- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Yasser’s Triple Discoloration Sign in Hall- Hittner Syndrome Post-Recent Successful Ablation of WPW Syndrome and Neonatal Closure of PDA-A New Diagnostic Sign and Interpretation
Yasser Mohammed Hassanain Elsayed*
Critical Care Unit, Kafr El-Bateekh Central Hospital, Damietta, Egyptian Ministry of Health (MOH), Egypt
*Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Kafr El-Bateekh Central Hospital, Damietta, Egyptian Ministry of Health (MOH), Egypt
Submission: August 20, 2024;Published: November 14, 2024

ISSN 2578-0204Volume4 Issue4
Abstract
Introduction: Hall-Hittner syndrome and its synonym; CHARGE syndrome is described as neurocristopathy
with mutations in CDH7. Major and minor criteria are included in the diagnosis of CHARGE syndrome or
Hall-Hittner syndrome. Wolff-Parkinson-White (WPW) syndrome is a common pattern of pre-excitation
with abnormal Accessory Pathways (AP). Patent ductus arteriosus is a frequent congenital cardiac defect
due to a delay in the closure of the ductus arteriosus of birth.
Case presentation: A young mentally retarded student female girl patient presented to the physician
outpatient clinic for periodic follow-up in previously published and diagnosed (CHARGE syndrome
hallmarked with Wolff-Parkinson-White syndrome and patent ductus arteriosus; 20 years post-repairing
is an extreme combination). Ablation of accessory pathway, ECG, echocardiography and duplex ultrasound
were the interventions.
Conclusion: The “Yasser’s triple discoloration sign (Triple color sign)” in Hall-Hittner syndrome
post-recent successful ablation of WPW syndrome and neonatal closure of PDA is a new diagnostic
dermatological and cardiovascular sign. The mechanism of “Yasser’s triple discoloration sign (Triple
color sign)” is still not understood despite the suggested theories. The evidence of previously described
infantile ECG Tee-Pee signs of hypocalcemia and adult low-ionized calcium may be a guide for associated
DiGeorge syndrome. With the entrance of this new Sign (S), the old Mnemonic (CHARGE) syndrome can
be modified to CHARGES syndrome by adding the letter (S) to it. Furthermore, future research will be
recommended.
Keywords:Hall-hittner syndrome; Charge syndrome; Wolff-parkinson-white syndrome; Accessory pathway patent ductus arteriosus; Digeorge syndrome; Genetic syndromes; Yasser’s triple discoloration sign; Triple color sign
Abbreviations:AP: Accessory Psathway; CBC: Complete Blood Count; CHARGE Syndrome: Coloboma, Heart Defect, Atresia Choanae, Retarded Growth And Development, Genital Hypoplasia, and Ear Anomalies/Deafness; CHARGES Syndrome: Coloboma, Heart Defect, Atresia Choanae, Retarded Growth and Development, Genital Hypoplasia, Ear Anomalies/Deafness, and Yasser’s Triple Discoloration Sign; DA: Ductus Arteriosus; ECG: Electrocardiography; PA: Pulmonary Artery; PD: Patent Ductus; PDA: Patent Ductus Arteriosus; POC: Physician Outpatient Clinic; SGOT: Serum Glutamic-Oxaloacetic Transaminase; SGPT: Serum Glutamic-Pyruvic Transaminase; VR: Ventricular Rate; WPW syndrome: Wolff-Parkinson- White Syndrome
Introduction
Hall-Hittner Syndrome is a synonym for CHARGE syndrome which was described as a nonrandom group of anomalies: coloboma of the eye, heart defects, atresia of the nasal choanae, retardation of growth or development, genital or urinary abnormalities, ear abnormalities and deafness [1-3]. It is an autosomal dominant disease affecting 1:10,000 births [1,2] that was first described as a recognizable pattern of congenital malformations by Hall in 1979 [2]. About 65% is due to mutations in CDH7, which is an ATP-dependent chromatin remodeler gene [1]. It was originally assumed to be a neurocristopathy direct evidence using hESCs and their differentiation to NCC. This syndrome is a typical example of how pluripotent stem cells have been used to gain a deeper insight into the molecular basis of idiopathic conditions [1]. Diagnostic criteria for the diagnosis of CHARGE syndrome were summarized by Blake et al in 1998 [3] and were classified into the major (the classical 4C’s: Choanal atresia, Coloboma, Characteristic ears, and Cranial nerve anomalies) and minor criteria. Minor criteria include cardiovascular malformations, pubertal delay, orofacial cleft, characteristic face, growth deficiencies, and developmental delay.
