- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Factors Influencing Orthopedic Surgeons’ Clinical Adoption of Innovative Technologies
Sean Reynolds, Naveen Donthu* and Christopher Campagna
Georgia State University, USA
*Corresponding author: Naveen Donthu, Georgia State University, USA
Submission: January 02, 2024;Published: July 31, 2024

ISSN 2578-0069Volume3 Issue2
Abstract
This study examines behavioral factors that influence the likelihood of orthopedic surgeons’ adoption of innovative technologies, such as 3D printing, in their patient care and treatment. In this empirical investigation, we use Technology Acceptance Model 2 (TAM2) to evaluate the relationships between technology acceptance and surgeon behavior. The PLS-SEM results suggest that subjective norms, image and technology readiness are significant predictors of a positive intention to use technology and subsequently adopt it. These results contribute to the extant research by extending the application of TAM2 to clinical adoption and provides practitioners insights into variables that influence surgeons’ adoption of technology.
Abbreviations:Technology acceptance model; Surgeon decision making; Adoption; Innovation; 3D Printing
Introduction
Medical device organizations consistently seek new ways to remain competitive among their peers and they often attain a competitive edge through the launch of new, innovative products [1,2]. The adoption of these innovative products is not necessarily proven, as certain factors could influence the adoption process [3]. Surgeons are often the target audience for this industry’s innovations and influence these devices’ success, as they are the primary users of these technologies and continue to search for innovations that would improve their patients’ clinical outcomes. The products are usually designed using surgeons’ input to help mitigate the non-adoption of these devices because surgeons provide information that only they would appreciate in those products. Some technologies enjoy successful adoption from surgeon clinicians due to improved clinical outcomes, reduced operating times, greater efficiency, cost savings for the procedure (not necessarily the cost of the technology), etc. The successful adoption of these products is necessary for organizations’ continued growth, as companies spend significant research, development and marketing budgets to bring these products to market. However, strategic and tactical marketing plans can be arbitrary and conceptually flawed [4]. These sales and marketing plans historically follow the process for diffusion models [5], in which surgeon targets become “innovators,” thus influencing the “majority.” This approach does not always translate to increased sales [6]. Although these models describe sales and marketing-timing techniques, they do not provide insight into surgeons’ decision-making processes [7]. Therefore, sales and marketing techniques create a need for more defined ways to target surgeons successfully and determine what drives their adoption behaviors.
Companies that launch these new products need to understand better the factors behind surgeon adoption rates [8]. Although many innovative surgical technologies are available, in this study, we examined adoption behaviors for 3D-Printed (3DP) implants. The 3DP implant market is projected to grow from $973M in 2018 to $3.69B by 2026, with a compounded annual growth rate of 18.2% [9]. The drivers of this growth include applications and benefits that many in the medical arena view as groundbreaking and transformational. This manufacturing process reduces the medical costs of goods [10] and it provides benefits from a clinical aspect, such as in surgical planning (Lah & Patralekh, 2018). Additional beneficial clinical uses of 3DP include the creation of cutting guides; customized, patient-specific implants; and standardized implants, which help the surgeon provide patients with clinical options to improve procedural workflow, patient fit and clinical outcomes [11-13]. For surgeons and patients, these new 3DP implants and tools offer potential improvements in clinical performance and outcomes, such as improved fusion rates in patients, which would help in their surgical recovery [14]. 3DP implants offer advantages compared to prior options of solid titanium and PEEK implants. Titanium also has a strong affinity to bone; therefore, 3DP titanium surfaces are often rough and promote the bony surface adhesion properties required for fusion [15]. Also, 3DP implants with porosity have favorable radiographic-imaging qualities that allow a surgeon to assess the fusion across the implant and promote bone fusion.
We attempt to show what intrinsically motivates spine surgeons’ adoption of 3DP technology and to determine whether there are correlations between social norms and clinical variables with the adoption of this technology. The study includes the effect of subjective norm, image, job relevance, output quality and result demonstrability. We also discuss findings related to surgeons’ Perceived Usefulness (PU) of technology and perception of innovation. We constructed a theory-based model and tested multiple hypotheses. It is important to note that we developed the full model practically, with areas that could be controlled. This study’s main strength is the fact that it is based on the very popular Technology Acceptance Model (TAM). It highlights which attitudes and opinions of surgeons influence their intention and adoption of technology. It provides manufacturers insights into what to emphasize in their communications with the surgeons. Overall, the study makes theoretical and practical contributions.
