- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Exploring the Relationship Between Blood Groups, Secretor Status, and Cardiovascular Disease in Northern Sudan
Mahjoub Mohammed RM1, Osman Ali M1, Mohammed Mahjaf G2, Abdien Saeed A1, Abdalmajed Altaher T3, Ahmed Osman RA3 and Nouraldein Mohammed Hamad M4*
1Department of Haematology, Faculty of Medical Laboratory Sciences, Shendi University, Sudan
2Department of Medical Microbiology, Faculty of Medical Laboratory Sciences, Shendi University, Sudan
3Department of Clinical Chemistry, Faculty of Medical Laboratory Sciences, Shendi University, Sudan
4Assistant professor, Microbiology department, Faculty of Medicine, Elsheikh Abdallah Elbadri University, Sudan
*Corresponding author: Mosab Nouraldein Mohammed Hamad, Assistant professor, Microbiology department, Faculty of Medicine, Elsheikh Abdallah Elbadri University, Sudan
Submission: July 11, 2025;Published: August 08, 2025

ISSN 2578-0204Volume5 Issue 1
Abstract
Background: Many recent reports suggest a link between blood groups and various manifestations of
heart disease. This is a cross-sectional, prospective, analytical study aimed at determining the frequency
of blood groups and secretor status among patients with cardiovascular diseases in Shendi locality from
August to December 2021.
Methods: Seventy patients with different types of cardiovascular diseases who attended ELmek-nimer
Hospital were enrolled. Informed consent was obtained from each patient before collecting blood samples
and saliva. ABO and secretor status were determined using slide techniques and tube methods with
specific antisera and indicator cells. Data were analyzed using the SPSS computer program.
Result: The results showed that the most common blood group among patients with cardiovascular
disease was O, followed by A, then B, with AB being the least frequent. The majority (65.7%) of these
patients were non-secretors. The most prevalent cardiovascular disease was more common in females
compared to males, and it was most frequently diagnosed in elderly patients aged 51-85 years. The most
common cardiovascular conditions included Dilated Cardiomyopathy and Coronary Artery Disease,
followed by ischemic heart disease, while the least frequent was a permanent pacemaker.
Conclusion: The frequency of Ischemic Heart Disease (IHD) was higher in the A group, and the frequency
of Dilated Cardiomyopathy (DCM) and Coronary Artery Disease (CAD) was higher in the O group. Finally,
the results of the present study showed that there is no association of ABO blood group and secretor
status with cardiovascular diseases.
Keywords:ABO; Cardiovascular diseases; Sudan; ABO blood group; Secretor status
Introduction to TTR Amyloidosis
Since the discovery of the ABO system in 1900, a multitude of blood group antigens have been identified and many different styles of terminology have been used. The International Society of Blood Transfusion (ISBT) recognizes 285 blood group antigens; 245 of these are classified into one of 29 blood group systems. Forty years later, both Landsteiner and Wiener discovered the Rh(D) antigen [1]. The genes of ABO and Rh(D) are located on chromosome 9 and 1 respectively. The bombardment of the red blood cells with A and /or B antigens occurs as a consequence of the action of the glycosyltransferase enzymes that add specific sugars to the precursor substance [2]. about 80% of the UK populations are ABH secretors as they have H antigen plus A or B according to their ABO genotype in body fluids such as saliva sweat, tears, serum and the gastrointestinal mucous secretions. The remaining 20% are non-secretors or weak secretors who have no or little antigen present in their body fluids. A recent paper suggests that individual ABO blood groups and secretor status are part of human’s innate immunity against infectious disease [3]. In addition, blood group was studied as a risk factor for many diseases like peptic ulcer, carcinoma of the stomach, periodontal disease, and diabetes mellitus. There is evidence that individual’s ABO group can predetermine the risk of thrombosis. However, significance of the association between the ABO blood group and IHD in the clinical practice is not yet known [4]. The cardiovascular system includes the heart and the blood vessels. A functional cardiovascular system is vital for survival because, without blood circulation, the tissues lack oxygen and nutrients, and wastes accumulate. Under such conditions, the cells soon begin irreversible changes, which quickly lead to death. Cardiovascular disease (also called heart disease) is a class of diseases that involves the heart, the blood vessels (arteries, capillaries, and veins), or both. This study aimed to determine the frequency of ABO blood groups and secretor status of cardio vascular patients and to correlate association of blood group with cardio vascular diseases.