Patients who have all four major criteria or three major and three minor criteria are strongly likely to have CHARGE syndrome [4]. A definitive diagnosis of CHARGE syndrome is established when all four major characteristics or three major and three minor characteristics are identified in an individual. The diagnosis is considered if one or two major and several minor characteristics are identified in an individual [2]. Wolff-Parkinson-White (WPW) syndrome is a congenital cardiac preexcitation syndrome that arises from abnormal cardiac electrical conduction through an Accessory Pathway (AP) that can result in symptomatic and fatal arrhythmias. The ECG hallmark of WPW syndrome includes a short PR interval and prolonged QRS with an initial slurring upstroke (delta wave) in the presence of Normal Sinus Rhythm (NSR). The most frequent clinical presentations are palpitations, episodic lightheadedness, presyncope, syncope and even cardiac arrest. The AP is typically comprised of myocardial tissue and usually has nondecremental or non-delayed conduction allowing for immediate ventricular activation. This non-decremental conduction property predisposes patients with WPW syndrome to Sudden Cardiac Death (SCD). Asymptomatic patients (at low risk of cardiac arrest) with WPW patterns do not require urgent treatment. Patients deemed to be at high risk may benefit from preventative antiarrhythmic medications or prophylactic accessory pathway ablation depending on their level of risk, the type and characteristics of the pathway, their cardiac comorbidities and other medical conditions [5]. The 2015 ACC/AHA/HRS guidelines indicate that in asymptomatic patients with WPW patterns, EP study is reasonable, and ablation is reasonable for accessory pathways found to be either at high risk or in patients with high-risk occupations [6]. Patent Ductus Arteriosus (PDA) is a congenital anomaly with persistent connection between the aorta and the Pulmonary Artery (PA) [7].
PDA in the fetus connects the proximal descending aorta with the proximal left PA. Normally this close soon after birth. If the PD does not spontaneously close, there is a continuous flow from the aorta to the PAs [8]. PDA with a murmur and significant left-to-right shunting should be closed at any age before the establishment of irreversible pulmonary hypertension [7]. A PDA is rare in healthyterm newborns. As gestational age decreases, the incidence of PDA increases. In extremely premature infants, especially those with respiratory distress syndrome, up to 80% may have a PDA at 3 days of age. There are some genetic conditions and associated risk factors with PDA: Trisomy 13, 18, 21, Holt-Oram, Noonan, CHARGE, TAAD/ PDA, DiGeorge, familial PDA, prematurity, surfactant deficiency, congenital rubella syndrome, Loeys-Dietz syndrome, Wiedemann- Steiner syndrome, and Fetal Alcohol Spectrum Disorder [8-11]. Most adult patients with PDA have asymptomatic lesions diagnosed by the discovery of a murmur [8]. Transcatheter device closure of PDA is now the procedure of choice and surgery s only performed if the percutaneous method is unsuccessful [7].
Case Presentation
History
A 22-year-old student a single young female Egyptian patient presented to the Physician Outpatient Clinic (POC) for periodic follow-up with no complaint. Her mother gave a history of patent ductus arteriosus since 3mo. after developing acute respiratory distress syndrome and severe pulmonary hypertension repaired on 11mo. [12]. The mother gave a history of difficulty in learning, intellectual defects, blurred vision, hearing defects, intermittent mucus nasal discharge, intermittent nasal obstruction, growth retardation, amenorrhea and hypogonadism [12]. There is no history of the above tachycardia after PDA repair until two years ago (at the age of 20 years) [12]. Informed consent was taken from her father.