Technology Acceptance Models
In this study, we focused on surgeons’ behavioral influences that drive their BIs. Two historical theories used to study these BI phenomena are the Theory of Reasoned Action (TRA) [16] and the Theory of Planned Behavior (TPB) [17]. We based this study on the TPB, as the framework we used in the study, the TAM, directly stemmed from the TPB. Ajzen I [17] created the TPB, which is a theoretical model to predict and explain human social behavior and serves as a framework for behavioral change interactions. He wanted to establish a methodology to measure attitudes and norms’ influence on intention and the resultant behavior. He noted that the TRA did not account for perceived behavioral control; therefore, the TPB would improve on the TRA by measuring this construct. Perceived behavioral control regards one’s behavior as being influenced by their self-confidence [18]. From the TPB, Davis FD [19] developed the TAM to measure further the adoption of IT and how behaviors influenced their adoption. Over the last 30 years, TAM has been extensively studied with several iterations of the framework. The TAM has proven to be a validated framework for studying technology adoption across various areas, from consumer adoption to education to hospital management systems [20, Nagy, 2018; Ratten, 2015). In the years since its inception, TAM has been updated numerous times. These updates are the last version of the TAM by Venkatesh VD et al. [21], the TAM2 by Venkatesh V et al. [22], the Unified Theory of Acceptance and Use of Technology (UTAUT) by Venkatesh V et al. [23] and the TAM3 by Venkatesh V et al. [24]. Lai PC [25] discussed these models and their respective contributions to studying technology adoption, specifically to IT.
Minimal studies have been conducted to explore the various TAM frameworks when considering surgeons’ adoption of technology for clinical practices. Although a few studies were found to be healthcare-relevant, the researchers used the TAM to study electronic health records system adoption [26] and automated medication management systems in hospitals [27,20]. Also, Strudwick G [28] postulated the potential use of the TAM to enhance infusion pump use in health care. This application was the closest of any of the TAM models concerning clinical adoption intentions. In a marketplace in which industries are rapidly embracing innovative technology to increase efficiency and provide superior experiences, academia and the healthcare industry agree that this segment has lagged in innovation [29].
Figure 1:TAM2 framework model.
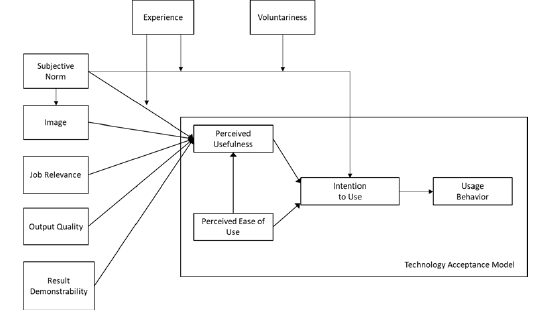
We utilized the TAM2 [22] framework (Figure 1) in this study to help determine which factors influence surgeons’ adoption of 3DP implant technology for clinical use. TAM2 is the most robust model to utilize as a framework due to its applicability in surgeon technology adoption, as it is used to study the cognitive and social factors that may influence the adoption. The core component of the TAM is used to measure these behaviors by using constructs that reflect one’s PU and Perceived Ease of Use (PEOU) of the technology. These two constructs then influence users’ Attitudes Toward technology (AT), which influence the user’s Behavioral Intention (BI) to use the technology. It should be noted that subsequent studies have also referred to BI as Intention to Use (IU). BI should lead to some level of adoption of the technology. TAM2, Venkatesh’s [22] iteration of the TAM, established new constructs encompassing social influence (subjective norms, voluntariness and image) and cognitive instrumental processes (job relevance, output quality, result demonstrability and PEOU) as determinants of PU and use intentions. Based on the other TAM frameworks, this framework is closely aligned with the processes observed in surgeons’ decisionmaking processes when they evaluate technology for clinical use.
Model and Hypotheses
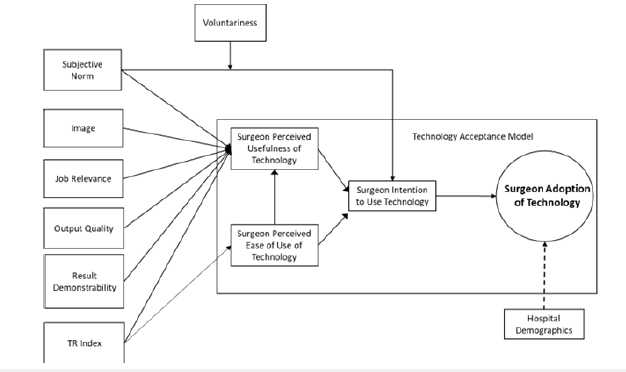
Historically, TAM2 has been sparingly used for clinical application research. Chismar WG et al. [30] examined the use of TAM2 and its applicability to pediatricians and their adoption of internet-based health applications. We also apply TAM2 in the healthcare setting regarding the clinical adoption of technology used in surgery. It is theoretically relevant to evaluate Venkatesh V [22] TAM2 framework within the surgical domain to determine whether it can be applied to clinical applications and account for the impact of the additional Technology Readiness Index construct (Figure 2). This study should provide insights into which of the constructs influence surgeons’ adoption of technology and could thereby serve as an addition to the body of knowledge of TAM frameworks but from a clinical application. For practitioners, this study could provide insights to firms developing innovative technologies regarding how to target their marketing efforts more precisely to surgeons.