Results of this study may be useful in determining which blood group system is more susceptible to cardiovascular diseases [5]. A blockage that stops blood flow to the heart or brain is the primary cause of cardiovascular diseases, which include heart attacks and strokes. These conditions are typically acute occurrences. The most frequent causes are blood clots or the accumulation of fatty deposits on the inner walls of blood vessels in the brain [5]. The heart and blood arteries are components of the cardiovascular system. Survival depends on a healthy cardiovascular system because, without blood flow, waste products build up and tissues lack oxygen and nutrients. In such circumstances, the cell rapidly becomes irreversible, which ultimately results in death. A kind of illness known as cardiovascular disease, or heart disease, affects the heart, the blood vessels (arteries, capillaries, and veins), or both [6]. The most frequent cause of chronic coronary artery disease is atherosclerotic plaque blockage of the coronary arteries. Patients with coronary artery disease do not initially have a consistent set of symptoms. In cases of acute myocardial infarction, Prinzmetal (variant) angina, microvascular angina, unstable angina, and chronic (stable) angina, chest discomfort is typically the main symptom [7].
Regarding ABO blood grouping in heart problems, we could only locate one study in Sudan. Reela A. Abdelraheem’s research, which was published in the University of Sudan for Science and Technology’s bibliographies, examined seventy individuals with various cardiovascular conditions to see if there was any correlation with blood grouping. Even though Ischemic Heart Disease (IHD) was more common in the O group, her findings indicated no correlation between cardiovascular illnesses and the ABO blood group or the Rh factor [8]. As far as we are aware, this is the only study in this setting that found no correlation between ABO grouping and CHD. However, they did not include healthy controls for comparison, and their sample size was tiny. In order to assess the frequency differences between CHD cases and controls, we therefore sought to enroll a sizable sample size as well as healthy controls.
Material and Methods
This was a cross-sectional prospective analytical study conducted in Shendi Locality, River Nile State, Sudan, from August to December 2021. The study aimed to determine the frequency of ABO blood groups and secretor status among Sudanese patients with Cardiovascular Diseases (CVD) and to investigate the association between ABO blood groups, secretor status, and CVD.
Study Area
The study was conducted in the Cardiac Care Unit (CCU) of Almek Nimir University Hospital in Shendi city. Shendi is a locality within the River Nile State, located approximately 172km north of Khartoum, Sudan. Situated in the southern part of the River Nile State, the city covers an area of about 30km². The main economic activities in the area are agriculture and service provision (commercial, social, education, and health services). Shendi city hosts Almek Nimir University Hospital and Shendi University, which includes faculties of Medicine and Health Sciences, Sciences and Technology, Arts, Economics, Education, among others.
Study population
Seventy (70) patients diagnosed with cardiovascular diseases, encompassing various age groups and both sexes (male and female), were included.
Inclusion criteria
Patients of different age groups diagnosed with cardiovascular diseases at Almek Nimir University Hospital in Shendi Locality were included in this study.
Exclusion criteria
Healthy individuals or patients with diseases other than cardiovascular diseases were excluded from this study.
Sample collection
Venous blood (2.5ml) was drawn after sterilizing the site with 70% alcohol. A 20 or 21 G needle was used with minimal occlusion of the arm by a tourniquet. Blood was collected in K₂EDTA (Potassium Ethylenediaminetetraacetic acid) tubes and mixed gently by inversion [9]. Saliva was collected in a sterile container.
ABO Slide Agglutination Test
When red blood cells are mixed with specific antisera, agglutination (clumping) occurs on slides containing cells possessing the corresponding antigen. No agglutination occurs if the cells lack the corresponding antigen [10]. Place one drop of anti-A antiserum on the slide section labeled “Anti-A”. Place one drop of anti-B antiserum on the slide section labeled “Anti-B”. Add one drop of the test cell suspension to each antiserum circle. Mix each solution carefully using a separate applicator stick. Tilt the slide gently back and forth for one minute and observe for agglutination. Record the results immediately. Agglutination (clumping) of red blood cells indicates a positive reaction. No agglutination indicates a negative reaction. Results must be read immediately to avoid false positives caused by drying. Known positive (+ve) and negative (-ve) red blood cell controls (cells known to possess or lack A and B antigens) were included following relevant quality assurance guidelines.
