- Submissions

Full Text
Orthopedic Research Online Journal
Non-Union of the Humeral Shaft in Adults. Does Osteomuscular Decortication and Iliac Graft Support Promote Bone Consolidation?
Tékpa BJD*, Mapouka M, Yafondo TA, Fassioni Eve, Tékpa SB and Nabia DR
Department of Orthopedic and Traumatology, Community University Hospital of Bangui, Central African Republic
*Corresponding author: Tékpa BJD, Department of Orthopedic and Traumatology, Community University Hospital of Bangui, Central African Republic
Submission: April 18, 2022;Published: August 24, 2022

ISSN: 2576-8875 Volume9 Issue5
Abstract
Introduction: Non-union are the most common complications of diaphyseal fractures of the humerus. The management of this condition varies on the type of pseudarthrosis. The objective of the study was to assess the results of our treatment.
Patients and methods: We conducted a retro-prospective study between April 2011 and March 2016, involving 50 cases of non-union of the humeral shaft in our department. Non Septic non-unions without bone defect were treated by osteomuscular decortication with or without iliac grafting. The patients were aged 18 years or older, followed and evaluated at a minimum follow-up of 12 months. The non-unions were distributed by septicity and vitality based on Weber and Čech classification. The osteomuscular decortication with or without iliac graft was the most used surgical technique. The Stewart-Hundley criteria were used to assess the functional results of the affected arms. The data were analyzed using Epi info 2010 version 3.5.2. The Chi2 test was used to compare the pre-operative and post-operative outcomes for a significance level retained at 0.05.
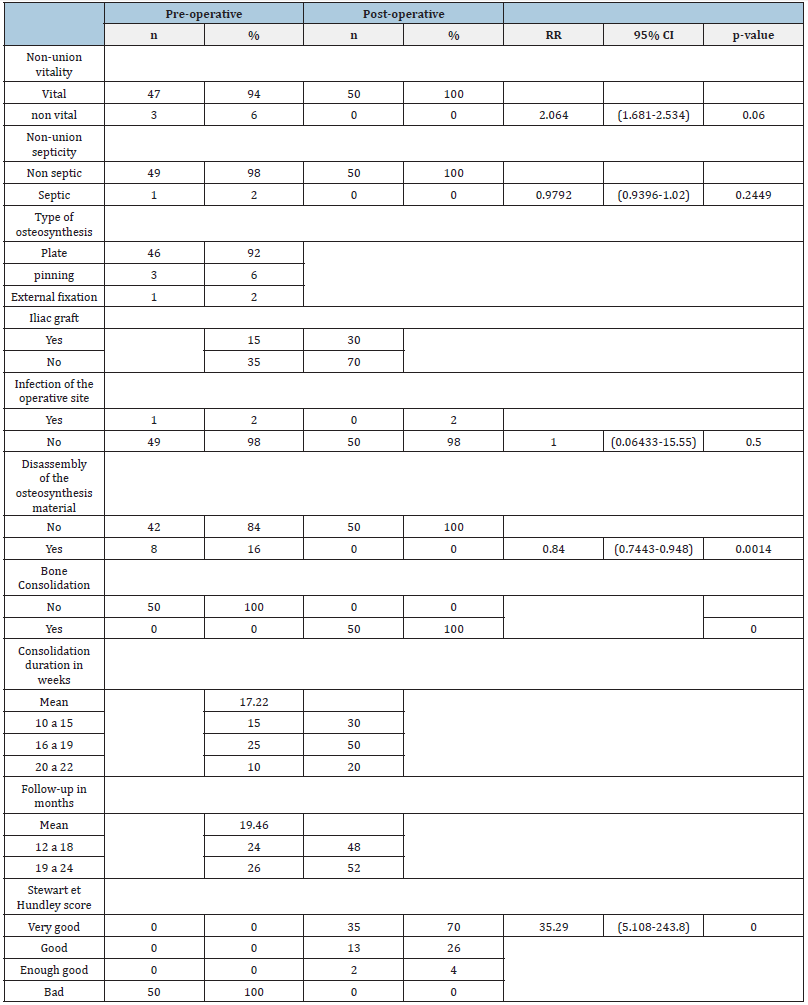
Results: There were 47 cases (94%) of vital non-union and 3 cases (6%) of non-vital humeral shaft non-union. One pseudarthrosis was septic. The osteosynthesis used plate in 46 cases (92%), intramedular pinning in 3 cases (6%) and the external fixator in the only case of septic pseudarhtrosis after recovery from infection (2%). The postoperative was free of infection and disassembly of the ostheosynthesis material allowing to significantly reduce the risk of complications (RR 0.84) (95% CI 0.7443-0.948) (p = 0.0014). All the patients consolidated (p = 0.000). The mean time to union was 17.2 weeks (range: 10 and 22). The postoperative functional results according to the Stewart and Hundley score compared to the preoperative ones were very good in 35 cases (70%), good in 13 cases (26%) and quite good in 2 cases (4%) (P = 0.0000) (95% CI: 5.108-243.8).