Figure 2:Proposed framework model.
The constructs of PU, PEOU and IU are critical components of
the TAM. We will utilize construct-scale items from Venkatesh V et
al. [22] as well as Porter CE et al. [31]. TAM2 differs from the TAM
because TAM2’s external variables directly measure the PU rather
than the PEOU. As Venkatesh V et al. [22] stated, extensive empirical
evidence shows that the PEOU is significantly linked to intention
via its impact on PU. The TAM’s constructs, such as PU, PEOU and
IU, have been thoroughly investigated and shown to influence
adoption positively. Regarding surgeons and their influences on
3DP implant adoption, the PU, PEOU and IU are expected to have
positive relationships similar to those observed in prior studies.
It is hypothesized that surgeons believe technology have a PU for
their surgical procedures and have a PEOU, as the technology would
be viewed as an improvement to current technologies and no more
difficult to use in surgery. These two behaviors would suggest that
the surgeon would therefore intend to use the technology if the PU
and PEOU are positive. Therefore, we hypothesized the following:
H1: Surgeons’ perceived usefulness positively influences the
intention to use.
H2: Surgeons’ perceived ease of use positively influences the
intention to use.
H3: Surgeons’ perceived ease of use positively influences
perceived usefulness.
Subjective Norms (SN), as Fishbein M et al. [16] stated,
measure one’s perception that most people who are important
to him/her think that he/she should or should not perform the
behavior in question. Surgeons are influenced by those who train
them during residency or fellowship. Surgeons attend medical
conferences to share and learn the latest surgical techniques and
use of technologies to improve their clinical outcomes [32], which
often involves discussing the surgical outcomes that result from
various techniques and technologies. Surgeons value the influence
of key opinion leaders in the medical device industry [33] and they
will investigate what technologies others are using and measure
those surgeons’ clinical success. These influences will affect how a
surgeon views the adoption of specific devices.
H4: Surgeons’ subjective norms positively influence
perceived usefulness.
H5: Surgeons’ subjective norms positively influence
intention to use.
Moore GC et al. [34] researched image (I) and defined it
as the degree to which the use of an innovation is perceived to
enhance one’s perception or status in one’s social system. Users of
innovations in the medical field are sometimes viewed favorably
by others, especially if their use leads to demonstrably improved
clinical outcomes. Those individuals will become more visible
among their peers due to discussion of their clinical outcomes and
use of technology in public forums, thus potentially enhancing their
image in their social and medical networks.
H6: Surgeons’ images positively influence perceived
usefulness.
Venkatesh V et al. [22] state that job relevance concerns an
individual’s perception regarding the degree to which the target
system applies to their job. Surgeons will adopt technologies that
provide them with clinical and procedural workflow benefits. They
choose technologies that, in general, will improve or enhance their
surgical skill set.
H7: Surgeons’ job relevance positively influences perceived
usefulness.
Davis FD et al. [35] defined output quality as to how well
a system performs the tasks related to its job relevance. The
technology should demonstrate outputs that are reproducible and
measurable and that improve one’s margin of error in the procedure.
Surgeons will favor technology that improves their patients’ clinical
outcomes and establishes improved clinical efficacy. If a technology
does not demonstrate improved output quality, its PU will diminish.
H8: Surgeons’ output quality positively influences perceived
usefulness.
Moore GC et al. [34] defined result demonstrability as the
tangibility of the results of using a technology, which denotes the
surgeon’s ability to understand the results utilized technology
provides and their ability to communicate this understanding
to others. If the surgeon perceives the technology as useful, they
should be able to communicate this result to others. This ability is
important when surgeons must explain the technology’s benefits
to decision-makers in the hospital to determine whether value
analysis committees will approve the system for use.
H9: Surgeons’ result demonstrability positively influences
perceived usefulness.
Prior research discussed in the literature review has shown
that once a subject’s behavioral intent to use IT technology has
been established by PU and PEOU, the adoption of the technology
more readily occurs [19,21,22]. The same assumption can apply to
surgeons’ intention to use surgical technology clinically.
H10: Intention to use positively influences surgeons’
adoption of technology.
Parasuraman A [36] developed the Technology Readiness
Index (TRI) to measure one’s motivations that may influence the
adoption of new technologies. He created this scale from a validated
questionnaire of 1,200 participants. The developed scale is used to
measure the dimensions of optimism, innovativeness, discomfort
and insecurity concerning various technological products.
Comparing the TRI to PU could serve as a valuable validation
measure. If a surgeon has a high TRI score, then there may be a
positive correlation with PU and/or PEOU and a potentially positive
link to adopting the technology.
H11: Surgeons’ TR Index positively influences perceived
usefulness.