Rh (D) red blood cell typing
Rh (D) typing is based on direct agglutination. Red blood cells possessing the D antigen will agglutinate when mixed with anti-D serum. Agglutination of test cells with anti-D serum (and no agglutination with the control reagent) indicates a positive result (presence of D antigen). Absence of agglutination indicates a negative result (D antigen not demonstrable). If Rh typing is negative, Dᵘ (weak D) typing is automatically performed.
Dᵘ (Weak D) testing by Indirect Antiglobulin Test (IAT)
The Indirect Antiglobulin Test (IAT) is used to detect red cell sensitization by antibodies (like IgG anti-D) in vitro. If specific IgG antibodies and corresponding antigens are present, incubation causes the antibody to bind to antigenic receptors on the red cells. Subsequent addition of Antihuman Globulin (AHG) causes agglutination of sensitized cells. Place two drops of blended (IgG+IgM) anti-D serum into a 10×75mm test tube. Add one drop of a washed 5% suspension of the test red blood cells. Mix well and incubate the tube at 37 °C for 15 minutes in Low-Ionic-Strength Saline (LISS). After incubation, centrifuge the mixture, read the result macroscopically, and record it. Wash the cell mixture 3-4 times with a large volume of saline, decanting completely after each wash. Add two drops of antihuman globulin (AHG, Coombs’) reagent. Mix well. Incubate at room temperature for 4-5 minutes. Centrifuge at 3400rpm for 15 seconds. Read the final result macroscopically and/or microscopically and record.
Determination of Secretor Status
Soluble ABH blood group substances are present in secretions (e.g., saliva, gastric juice) in approximately 78% of the population (“secretors”; possessing the Se gene). These water-soluble antigens can neutralize their corresponding antibodies. This neutralization inhibits the antibody’s ability to agglutinate red blood cells possessing the corresponding antigen. This reaction, called hemagglutination inhibition, allows detection of soluble ABH substances and determination of secretor status.
Ethical Considerations
Ethical approval for the study was obtained from the Board of the Faculty of Medical Laboratories Sciences at SHENDI UNIVERSITY. The written informed consent form was obtained from each guardian of the participant as well as from the subject himself before recruitment into the study. All protocols in this study were done according to the Declaration of Helsinki (1964).
Data Analysis
Data were analyzed using SPSS 25.0, descriptive statistics in terms of frequency, percentages, means, and standard deviations, and the Chi-square test was calculated. A p-value≤0.05 is considered statistically significant.
Result
This was a cross sectional prospective analytical study aimed to determine frequency of ABO and secretor status blood groups in Sudanese patients and to correlate their association with cardiovascular diseases, this study done on seventy patients 33 (47.0%) males and 37 (53.0%) females. The results of this study showed that cardiovascular diseases have been found in females more than males, and also found in elderly patients aged between 51-85 years. According to the study found the most frequent duration of disease was less than 3 years (57.1%), followed by 4 to 7 years (24.3%), and the least frequent was more than 7 years (18.6%). The most common type of cardiovascular disease was coronary artery disease and dilated cardiomyopathy (20.0%), followed by ischemic heart disease (18.6%), and least frequent was permanent pacemaker (2.9%). The most common type of cardiovascular disease in females was IHD (18.9%), followed by DCM, then VHD (16.2%), and least frequent PPM (5.4%). The most common type of cardiovascular disease in males was CAD (27.3%), followed by DCM (24.2%), and least frequent PPM (0.0%). The results of the study revealed that the majority of patients with cardiovascular diseases were non-secretors (65.7%).
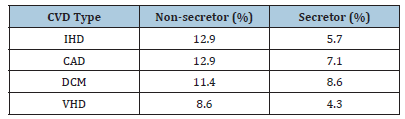
Most patients with DCM, CAD, HF, and MI were blood group O., while the patients with IHD and VHD were commonly blood group A. According to the result the frequent secretor in IHD was (5.7%) and non-secretor was (12.9%), in VHD secretor was (4.3%)and nonsecretor (8.6%), in RHD secretor was (0.0%) and non-secretor was (5.7%), in DCM secretor was (8.6%) and non-secretor was (11.4%), in CAD secretor was (7.1%) and non-secretor was (12.9%), in HF secretor was (4.3%) and non-secretor was (5.7%), in MI secretor was (2.9%), and non-secretor was (7.1%), and in PPM the secretor was (1.4%)and non-secretor was (1.4%). According to the results most frequent blood group in males was O phenotype (51.5%), followed by A phenotype (36.4%), then B phenotype (12.1%), and least frequency was AB (0.0%), while most frequent blood group in female was O phenotype (45.5%), followed by A (37.8%), then B phenotype (13.5%) and least frequency was AB (2.7%). According to the results of the study found that the most frequent blood group in the study was O phenotype (48.6%), followed by A phenotype (37.1%), then B phenotype (12.9%), and least frequent was AB phenotype (1.4%). Regarding gender, the results revealed that the secretor in males was (36.4%) and in females was (32.4), while the non-secretor in males was (63.6%) and in females was (67.6%) (Tables 1-6).