Physical examination
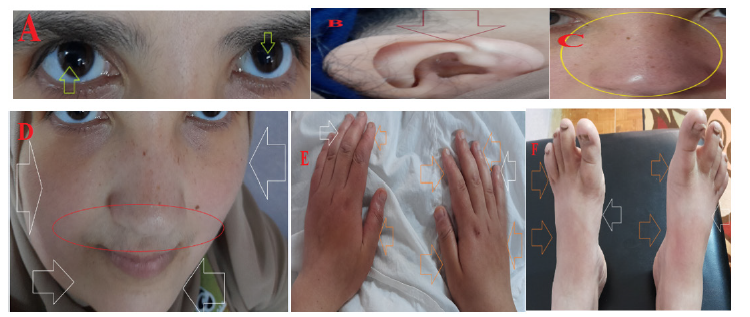
Upon updated physical examination, generally, the patient was infantile, had small eyes, hypertelorism, abnormal ears, coloboma in both eyes and Khnf sound (Figure 1A-C)., with a regular pulse rate (VR of 70), Blood Pressure (BP) of 130/70mmHg, respiratory rate of 14bpm, a temperature of 36 °C and pulse oximeter of Oxygen (O2) saturation of 99%. Tests for provocative latent tetany were positive. There are three fixed non-blanching colors appearing on the face, hands and feet (Figure 1D-F). The three-color sign is described according to both the “Monk Skin Tone Scale” and the “Skin tone color palette” as (C-A-C) or (Honey-Pale ivory -Honey). No more relevant clinical data were noted during the clinical examination.
Figure 1:Multiple recent images of the patient showing Infantile facies, small eyes, hypertelorism, coloboma in both eyes (A), abnormal ears (B), and Khnf sound (C). There is triple non-blanching discoloration (Honey-Pale ivory -Honey) on the face, hands, and feet (D-F).
Investigations and management
Within two years before ablation, the patient started to sense of recurrent palpitation with no recorded ECG tachycardia. Planning for catheter ablation was done. Before repairing PDA, the patient had a recurrent neonatal history of paroxysmal supraventricular tachycardia (PSVT of VR; 164bpm) with evidence of WPW syndrome (Figure 2A). The ECG tracings were done within 2 years before (Figure 2B) and just before catheter ablation (Figure 2C) and showed evidence of WPW syndrome with no PSVT. The echocardiography done before catheter ablation showed observed dyssynchrony between the septal wall and inferior walls (Figure 3A). The successful ablation was applied 2 years ago (Figure 2B). The echocardiography was repeated after catheter ablation and showed the disappearance of the above dyssynchrony between the septal wall and inferior walls (Figure 3C). Recent arterial duplex ultrasound (Figure 3D) and venous (Figure 3E) for lower limbs were within normal. The ECG tracing was done within 2 years after catheter ablation and showed NSR with no evidence of WPW syndrome (Figure 2D). The current Complete Blood Count (CBC), SGPT, SGOT, serum creatinine, urea and RBS were within normal. Ionized calcium was low (7.14 mg/dl). “Yasser’s triple discoloration sign (Triple color sign)” in Hall-Hittner syndrome post-recent successful ablation of WPW syndrome and neonatal closure of PDA was the most probable diagnosis. Oral calcium and vitamin D preparation for 30 days were prescribed with further recommended cardiac and endocrinologist follow-up.
Figure 2:A-ECG tracing was taken on the 2.5mo. of life (since 20 years) and before PDA repair showing paroxysmal supraventricular tachycardia (of VR: 168), short PR-interval (parallel blue line and lime arrow), wide QRS (dark blue arrow), delta wave (white arrow) of evidence of WPW syndrome (white circle), ST-segment depression (light blue arrows), T-waves inversion (green arrows) and LAD (yellow arrows). B-ECG tracing was done within 2 years before catheter ablation showing NSR (of VR: 83), short PR-interval (parallel green lines), wide QRS (parallel blue lines), delta wave (lime arrows) of evidence of WPW syndrome (light blue circle), T-waves inversion (yellow arrows) and LAD (golden arrows). C-ECG tracing was done within just before catheter ablation showing NSR (of VR: 77) with the same above changes. D-ECG tracing was done within 2 years after catheter ablation showing NSR (of VR: 69) with the same above changes.