H12: Surgeons’ TR index positively influences perceived
ease of use.
Voluntariness is the extent to which potential adopters perceive
the adoption decision as non-mandatory, as Venkatesh V et al. [22]
described. Surgeons may believe they have no choice in adopting the
technology for potentially many reasons. Either hospital decisionmakers
have mandated it, well-informed patients may request it (or
go to another surgeon who does use the technology), or their social
and medical network all utilize the technology; therefore, they must
adopt it to minimize the perception that they are not providing the
best therapeutic options for their patients.
H13: Voluntariness moderates the relationship between
subjective norms and intention to use.
We used hospital demographics to analyze the demographics of hospitals that adopted the technology. This could explain what roles hospital size, location and ownership have in the influence of the adoption of technology. These factors are beyond the surgeon’s control. Venkatesh V et al. [22] will study the experience variable and concluded that social norms lessened with increased system experience. Venkatesh V et al. [22] did not directly measure this construct and for the purposes of this study, we will also not measure experience.
Method
Primary data collection was performed via a survey instrument and the survey was created using the Qualtrics survey system. The data collected via the survey instrument were analyzed to determine correlations quantitatively among the constructs established in the TAM2 model. The construct scales were structured on a fivepoint Likert scale. An email list compiled from various surgeon conferences and by several spine organizations was utilized. The resultant list included approximately 2,500 surgeons globally. Surgeons were targeted via numerous methods. The first option was the compiled email list. We sent emails linking to the survey and inviting surgeons to complete it three times over three months. The second option was surgeon visits to a spine implant organization’s corporate office. Surgeons were invited to complete the survey at their leisure and were given a business card with the survey link information, including the addition of a Quick Response (QR) code. The third recruitment option concerned individual networking via LinkedIn connections. Surgeon contacts were emailed an invitation to complete the survey via LinkedIn messaging. A fourth recruitment activity involved surgeon participants at various surgeon conferences held in the United States, who were given the survey instrument business card as well. Finally, the fifth option was assistance from select sales representatives, who encouraged surgeon customers to complete the survey by visiting the survey link provided via email. All surgeons contacted via office visits, LinkedIn or sales representative interaction were cross-referenced with the original surgeon email list. The results consisted of 100 completed surveys from 2,500 surgeons, representing an effective response rate of 4%. Although this response rate may seem low, it should be remembered that the respondents are busy surgeons who rarely participate in market research studies.
This proactive strategy allowed us to obtain responses from a variety of spinal surgeons. They were selected based on the criteria of being an orthopedic surgeon or neurosurgeon operating weekly. Participants had access to the survey twenty-four hours per day and were advised to complete the survey during non-business hours. The survey instrument’s questions were further adjusted based on prior research by Chismar WG et al. [30] as well as Burns LR et al. [37], who made modifications appropriate for their research, and we made two similar adjustments. Sentences were reworded to incorporate the nomenclature of technology and the word “surgeon” in questions when applicable to increase interest by providing personal and professional appeal and thus enhance the response rate [30]. We also substituted the word “system” with “technology.” Three surgeons evaluated the survey to ensure that the questions were coherent and that the survey’s length was appropriate and maintained surgeon engagement. The estimated time required for the survey’s completion was five to ten minutes. Once the data were retrieved from the internet survey tool, it was entered into IBM’s SPSS v. 27 and SmartPLS3 v 3.3.3 for quantitative analysis and reporting.
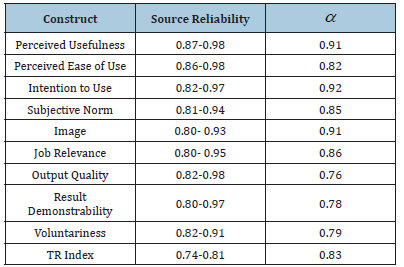
Scales and Measurement
The formative scales for the various theoretical constructs (subjective norms, image, job relevance, output quality, result demonstrability, TRI, voluntariness, PU, PEOU and IU) were utilized from previously established studies. The TAM scales of PU, PEOU and IU were measured using items adapted from Davis FD et al. [38]. The measurements of subjective norms were adapted from Taylor S et al. [39], result demonstrability and image from Moore GC et al. [34], job relevance and output quality from Davis FD et al. [35] and the TRI from Parasuraman A [27]. Reliability regards the internal consistency of items within the construct and is measured via Cronbach’s alpha. According to Venkatesh V et al. [22], the constructs have internal consistency reliability coefficients greater than 0.70 (Table 1).
Table 1:Reliability.