Table 1:Study population distribution.
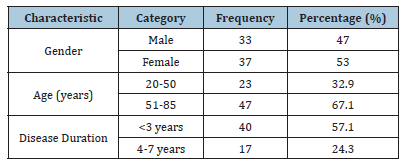
Table 2:CVD Types overall and by gender.
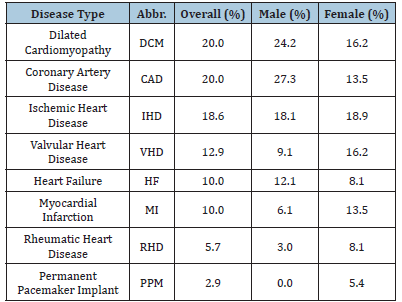
Table 3:ABO groups overall and by gender.
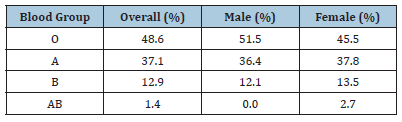
Table 4:Secretor status overall and by gender.
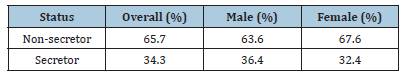
Table 5:ABO blood groups and CVD types.
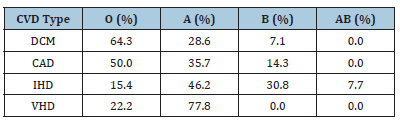
Table 6:Secretor status and CVD types.
Discussion
In recent years, numerous data have surfaced indicating a correlation between blood types and different cardiac disease symptoms. Numerous risk factors for coronary heart disease have been proposed. The ABO blood grouping is one of them [11]. According to World Health Organization (WHO) data, Cardiovascular Diseases (CVDs) are and remain the leading causes of death globally: an estimated 17.3 million people died from CVD in 2008, representing 30% of all global deaths (WHO Media Centre 2011), cardiovascular diseases [12]. This is a cross section prospective analytical study was conducted in Shendi locality during the period from August to December 2021 to determine frequency of ABO and secretor status blood groups in Sudanese patients and to correlate their association with cardiovascular diseases. Regarding the association of cardiovascular disease with blood group the results obtained in this study showed that the prevalence of blood group O was higher in patients with Dilated Cardio Myopathy (DCM), rather than other ABO blood groups, that may be due to high prevalence of blood group O in Sudanese population, similar to the results of study done by Fathelrahman [13], which concluded that blood group O was the predominant in Sudanese population. Statistical analysis of this study revealed that there was a high frequency of the O blood group in patients with coronary heart disease.
This result was similar to the results of a study done in Bangladesh by Biswas J et al. [14], which showed the prevalence of Coronary Artery Disease (CAD) was higher in blood group O than in other blood groups. Also, this result was not similar to the results of a study conducted by Wazirali et al. [15], which concluded that phenotype A is associated with substantially increased risk for coronary heart disease. Also, these results agree with the results of a study conducted by Whincup et al. [16], which found that blood group A are associated with higher risk of ischemic heart disease as compared to group O. Also, these results were agreed with the results of study done in Pakistan by Wazirali et al. [15] & Khan et al. [17], which found a strong association of ischemic heart disease with blood group A as compared with other blood group. Also, the results of this study were not similar to the results obtained in the UK by Meade et al. [18], which found that the incidence of ischemic heart disease is significantly highest in patients with blood group phenotype AB than in those with groups O, A, or B. Regarding to statistical analysis of results of the ABO and secretor status in CVD found that the A blood group associated with IHD and nonsecretor patients more than secretor this study not similar previous study done by Swapnali et al. [19] showed the prevalence of IHD was higher in blood group O, (74%) was secretor and (26%) nonsecretor [19]. Finally, the results obtained from this study found that there was no association between cardiovascular disease and the type of blood groups, with a p-value of 0.06.
