if paired with psychotherapy.
D. Big Data and AI: Massive neuroimaging datasets for
personalized therapy suggestions can be analysed in a machine
learning manner with AI assistance.
E. Discovery of novel biomedical targets: An emerging
biomedical target is the SIRT1 (sirtuin-1) gene, and its
product, which is a NAD+-dependent deacetylase protein, a
pivotal regulator of neurogenesis and synaptic plasticity in the
brain [16]. Numerous processes, many of which are impacted
by SIRT1 activity, trigger age-related cognitive decline,
including lowered neurogenesis, decreased synaptic density,
oxidative stress formation, and mitochondrial malfunction.
When integrated with interventions that increase SIRT1
expression and activity, cognitive training and rehabilitation
programs that test memory, attention, and executive skills may
be more effective. SIRT1 is a prospective target for cognitive
enhancement therapies in aging populations because of its
function in promoting synaptic plasticity, memory formation,
and neuroprotection against age-related cognitive decline [17].
Though these studies were done in 2010, today’s therapeutic
purposes are still prominent if targeted by psychotherapists as
an assistance to drug treatment or psychotherapy.
Conclusion
Psychotherapy is a biologically active intervention that depends on neuroplasticity to change the structure of the brain, instead of just a cognitive or emotional process. Psychotherapy techniques like cognitive behavioural therapy, mindfulness, EMDR, and psychodynamic therapy have been shown to produce tangible adjustments in the circuits responsible for emotion regulation, memory, and self-awareness. This has been backed by evidence from neuroimaging and neuroscience. The argument of implementing psychotherapy alongside pharmaceutical methods in contemporary mental health care is strengthened by the recognition of psychotherapy as a tool for brain rewriting to modify.
References
- Messina I, Sambin M, Palmieri A, Viviani R (2013) Neural correlates of psychotherapy in anxiety and depression: A meta-analysis. PLoS ONE 8(9): e74657.
- Schoenfeld TJ, McCausland HC, Morris HD, Padmanaban V, Cameron HA (2017) Stress and loss of adult neurogenesis differentially reduce hippocampal volume. Biological Psychiatry 82(12): 914-923.
- Goldapple K, Segal Z, Garson C, Lau M, Bieling P, et al. (2004) Modulation of cortical-limbic pathways in major depression: Treatment-specific effects of cognitive behavior therapy Arch Gen Psychiatry 61(1): 34-41.
- Linden DEJ (2006) How psychotherapy changes the brain-the contribution of functional neuroimaging. Mol Psychiatry 11(6): 528-538.
- Kays JL, Hurley RA, Taber KH (2012) The dynamic brain: Neuroplasticity and mental health. J Neuropsychiatry Clin Neurosci 24(2): 118-124.
- Barsaglini A, Sartori G, Benetti S, Pettersson-Yeo W, Mechelli A (2014) The effects of psychotherapy on brain function: A systematic and critical review. Prog Neurobiol 114: 1-14.
- Cozolino LJ (2017) The neuroscience of psychotherapy: Healing the social brain. In: (3rd edn), W.W. Norton & Company, USA.
- Beauregard M (2014) Functional neuroimaging studies of the effects of psychotherapy. Dialogues Clin Neuroscience 16(1): 75-81.
- Mayberg HS (2003) Modulating dysfunctional limbic-cortical circuits in depression: Towards development of brain-based algorithms for diagnosis and optimised treatment. Br Med Bull 65(1): 193-207.
- Etkin A, Wager TD (2007) Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 164(10): 1476-1488.
- Milad MR, Quirk GJ (2012) Fear extinction as a model for translational neuroscience: Ten years of progress. Annu Rev Psychol 63(1): 129-151.
- Harmer CJ, Goodwin GM, Cowen P J (2009) Why do antidepressants take so long to work? A cognitive neuropsychological model of antidepressant drug action. Br J Psychiatry 195(2): 102-108.
- Paquette V, Lévesque J, Mensour B, Leroux JM, Beaudoin G, et al. (2003) “Change the mind and you change the brain”: Effects of cognitive-behavioral therapy on the neural correlates of spider phobia. NeuroImage 18(2): 401-409.
- Gorka SM, Young CB, Klumpp H, Kennedy AE, Francis J, et al. (2019) Emotion-based brain mechanisms and predictors for SSRI and CBT treatment of anxiety and depression: A randomized trial. Neuropsychopharmacology 44(9): 1639-1648.
- Cozolino L (2017) The neuroscience of psychotherapy: Healing the social brain, In: (3rd edn), W. W. Norton & Company, USA, p. 584.
- Gao J, Wang WY, Mao YW, Gräff J, Guan JS, et al. (2010) A novel pathway regulates memory and plasticity via SIRT1 and miR-134. Nature 466(7310): 1105-1109.
- Donmez G, Wang D, Cohen DE, Guarente L (2010) SIRT1 Suppresses beta-amyloid production by activating the alpha-secretase gene ADAM10. Cell 142(3): 494-495.
- Buchheim A, Viviani R, Kessler H, Kächele H, Cierpka M, et al. (2012) Changes in prefrontal-limbic function in major depression after 15 months of long-term psychotherapy. Plos One 7(3): e33745.
- Tang YY, Hölzel BK, Posner MI (2015) The neuroscience of mindfulness meditation. Nat Rev Neurosci 16(4): 213-225.
- Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, et al. (2011) Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research 191(1): 36-43.
- Pagani M, Di Lorenzo G, Monaco L, Daverio A, Giannoudas I, et al. (2015) Neurobiological response to EMDR therapy in clients with different psychological traumas. Front Psychol 6: 1614.
- Thomaes K, Dorrepaal E, Draijer N, Jansma EP, Veltman DJ, et al. (2014) Can pharmacological and psychological treatment change brain structure and function in PTSD? A systematic review. J Psychiatr Res 50: 1-15.
© 2025 Rakib Miah, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