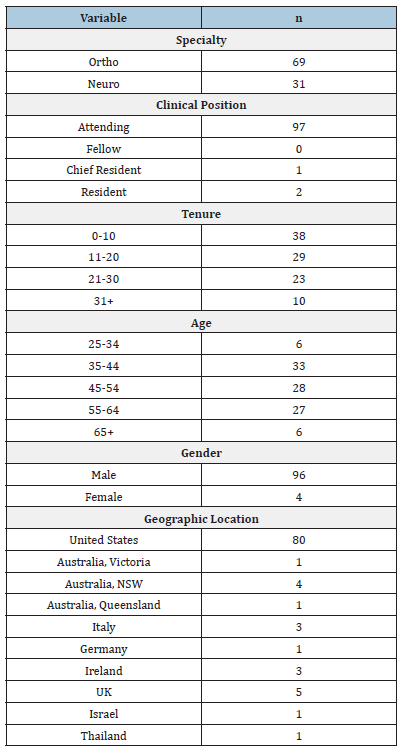
Result
Initial results involved examining the multicollinearity and correlations of the constructs within the framework using SPSS. This portion of the analysis would show which constructs should be examined for structural equation modeling via PLS. The data analysis process included the coding and cleaning of the data collected from the survey. We then performed statistical calculations via SPSS to analyze the collected data. We calculated all the variables’ frequencies and ran error tests. Based on the selected variables, we determined the mean, median, mode and standard deviation. These tasks allowed us to validate the data and eliminate invalid surveys (e.g., missing data or incorrect data entry). As each question required an answer before the respondent could progress in the survey, we had no issues with missing data. We correctly coded text variables to reflect proper measurement and we performed frequency tests on the cleaned data, which entailed reviewing the descriptive statistics. The number of subjects who participated in the study was one hundred and Table 2 presents descriptive statistics for their demographics.
Table 2:Surgeon demographics.
We assessed multicollinearity to ensure that overlapping of factors did not occur among the independent variables. We used the tolerance and Variance Inflation Factor (VIF) to measure collinearity. The resultant tolerance values were all much higher than 0.10 and the VIF values were below 2.0; therefore, we had no issues with multicollinearity [40]. The final SPSS analysis involved correlation analysis to determine the strength and direction of the linear relationship between the variables. Using SPSS, we performed a bivariate calculation to determine the direction (Spearman’s Rho correlation) and strength of the relationships (the magnitude of the value of the correlation coefficient). The only construct that did not have a statistically significant effect on correlation was the relationship between voluntariness and subjective norm. Therefore, we did not measure the moderation on the relationship between subjective norm and IU by voluntariness via SPSS or PLS3.
Dependent Variable
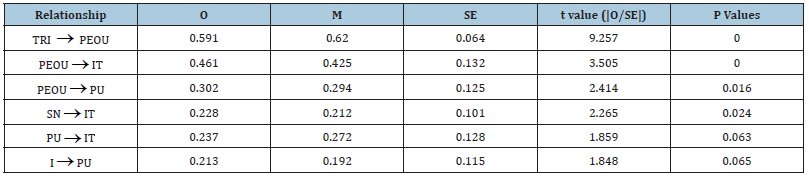
SmartPLS 3.3.3 [41], the PLS-SEM tool we used in this analysis, provided total indirect effects, total effects, outer loadings and outer weights. Furthermore, calculations of tolerance and VIF fell within acceptable ranges [42]. Finally, to determine the contribution of each of the relationships to the latent PU, PEOU and IT constructs, we drew a bootstrap of 5,000 samples and assessed the significance of path coefficients (results shown in Table 3). The relationships not reflected in the table were not statistically significant.
Table 3:Path relationships.
Independent Variable
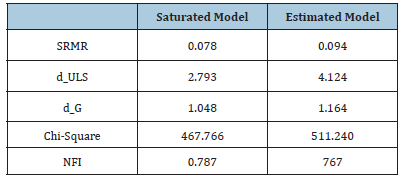
Establishing the IVs’ validity was a two-step process; first, we checked and confirmed each subscale’s internal consistency (Cronbach’s alpha) from the prior SPSS analysis. Next, we confirmed that collinearity did not exist among the IVs (VIF < 1.99). Last, we fit the PLS model (Table 4) and computed and checked the outer loadings and outer weights of respective items of the IVs for magnitude and significance.
Table 4:Model fit.
Model Results
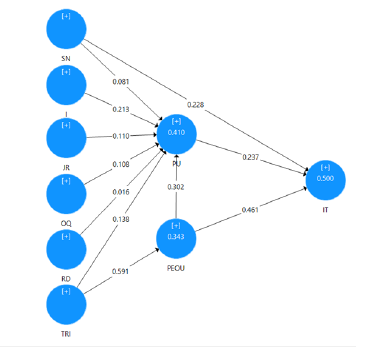
We evaluated the final model and found it explained 50% (adjusted R square) of the variance in IU. We found SN, I and the TRI affected the technology acceptance model’s core variables, PU, PEOU and IT. We found PU (41%) and PEOU (34%) significantly influenced IT. This finding supports the positive responses to the hypothetical question of which factors positively influence surgeons’ adoption of 3DP implants. Figure 3 shows the empirically supported model. To examine differences in these factors’ impact on IU between surgeons who adopted 3DP implants and those who did not, we conducted a multigroup analysis. We determined which groups to compare based on whether the surgeon indicated on the survey that they had adopted 3DP implants. The number of surgeons who adopted 3DP implants was 74 and 26 had not adopted the implants. Interestingly, the surgeons who adopted 3DP implants were located in either large (201+ beds), non-profit or urban medical centers. Using data groups in PLS, we generated the data in Table 5 to analyze the influence of the two separate groups on the model.