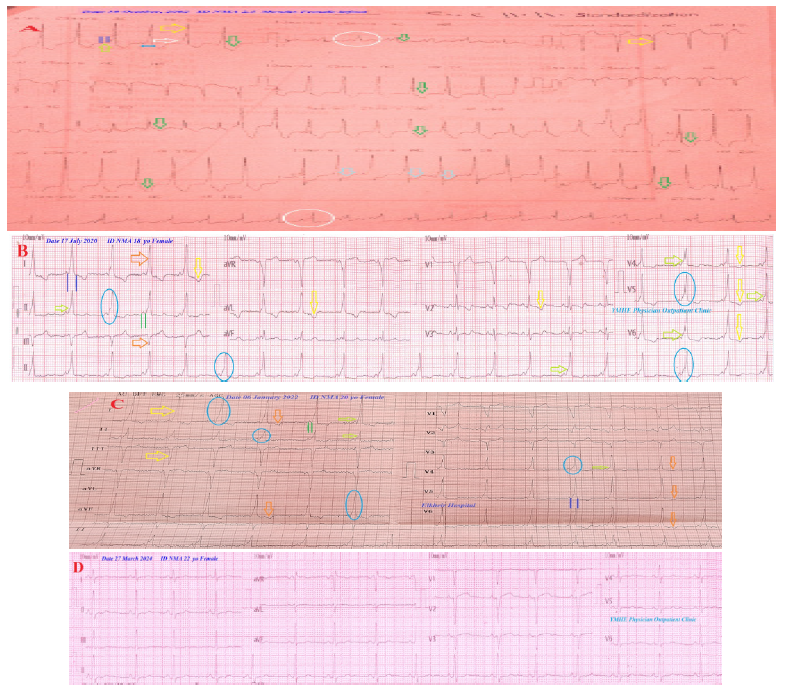
Figure 3:The echocardiography done before catheter ablation showed observed dyssynchrony between the septal wall and inferior walls (light blue and lime arrows) with evidence of delta wave (orange circle) (A). The successful ablation (lime arrow) was applied within 2 years ago (B). The echocardiography was repeated after catheter ablation and showed the disappearance of the above dyssynchrony between the septal wall and inferior walls (light blue and lime arrows) (C). Recent arterial duplex ultrasound (D) and venous (E) for lower limbs was within normal.

Discussion
A. Overview: A young mentally retarded student female girl
patient presented to the physician outpatient clinic for periodic
follow-up in a previously published and diagnosed (CHARGE
syndrome hallmarked with Wolff-Parkinson-White syndrome
and patent ductus arteriosus [12]).
B. The primary objective for my case study was the presence
of the new “Yasser’s triple discoloration sign (Triple color
sign)” in Hall-Hittner syndrome post-recent successful ablation
of WPW syndrome and neonatal closure of PDA.
C. The secondary objective for my case study was the
question of how you manage the case.
D. The presence of Infantile facies, coloboma (small eyes
with blurred vision), hypertelorism, heart defects (PDA), atresia
of the choanae (Khnf sound, intermittent nasal obstruction, and
mucus nasal discharge), retardation (of growth, intellectual,
and learning), genital defects (hypogonadism, amenorrhea)
and ear anomalies (diminished hearing) are parallel with a
diagnosis of Hall-Hittner or CHARGE syndrome.
E. The existence of previously infantile T-wave alternate
may reflect the efficacy of PDA repairing and the existence of
previously described infantile ECG Tee-Pee sign of hypocalcemia
and adult low-ionized calcium in charge is an interesting [12].
F. The evidence of previously described infantile ECG Tee-
Pee sign of hypocalcemia [12] and adult low ionized calcium
may be a guide for associated DiGeorge syndrome.
G. Colorism (privileging of lighter over darker skin) affects
development across the lifespan [13].
H. The new “Yasser’s triple discoloration sign (Triple color
sign)” is a newly described associated sign.
I. There are three fixed non-blanching colors appearing on
the face, hands and feet (Figure 1D-F). A Slight color change is
happening during winter.
J. The three colors described according to both the Monk
Skin Tone Scale and the Skin tone color palette [14,15] which
was used for the color verification (Figure 4).
K. The three colors were (C-A-C) or (Honey-Pale ivory
-Honey).
Figure 4:Showing the Monk Skin Tone Scale (MST).
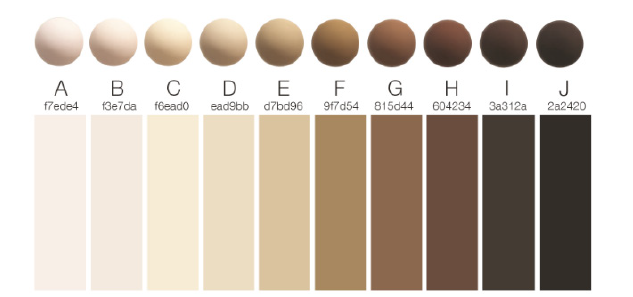
L. Skin shade Massey and Martin scale and colorimetric
scale for skin of color were not suitable for application [16-18].
M. The mechanisms of the presence of the three colors in the
Yasser’s triple discoloration sign are unknown.
N. Hyperemic fixed grading capillary changes and certain
chemical precipitation are suggested interpreted theories.