Conclusion: The treatment of non-union of the humerus shaft without defect by osteomuscular decortication and osteosynthesis using plate leads to a bone, with satisfactory clinical and functional outcomes.
Introduction
A uniform definition of non-union does not exist. It is defined as an absence of union, six to nine months after the fracture [1]. This definition has been reconsidered recently, no longer taking into account the time factor. Thus, we name pseudarthrosis, the fracture which, for a biological or mechanical reason, will not lead to spontaneous bone consolidation [1-4]. Non-union is the main late complication of diaphyseal fractures of the humerus [2,3,5]. It represents roughly 5% to 10% of all fractures [4,6,7]. It can be classified by vitality of the affectef bone [8]. The middle third of the humerus represents its frequent location [5-7,9]. The treatment of humeral non-union is a challenge for the surgeon. This treatment depends on the type of the non-union [9-11].
The humeral shaft non-union was frequent in our department. We conducted this study to evaluate the outcomes of our surgical treatment.
Hypothesis: Does osteo-muscular decortication lead to bone consolidation?
Patients and Methods
A prospective study on diaphyseal pseudarthrosis of the humerus was conducted between 2011 and 2015 in the only Orthopedics-Traumatology department in Bangui. All types of septic or aseptic, hypertrophic or atrophic pseudarthrosis were studied. Patients consenting to treatment were followed up and evaluated at a minimum follow-up of 12 months. The lost of followup and metaphyseal-epiphyseal localizations were excluded.
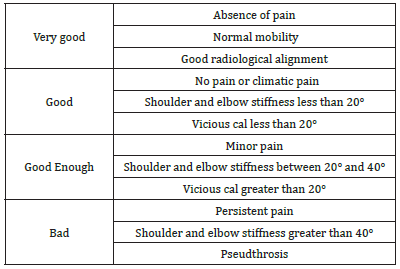
Pseudarthrosis was classified by vitality and septicity based on Weber-Cech classification [12]. The patients arms were functionally assessed in pre and postoperative times using the Stewart and Hundley criteria [13] (Table 1). All the patients were operated by osteomuscular decortication for the hypertrophic (vital) forms.
Table 1:They score stewart and hundley.
The diagnosis of pseudarthrosis was made after clinical and radiological examinations. The vital non-unions were treated by decortication without adding a bone graft. Avital non-unions were also treated by the same procedure but with the addition of bone graft. The debridement with a control of the infection before surgery was used in the septic forms. The unique septic pseudarthrosis was treated by external fixation. The bone consolidation was clinically confirmed by the lack of mobility at the site of the old fracture, an absence of pain and apparition of a mature callus.
A survey sheet including the socio-demographic characteristics, clinical, therapeutic and follow-up aspects was used to collect the data from each patient. The data analysis was performed using Epi info 2010 version 3.5.2. The Chi2 test was used to compare the pre-operative and post-operative outcomes for a significance level retained at 0.05.
Results
The study included 50 patients (37 men and 13 women). The mean age of the series was 41.6 years (range 22 and 75 years). There were 31 (62%) cases of non-union of the right humerus versus 19 (38%) non-union of the left humerus. The middle third of the right humerus was the most affected. The most frequent fracture lines were oblique (49%) and transverse (32.7%). The causes of fractures complicated by non-union were road accidents in 36 cases (72%), firearms in 5 cases (10%). The initial management of fractures before the onset of pseudarthrosis was carried out in 7 cases (14%) by bonesetter consultants and 43 (86%) by doctors. The initial treatment was orthopedic in 21 cases (42%), surgical in 20 cases (40%) and traditional in 9 cases (18%). Iliac graft was used in 15 cases. A patient with septic nonunion consolidated without infection after stabilization with an external fixator. All the patients consolidated (p = 0.000). The mean time to union was 17.2 weeks (range: 10 and 22). The postoperative functional results according to the Stewart and Hundley score compared to the preoperative ones were very good in 35 cases (70%), good in 13 cases (26%) and quite good in 2 cases (4%) (P = 0.0000) (95% CI: 5.108-243.8) (Figure 1 ; Tables 1-3).