Figure 3:Empirically supported PLS-SEM model
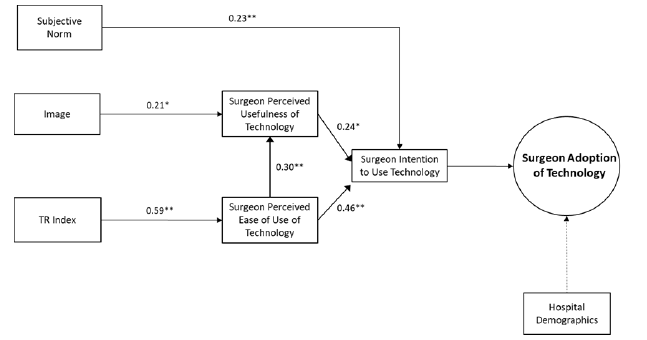
Table 5:R square adjusted results.
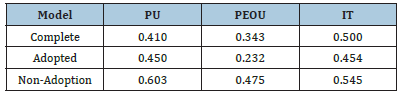
We conducted a multigroup analysis to evaluate differences between DVs across the adoption groups. PU and PEOU consistently predict IU across the two groups. The non-adopters reflected higher R square values, which indicate that the IVs in the model captured the behaviors that did not encourage those surgeons to adopt 3DP implants. Interestingly, the path coefficient of output quality → PU explained 41.5% of non-adopters’ behavior, which we did not observe in the adopter group. The adopter group’s lower R square values indicate that although subjective norm, image and TRI are predictors, we did not capture some behavioral predictors in the model.
Findings and Implications
We analyzed surgeons’ BIs and their likelihood of adopting technology, especially 3DP implants. For this purpose, we used TAM2 to determine which BIs were significant in the model. By studying the various social and cognitive factors that can influence a surgeon’s behavioral intent, we determined that the key influences had a more significant impact than others. We used PLS-SEM to evaluate each hypothesis and the full model. The testing revealed strong relationships and high significance levels between technical readiness, PEOU and intent and surgeons’ IU. This pathway (Figure 4) reveals high coefficient levels between the three variables and strong p-values for each factor. These empirical findings make sense intuitively. Surgeons who keep up with innovative technologies being tested and incorporated into their field of practice would seem more likely to perceive these innovations and their utilization as a relatively seamless process. Consequently, it is logical that this group is often the first among their surgical peers to learn and review new technologies and would perceive technology use as undaunting.
Figure 4:Complete Model.
Discussion
It is reasonable to assume that subjective norms’ positive relationship with IU occurs due to a surgeon’s influences from others. As discussed earlier in the theoretical framework, SN concerns one’s perception that most people who are important to him/her think that they should or should not perform the behavior in question [16]. Surgeons are influenced by other surgeons throughout their careers, from residency and fellowship to post-training. After training, they continue to seek input from other surgeons in their hospital practice and by attending surgeon conferences to learn how research and studies affect clinical care. This effort often involves analyzing the technologies used and these devices’ clinical impact. 3DP implants are currently heavily promoted at surgeon conferences via corporations and surgeons’ panel discussions. Therefore, these influences undoubtedly shape surgeons’ perception of technology’s usefulness and their resulting intention to adopt. It is reasonable to assume that image’s positive relationship with PU occurs due to surgeons’ desire to improve their standing among their peers by using novel technology. We can postulate that image is a factor because it is defined as the degree to which the use of an innovation is perceived to enhance one’s image or status in one’s social system [34]. Surgeons may adopt technologies to improve their image and desire to pioneer the use of new technologies in the hopes of it improving the procedure or their patient’s clinical outcomes. Image helps influence a surgeon’s subjective norm because they in turn can use their knowledge to influence others’ use of novel technology.
The TRI’s influence on PEOU is another predictor of surgeons’ behavior, as it is a strong and very significant factor. A surgeon’s readiness to use technology is not surprising because surgeons often use newer technologies to improve their patients’ clinical outcomes. They also have a propensity to use technology from the very first moment of surgical training. 3DP technology has potential surgical benefits, such as improved workflow, improved fusion rates and outcomes, compared to PEEK implants. Current research has portrayed 3DP implant technology positively; therefore, it is no surprise that spine surgeons’ TRI would influence their PEOU with this technology. SN, image, the TRI, PU, PEOU and IU suggest positive relationships and can predict surgeons’ intention to adopt a technology. However, other predictors that interestingly did not show a statistical relationship included job relevance, output quality and result demonstrability. Although these factors did not show model relevance, we can postulate that they will have statistical significance in a larger sampling pool, especially because the initial SPSS analysis showed correlations between these factors regarding PU. It should be noted that of the one hundred spine surgeons who completed the research survey, seventy-four had officially adopted 3DP implants in their practice.