Conclusion
n this cohort, CVDs showed no significant association with ABO blood groups, despite blood group O being most prevalent (48.6%). Non-secretors dominated (65.7%), and gender-specific patterns emerged: CAD was the primary CVD in males (27.3%), while IHD led in females (18.9%). Overall, CVDs were more common in females (53%), with DCM and CAD as the most frequent types (20.0% each) and PPM the rarest (2.9%).
Recommendations
1. Further study is required to give baseline data regarding
distribution of ABO of patients with cardiovascular diseases
2. Individuals with blood group O and A should be aware of
preventive measures against cardiovascular disease, including
diet and physical exercise
3. Other studies should be conducted using advanced techniques
such as the gel technique to confirm the results.
4. Further investigations in other regional settings with much
larger populations may elucidate these findings.
5. 5-Researchs on normal distribution of ABO blood group
system among Sudanese people should be done to establish
data base program.
References
- Garraty G, Dzik W, Issitt PD, Lublin DM, Reid ME, et al. (2000) Terminology for blood group antigens and genes, historical origins and guideline in the new millennium. Transfusion 40(4): 471-489.
- John DR (1996) Technical manual of American association of blood banks. (12th edn), American Association of Blood Banks USA, pp. 373-387.
- Hoff Brand AV, Lewis SM, Tuddewhan EGD (2000) Post graduate Heamtology, (4th edn), British Library, London, UK.
- Clark P, Meiklejohn DJ, O'Sullivan A, Vickers MA, Greaves M (2005) The relastionships of ABO Lewis and secretor blood groups with cerebral ischemia of arterial origin. J Thromb Haemost 3(9): 2105-2108.
- Kelly BB, Fuster V (2010) Promoting cardiovascular health in the developing world: A critical challenge to achieve global health. National Academies Press, Washington DC, USA.
- Abo Algasim El, Malik H, Tarq E (2007) Sequences of ABO, Rh-D and kell blood group antigen in dinka. Sudanese Ethnic Group.
- He M, Wolpin B, Rexrode K, Manson JE, Rimm E, et al. (2012) ABO blood group and risk of coronary heart disease in two prospective cohort studies. Arteriosclerosis, Thrombosis, and Vascular Biology 32(9): 2314-2320.
- Reela AE (2012) Determination of ABO blood groups and rhesus factor in Sudanese patients with cardiovascular disease. Library of the Sudan University of Science and Technology (SUST), Sudan.
- Kathen EB, Barbara ED, Lincon PJ (1988) Blood group serology, (6th edn), Churchill Livingstone, Scotland, pp. 39-88.
- Walker RH, Hoppe PA, Judd WJ (1999) Technical manual, (3rd edn), American Association of Blood Banks, Arlington, Texas, USA, pp.197-223.
- Ali EH, Hassan HM, Alkheder RIH, Al-Tyeb MH, Bushra AA, et al. (2019) ABO and rhesus grouping among sudanese patients with coronary artery disease at Sudan heart center-Khartoum state. EC Emergency Medicine and Critical Care 4: 01-12.
- B Woolf (1955) On estimating the relation between blood group and diseases. Annals of Human Genetics 19(4): 251-253.
- Hassan FM (2010) Frequency of ABO, sub group ABO and Rh (D) blood groups in major sudanese ethnic groups. Pak J Med Res 49(1).
- Biwas S, Ghoshal PK, Halder B, Mandal N (2013) Distribution of ABO blood group and major cardio vascular risk factor with coronary heart disease. Biomed Res Int 2013: 782941.
- Hafeezullah W, Ashfaque RA, Herzig JW (2005) Association of blood group A with increased risk of coronary heart disease in the Pakistani population. Pak J Physiology 1(1-2).
- Whincup PH, Cook DG, Phillips AN, Shaper AG (1990) ABO blood group and ischaemic heart disease in British men. BMJ 300(6741): 1679-1682.
- Khan IA, Farid M, Qureshi SM, Chaudray MA (2005) Relationship of blood group A with ischemic heart disease. Pakistan J Med Res 44(4): 159-160.
- Meade TW, Cooper JA, Stirling Y, Howarth DJ, Ruddock V, et al. (1994) Factor VIII, ABO blood group and the incidence of ischaemic heart disease. Br J Haematol 88(3): 601-607.
- Swapnali, Kisan R, Bharadwaj NA (2014) Study of ABO blood group and secretor status in ischemic heart disease patients in and around davangere. International Journal of Pharmacy and Biological Sciences 4(1): 75-78.
© 2025 Nouraldein Mohammed Hamad M . This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