Figure 1: Osteomuscular decortication followed by iliac graft in a 33-year-old patient.
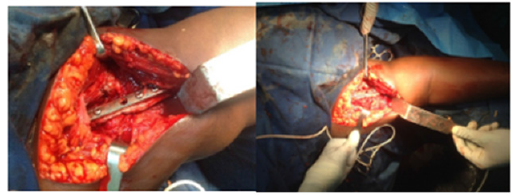
Table 2:Sociodemographic characteristics of all participants.
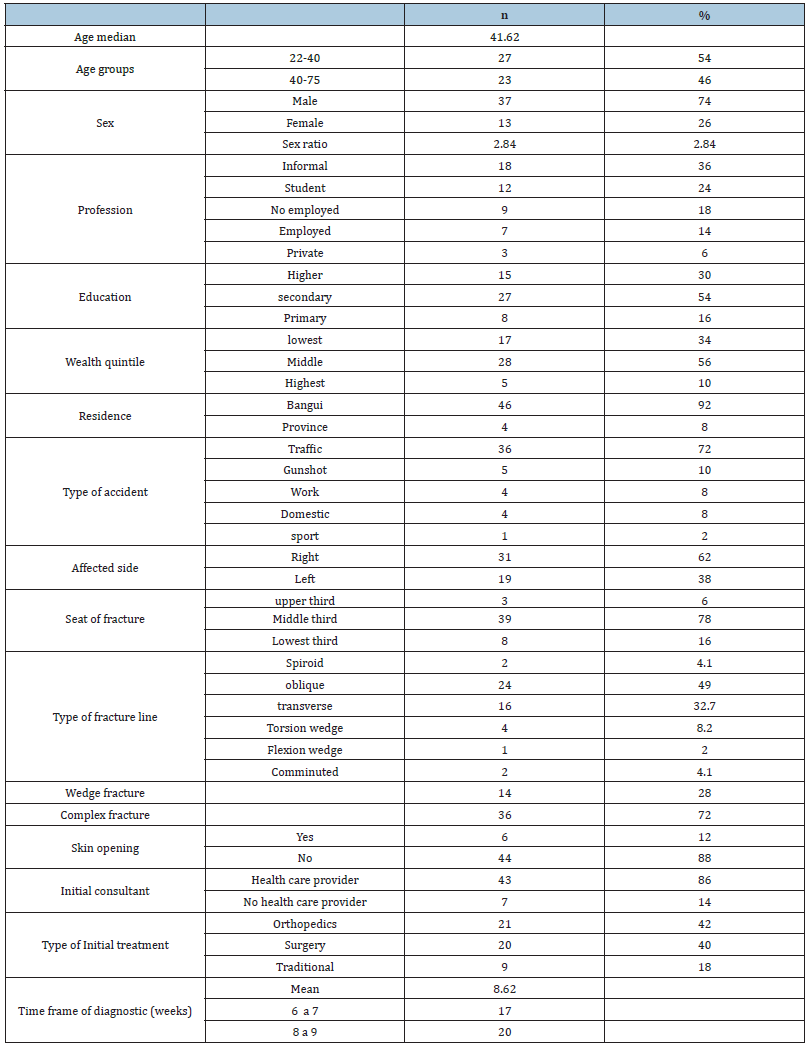
Table 3:Pre-operative and post-operative evaluation.
Discussion
The population of the study is young and could be explained by the hyperactivity of young populations and the proliferation of twowheeled vehicles in our country in recent years [7,14-19]. Most of our patients were males [7,14,18,20]. Public road accidents were the most cause with 72% of cases followed by gunshot injuries with 10% of cases. On the one hand, this result was explained by traffic accidents [21,22]. For instance, there has been increase in two-wheeled vehicles in the Central African Republic, in particular motorcycle taxis with a net increase in the number of accidents linked to them in recent years [22]. On the other hand, the increase in the number of firearm accidents in our series is explained by the military-political crisis in the Central African Republic [21]. The line of the initial fractures was predominantly oblique [5] followed by the transverse line. Similar results were reported in the literature by Dahmani [6], Padhye [7] and Baba [23]. The initial traditional treatment of fractures before the onset of non-union in our series was not negligible. These practices remain common in the Central African Republic as in some African countries, unlike the trends in some European countries whose authors have reported surgical treatment as the primary cause [5,24].