Overall, the resultant empirically supported model highlights that the intrinsic behaviors that influence surgeons’ adoption of technology include two social influences, subjective norms and image, and one cognitive influence, technology readiness. The sample of surgeons showed significant resultant TAM behavior variables, PU, PEOU, IU and subsequent adoption of 3DP implants. Medical device innovation will continue to proliferate and companies developing novel technologies will need to re-evaluate how they encourage the end-user to adopt them. TAM2 helped us determine that subjective norms, image and TRI influence surgeons’ intent to adopt the technology. Our study provides several contributions for practitioners. One contribution is the application of the TAM to non-IT, clinical technology adoption measurement. This research application suggests that the TAM is a useful model for measuring surgeons’ behaviors regarding the clinical adoption of technology. Finally, we extend previous research by investigating TAM2’s use in clinicians’ technology adoption because it has only been used in an IT healthcare technology adoption study [30].
An important contribution for practitioners is the capability to give companies guidance regarding which social influence norms can be targeted to influence potential users. Medical device companies could use more behavioral marketing to influence surgeons’ perceptions of new clinical technology’s usefulness by implementing social influence campaigns that target a surgeon influencer’s network [43]. Haenlein M et al. [15] confirmed that an individual’s social network includes others like themselves, who tend to have opinion leaders or revenue leaders influencing their network [44]. Marketing activities should target these key opinion and revenue leaders because they could provide a positive subjective norm and image to influence others. Finally, organizations could utilize the TRI to assess a surgeon’s technology readiness and subsequent PEOU.
References
- Clark J, Guy K (1998) Innovation and competitiveness: A review. Technology Analysis & Strategic Management, 10(3): 363-395.
- Tellis G, Jaideep Prabhu, Rajesh Chandy (2009) Radical innovation across nations: the preeminence of corporate culture. Journal of Marketing, 73(1): 3-23.
- Gelijns A, Rosenberg N (1994) The dynamics of technological change in medicine. Health Affairs 13(3): 28-46.
- Varadarajan R (2010) Strategic marketing and marketing strategy: Domain, definition, fundamental issues and foundational premises. Journal of the Academy of Marketing Science 38(2): 119-140.
- Rogers EM (2003) Diffusion of innovations. (5th), The Free Press, London.
- Mahajan V, Muller E (1998) When is it worthwhile targeting the majority instead of the innovators in a new product launch? Journal of Marketing Research (JMR) 35(4): 488-495.
- Roback K, Gaddlin P, Nelson N, Persson J (2007) Adoption of medical devices: perspectives of professionals in Swedish neonatal intensive care. Technology and Health Care 15(3): 157-179.
- Hatz MHM, Sonnenschein T, Blankart CR (2017) The PMA scale: a measure of physicians’ motivation to adopt medical devices. Value in Health 20(4): 533-541.
- Kunsel T, Sumant O (2019) 3D Printing healthcare market.
- Ventola CL (2014) Medical applications for 3d printing: current and projected uses. P & T: A Peer-Reviewed journal for formulary management 39(10): 704-711.
- Mobbs RJ, Coughlan M, Thompson R, Sutterlin CE, Phan K (2017) The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: case report. J Neurosurg Spine 26(4): 513-518.
- Wang YT, Yang XJ, Yan B, Zeng TH, Qiu YY et al. (2016) Clinical application of three-dimensional printing in the personalized treatment of complex spinal disorders. Chin J Traumatol, 19(1): 31-34.
- Wilcox B, Mobbs RJ, Wu AM, Phan K (2017) Systematic review of 3D printing in spinal surgery: the current state of play. J Spine Surg 3(3): 433-443.
- Kim D, Lim JY, Shim KW, Han JW, Yi S et al. (2017) Sacral reconstruction with a 3D-printed implant after hemisacrectomy in a patient with sacral osteosarcoma: 1-year follow-up result. Yonsei Medical Journal 58(2): 453-457.
- McGilvray KC, Easley J, Seim HB, Regan D, Berven SH et al. (2018) Bony in growth potential of 3d-printed porous titanium alloy: a direct comparison of interbody cage materials in an in vivo ovine lumbar fusion model. The Spine Journal 18(7): 1250-1260.
- Fishbein M, Ajzen I (1975) Belief, attitude, intention, and behavior: An introduction to theory and research. Addison-Wesley, Reading MA.