O. Normal arterial duplex ultrasound (Figure 3D) and venous
(Figure 3E) for lower limbs will reliably exclude peripheral
vascular disease.
P. I can’t compare the current case with similar conditions.
There are no similar or known cases with the same management
for near comparison.
Q. The author confirms that “Yasser’s triple discoloration
sign (Triple color sign)” is new and there were no similar signs
described in the literature.
R. The only limitation of the current study was the
unavailability of skin biopsy.
Conclusion and Recommendation
a) “Yasser’s triple discoloration sign (Triple color sign)” in
Hall-Hittner syndrome post-recent successful ablation of WPW
syndrome and neonatal closure of PDA is a new diagnostic
dermatological and cardiovascular sign.
b) The mechanism of “Yasser’s triple discoloration sign
(Triple color sign)” is still not understood despite the suggested
theories.
c) The evidence of previously described infantile ECG Tee-
Pee signs of hypocalcemia and adult low-ionized calcium may
be a guide for associated DiGeorge syndrome.
d) With the entrance of this new Sign (S), the old Mnemonics
(CHARGE) syndrome can be modified to CHARGES syndrome
by adding the letter (S) to it.
e) Furthermore, future research will be recommended.
References
- Avery J, Menendez L, Cunningham ML, Lovvorn HN, Dalton S (2014) Chapter 21-using induced pluripotent stem cells as a tool to understand neurocristopathies. Neural Crest Cells, Academic Press, pp. 441-459.
- Longman RE (2018) 126-Charge syndrome, obstetric imaging: fetal diagnosis and care. In: (2nd edn), Elsevier, pp. 541-543.
- Potter A, Phillips JA, Rimoin DL (2013) Chapter 83-genetic disorders of the pituitary gland. Emery and Rimoin's Principles and Practice of Medical Genetics. In: (6th edn), Academic Press, pp. 1-37.
- Blake KD, Prasad C (2006) Charge syndrome. Orphanet J Rare Dis 1(34).
- Chhabra L, Goyal A, Benham MD (2023) Wolff-Parkinson-White Syndrome. Treasure Island (FL), StatPearls Publishing, USA.
- Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, et al. (2016) ACC/AHA/HRS Guideline for the management of adult patients with supraventricular tachycardia: A Report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. Circulation. 133(14): e506-574.
- Khajali Z, Saedi S (2022) Chapter 33-congenital heart disease. Practical Cardiology. In: (2nd edn), Elsevier, pp. 607-633.
- Hughes D, Siegel MJ (2010) Computed tomography of adult congenital heart disease. Radiologic Clinics of North America 48(4): 817-835.
- Gillam M, Mahajan K (2023) Patent ductus arteriosus, Treasure Island (FL), StatPearls Publishing, Florida, USA.
- Anilkumar M (2013) Patent ductus arteriosus. Cardiol Clin 31(3): 417-430.
- Yap J (2022) Patent ductus arteriosus.
- Elsayed YH (2021) Charge syndrome hallmarked with wolff-parkinson-white syndrome and patent ductus arteriosus; 20 years post-repairing; An extreme combination. International Journal of Healthcare and Medical Sciences 7(3): 26-30.
- Cohen PR, DiMarco MA, Geller RL, Darrisaw LA (2023) Colorimetric scale for skin of color: A practical classification scale for the clinical assessment, dermatology management, and forensic evaluation of individuals with skin of color. Cureus 15(11): e48132.
- Monk E (2023) The Monk Skin Tone Scale, pp. 1-3.
- Courtney MH, Ellis PM, Alan TC, Candice S, Xango E, et al. (2024) Which skin tone measures are the most inclusive? an investigation of skin tone measures for artificial intelligence. ACM Journal on Responsible Computing 1(1): 1-21.
- Khan MA, Nguyen H, Branigan AR, Gordon RA (2023) How well do contemporary and historical skin color rating scales cover the lightness-to-darkness continuum? Descriptive results from color science and diverse rating pools. Research in Human Development 20(3-4): 106-122.
- Rosenblum A, Darity W, Harris AL, Hamilton TG (2015) Looking through the shades: the effect of skin color on earnings by region of birth and race for immigrants to the United States. Sociology of Race and Ethnicity 2(1): 87-105.
- Douglas SM, Charles CZ, Lundy G, Fischer MJ (2003) The source of the river: The social origins of freshmen at America's selective colleges and universities. Princeton University, Princeton, USA.
© 2024 Yasser Mohammed Hassanain Elsayed. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