Our time frame for diagnosing the non-union was similar to that reported by Tall, Abalo, Martinez and Mohammed [14-16,18].
We had a case of septic non-union. This was the only patient in our series who was treated with the external fixator after the management of the infection [5,7]. This isolated infection in preoperative time was controlled after regular dressings and appropriate antibiotic therapy adjusted by an antibiogram before surgery. The postoperative time was uncomplicated and led to consolidation. The author Lavini et al had also used the external fixator like us for the treatment of septic non-union in their study [25]. Among the 50 patients, 15 received iliac graft treatment. The majority of our patients was treated by osteomuscular decortication and screw plate. The iliac graft was provided in 15 cases (30%). This method of treatment by screwed plate associated or not with an iliac graft supply was preferred in our country because of the technical platform and the competence of human resources. It also remains the most found and described method in the literature concerning the treatment of non-union of the humeral shaft [7,14,21,26-28]. Rarely, some authors used other treatment methods with Kuntcher nails, Hacketal and modified intramedullary nails which tend to be abandoned [19].
Our treatment made it possible to eliminate the septicitis of the non-union with a statistically significant test threshold in postoperative time. None of our patients presented with paresis or paralysis of the radial nerve after surgery [15,16]. All the non-union that occurred on the osteosynthesis materials and complicated to disassemble were treated in our series and we did not have a postoperative disassembly [16,21,27].
All the non-union of our operated patients consolidated with a timing similar to those reported by several authors [16,29].
We chose our follow-up with exterms of 12 and 24 months to properly assess our patients and get satisfactory functional results. This duration led to a bone consolidation and allowed the necessary time for the patients to participate in the kinesitherapy sessions and recover to their maximum functionality before the pseudarhtrosis. Several authors had results close to our follow-up [5,16,18,21].
We had very satisfactory and statistically significant postoperative functional results postoperatively according to the based on Stewart and Hundley score. Dahmanietcoll, Gogoua etcoll [6,13,21] observed similar results in their series. Our result was due to the good quality of care we provide to our patients [30].
Conclusion
Non-union is a late and frequent complication of humeral shaft fracure that can be successfully treated using screw-retained plate associated with the bone graft for better post-operative functional results.
Conflicts of Interest
The authors has not declare conflicts of interest.
References
- Bhandari M, Fong K, Sprague S (2012) Variability in the definition and perceived causes of delayed unions and nonunions. A cross-sectional, multinational survey of orthopedic surgeons. J Bone Joint Surg Am 94: 1091-1096.
- Osman N, Touam C, Masmjean E, Asfazadouriah H, Alnot JY (1998) Results of non operativ and operative treatment of humeral shaft fractures. Ann Chir Main 17: 195-206.
- Kesemenli CC, Subasi M, Arslan H, Necmioglu S, Kapukaya A (2002) Treatment of humeral diaphyseal non unions by interlocked nailling and autologus bone grafting. Act orthopbelg 68: 471-475.
- Thein E, Chevalley F, Borens O (2013) Aseptic pseudoarthrosis of the long bones. Rev Med Suisse 9: 2390-2396.
- Segonds JM, Alnot JY Masmejean E (2003) Pseudarthrosis and aseptic delayed consolidation of the humeral diaphysis. Rev Chir Orthop 89(2): 107-114.
- Dahmani O, Bouziane A, Shimi M, Elibrahimi A, Elmrini A (2013) Aseptic non-union of humeral shaft fractures. Chir Main 32(2): 85-91.
- Padhye KP, Kulkarni VS, Kulkarni GS, Kulkarni MG, Kulkarni S, et al. (2013) Plating, nailing, external fixator and fibular strut grafting for non-union of humeral shaft fractures. Journal of Orthopaedic Surgery 21(3): 327-331.
- Weber BG, Čech O (1973) Pseudarthroses - pathophysiology, biomechanics, therapy, results. Huber I (Ed.), Bern, Stuttgart, Toronto, Canada.
- Chantelot C, Ferry S, Lahoude-Chantelot S, Prodomme G, Guinand C, et al. (2005) Surgery for pseudarthrosis of humeral shaft. fractures: a retrospective series of 21. Chir Main 24(2): 84-91.