- Ajzen I. (1985) From Intentions to Actions: A Theory of Planned Behavior. In: Kuhl J, Beckmann J (Eds.), Action Control. SSSP Springer Series in Social Psychology. Springer, Berlin, Heidelberg, pp. 11-39.
- Bandura A, Adams NE, Hardy AB, Howells GN (1980) Tests of the generality of self-efficacy theory. Cognitive Therapy and Research 4(1): 39-66.
- Davis FD (1986) A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results. Sloan School of Management, Massachusetts Institute of Technology.
- Escobar-Rodríguez T, Monge-Lozano P, Romero-Alonso M (2012) Acceptance of e-prescriptions and automated medication-management systems in hospitals: an extension of the technology acceptance model. Journal of Information Systems 26(1): 77-96.
- Venkatesh V, Davis FD (1996) A model of the antecedents of perceived ease of use: development and test. Decision Sciences 27(3): 451-481.
- Venkatesh V, Davis FD (2000) A theoretical extension of the technology acceptance model Four longitudinal field studies.pdf. Management Science 46(2): 186-204.
- Venkatesh V, Morris MG, Davis GB, Davis FD (2003) User acceptance of information technology: Toward a unified view. MIS quarterly 27(3): 425-478.
- Venkatesh V, Bala H (2008) Technology acceptance model 3 and a research agenda on interventions. Decision Sciences 39(2): 273-315.
- Lai PC (2017) The literature review of technology adoption models and theories for the novelty technology. Journal of Information Systems and Technology Management 14(1): 21-38.
- Terrizzi S, Susan SA, Meyerhoefer Chad, Scheinberg Michael, Donald L (2012) Extending the technology acceptance model in healthcare: identifying the role of trust and shared information. AMCIS 2010 Proceedings (19).
- Almeida J, Farias J, Carvalho H (2017) Drivers of the technology adoption in healthcare. Brazilian Business Review 14(3): 336-351.
- Strudwick G (2015) How can the technology acceptance model be applied to enhance infusion pump use by health care professionals? Vascular Access 9(1): 8-11.
- Hermes S, Riasanow T, Clemons EK, Böhm M, Krcmar H (2020) The digital transformation of the healthcare industry: exploring the rise of emerging platform ecosystems and their influence on the role of patients. Business Research 13: 1033-1069.
- Chismar WG, Wiley-Patton S (2003) Does the extended technology acceptance model apply to physicians. Proceedings of the 36th Hawaii International Conference on System Sciences.
- Porter CE, Donthu N (2006) Using the technology acceptance model to explain how attitudes determine Internet usage: The role of perceived access barriers and demographics. Journal of Business Research 59(9): 999-1007.
- Escarce JJ (1996) Externalities in hospitals and physician adoption of a new surgical technology: an exploratory analysis. Journal of Health Economics 15(6): 715-734.
- Gagliardi AR, Ducey A, Lehoux P, Turgeon T, Kolbunik J, et al. (2017) Multiple constraints compromise decision-making about implantable medical devices for individual patients: qualitative interviews with physicians. BMC Med Inform Decis Mak 17(1): 178.
- Moore GC, Benbasat I (1991) Development of an instrument to measure the perceptions of adopting an information technology innovation. Information Systems Research 2(3): 192-222.
- Davis FD, Bagozzi RP, Warshaw PR (1992) Extrinsic and intrinsic motivation to use computers in the workplace. Journal of Applied Social Psychology 22(14): 1111-1132.
- Parasuraman A (2000) Technology readiness index (TRI): A multiple-item scale to measure readiness to embrace new technologies. Journal of Service Research 2(4): 307-320.
- Burns LR, Housman MG, Booth RE, Koenig A (2009) Implant vendors and hospitals: competing influences over product choice by orthopedic surgeons. Health Care Management Review 34(1): 2-18.
- Davis FD, Bagozzi RP, Warshaw PR (1989) User acceptance of computer technology: a comparison of two theoretical models. Management Science 35(8): 982-1003.
- Taylor S, Todd PA (1995) Understanding information technology usage: a test of competing models. Information Systems Research 6(2): 144-176.
- Pallant J (2016) SPSS survival manual: A step-by-step guide to data analysis using SPSS program (6th edn), London, UK: McGraw-Hill Education.
- Hair JF, Hult GTM, Ringle C, Sarstedt M (2013) A primer on partial least squares structural equation modeling (PLS-SEM). Sage.
- Haenlein M, Libai B (2013) Targeting revenue leaders for a new product. Journal of Marketing 77(3): 65-80.
- Risselada H, Verhoef PC, Bijmolt THA (2014) Dynamic effects of social influence and direct marketing on the adoption of high technology products. Journal of Marketing, 78(2): 52-68.
- Ringle CM, Wende S, Becker JM (2015) "SmartPLS 3." Boenningstedt: SmartPLS GmbH.
© 2023 Naveen Donthu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