- Crosby LA, Norris BL, Dao KD, McGuire MH (2000) Humeral shaft non unions treated with fibular allograft and compression plating. Am J Orthop (Belle Mead NJ) 29: 45-47.
- Wright TW (1997) Treatment of humeral diaphysealnonunions in patients with severely compromised bone. J South Orthop Assoc 6: 1-7.
- Weber BG, Čech O (1973) Pseudarthroses - pathophysiology, biomechanics, therapy, results. (1st edn), Huber, Bern, Stuttgart, Toronto, Canada.
- Stewart MJ, Hundley JM (1955) Fractures of the humerus; a comparative study in methods of treatment. J Bone Joint Surg 37-A: 681-692.
- Tall M, Bonkoungou D, Sawadogo M (2014) Treatment of diaphyseal pseudarthrosis of long bones on neglected fracture by osteo-muscular decortication. Journal of Orthopedic and Trauma Surgery 100(6): 145-150.
- Abalo A, Dosseh ED, Adabra K, Walla A, James YE, et al. (2011) Open reduction and internal fixation of humeral non-unions: radiological and functional results. Acta Orthop Belg 77(3): 299-303.
- Martinez AA, Cuenca J, Herrera A (2009) Two-plate fixation for humeral shaft non-unions. J Orthop Surg (Hong Kong) 17(2): 135-138.
- Obert L, El Rifai S, Loisel F, Adam A, Lepage D (2015) Resistant or at-risk non-union of the humerus treated with RhBMP7 - single-centre evaluation with a minimum follow-up of 2 years. Suppl Journal of Orthopedic and Traumatological Surgery 10(7): 152.
- Mohammed JA (2014) Functional outcome after surgical plating for humeral shaft nonunion. Egypt Orthop J 49(4): 267-272.
- Ali A, Douglas H, Stanley D (2005) Revision surgery for pseudarthrosis after early failure of osteosynthesis of distal humerus fractures. J Bone Joint Surg [Br] 87-B:1107-1110.
- Checchia SL, Miyazaki AN, Fregoneze M (2009) Pseudarthrosis of the humeral neck: analysis of the results when using the technique described by walch and al. Rev Bras Ortop 44(3): 239-246.
- Gogoua DR, Toure S, Anoumou M, Kouame M, Kone B, et al. (2006) Mechanical complications of limb fracture osteosynthesis an epidemiological analysis of 26 cases. Mali Médical 21(2): 5-7.
- Gassima B (2015) Road traffic accidents by motorized vehicles in Bangui: epidemiological, clinical, therapeutic and evolutionary aspects. Doctorate thesis in medicine. No. 35/2015. Bangui, Central African Republic, p. 150.
- Baba R, Razak M (1998) Contributing factors in non-union of the humeral shaft fracture and the results of treatments. suppl A Med J Malaysia 53: 42-51.
- Ameil GM (1991) Pseudarthroses of the humeral diaphysis Apropos of 58 cases. Rev Chir Ortho Masson, Paris, 117(4): 263-269.
- Lavini F, RenziBrivio L, Pizzoli A, Giotakis N, Bartolozzi P (2001) Treatment of non-union of the humerus using the Ortho fix external fixator. Injury 32: 35-40.
- Metikala S, Bhogadi P (2015) Orthogonal double plating and autologous bone grafting of postoperative humeral shaft nonunion - A rare case report and review of literature. Journal of Orthopaedic Case Reports 5(4): 50-53.
- Bernard De Dompsure R, Peter R, Hoffmeyer P (2010) Uninfected nonunion of the humeral diaphysis: Review of 21 patients treated with shingling, compression plate, and autologous bone graft. Orthop Traumatol Surg Res 96(2): 139-146.
- Devnani AS (2001) Simple approach to the management of aseptic non-union of the shaft of long bones. Singapore Med J 42(1): 20-25.
- Bassiony AA, Almoatasem AM (2009) Infected non-union of the humerus after failure of surgical treatment: Management using the ortho fix external fixator. Ann Acad Med Singapore 38: 1090-1094.
- Beguin JM, Plenevaux P, Poilvache P (1991) Considerations regarding the treatment of nonunions of the humerus. Acta Orthopaedica Belgica 57(2).
© 2022 Tékpa BJD. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






