- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Pressure, Damping and Ventricularization
Nuray Kahraman Ay*
Department of Cardiology, Bezmialem Vakif University, Turkey
*Corresponding author: Nuray Kahraman Ay, Department of Cardiology, Bezmialem Vakif University, Adnan Menderes Boulevard (Vatan Street ) 34093 Fatih/ Istanbul, Turkey
Submission: February 16, 2018; Published: February 21, 2018
ISSN: 2578-0204 Volume1 Issue4
Abstract
The arterial pressure waveform to be included during coronary angiography makes procedure safer. At this point the sentience of angiographer, detection and evaluation of abnormal pressure waves, will ensure the avoidance of complications that may occur In this article, coronary pressure waveforms, the mechanisms of damping and ventricularization and precautions have been presented
Keywords: Pressure; Damping; Ventricularization
Introduction
Pressure
Although the risks of coronary angiography have declined over the years by increased clinical experience and advanced technologies, it still requires attention, knowledge and experience due to being an interventional diagnostic method. A safe coronary angiography begins with the selection of the appropriate catheter for the anatomical structure of the patient and the evaluation of the pressure when the catheter is placed in the coronary ostium. Coronary pressure waves are complementary requirements of angiography. The recognition, evaluation and precautions to be taken for abnormal pressure waves directly affect the mortality of the patient.
One of the first clues to the presence of stenosis in the left main coronary artery (LMCA) is abnormal changes in pressure when the catheter is seated in the ostial LMCA. This often occurs as a "ventricularization" or "damping". For decades, ventricularization was mostly experienced as a stenosis by invasive cardiologists [1]. Recognition of abnormal changes in pressure and precautions to be taken prevent catastrophic outcomes in patients.
Damping
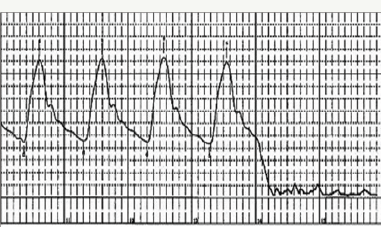
Damping can be defined as a significant decrease in the aortic pressure of the aortic root occurring when the catheter is placed in the coronary ostium accompanied with the disappearance of systolic and diastolic waveforms (Figure 1). At that moment, there is no pressure which means that there is no antegrade flow into the artery and that the area fed by the relevant artery cannot get blood. This suggests that either the size of the catheter used may be the same with the ostium of the vessel, or a catheter-related spasm has developed. The coronary ostium may have narrowed due to a lesion or the patient's artery may be anatomically thin. It is also possible that the catheter has occluded the vessel, blocking the blood flow. Arrhythmia, chest pain, and ischemia may occur if the catheter is not withdrawn quickly. It is very important for the operator to check the pressure as soon as possible after placing the catheter in the coronary ostium. Sometimes, the catheter is not properly placed in the ostium and leans on the vessel wall, which may potentially cause a decrease in the pressure. However, the waveform can be easily distinguished from that of actual damping
Figure 1: Aortic pressure and damping.
It is essential to choose an appropriate catheter for the anatomical structure of the patient for both ensuring a safe coronary angiography procedure and obtaining good image quality. Factors such as aortic root, structure of the aortic arch, anatomy of the coronary artery (transfemoral or transradial; right or left), body shape and catheter aid should be taken into account while selecting the catheter to be used. Choosing the appropriate catheter facilitates the operator's work and reduces the likelihood of complications.
A wide lumen catheter provides better support and image quality. Besides, it allows the passage of multiple balloon a guiding catheter for intravascular ultrasound (IVUS). Nevertheless, larger catheters have higher risk for vascular complication and damping induced by the blockage of antegrade perfusion. If the vessel is small in diameter and the catheter is larger than the vessel ostium, a side-hole catheter should be preferred [2]. Using a side- hole large catheter not only decreases damping, but also lowers the risk for vessel dissection that may be induced by contrast agent injection. On the other hand, in cases when a side-hole catheter is used, the opaque material may leak into the aortic root through the holes of the catheter, causing suboptimal visualization of the artery. It is not recommended to use side-hole catheters when the fractional flow reserve (FFR) technique is used as it may cause overestimation [2].
In general, pressure changes associated with arteriovenous malformation, subselective engagement of the catheter into the conus branch, and coronary artery spasm induced by catheter placement are more common in the right coronary artery [1]. The catheter-induced spasm may not only be at the point of catheterization, but also at the distal region. Changing the catheter to a smaller one and not sitting deep in the coronary ostium may be solve the problem. Infusion of intracoronary nitroglycerin 100- 200|ig can help to remove spasm.
Especially in the presence of ostial stenosis, it is important that the left coronary catheter is placed carefully and slowly in the ostium of the left main coronary artery (LMCA) The operator should check the press, if damping is observed, give as little as 1-2ml of opaque material during cineangiography and withdraw the catheter quickly (hit and run). In this way, the first image of the ostial stenosis can be obtained. It may be possible to evaluate the ostial stenosis of LMCA if contrast agent is given in anteroposterior (AP) or right anterior oblique (RAO) position when the catheter is behind the ostium [3]. Entering and exiting of the catheter to the ostium and contrast jet can increase spasm and stiffness. A LMCA stenosis between 40-60% may require more images for evaluation, and IVUS can be used to assess the stenosis in some cases.
Ventricularization
Suppose that you take a deep breath and inflate a balloon. Then, you inspire the air from the balloon again and inflate the balloon for the second time with the same air. Despite pressure changes, there is no new air inflow into the balloon. Similarly, ventricularization occurs when the coronary artery does not receive freshly oxygenated blood and the same blood circulates within the artery like in a closed system. Ventricularization is the deformation of the aortic pressure passing through the narrowed coronary artery. Pacold et al. [4] observed alterations in the intracoronary arterial pressure at various levels in 20 patients diagnosed with ventricularization. Also, an alteration was observed in the pressure waveforms when the stenosis of variable degrees was formed with a balloon-tip catheter in the left main coronary artery on an animal model.
In case of aortic or ostial stenosis, the rate of pressure decrease in the left main coronary artery varies depending the degree of the stenosis [1]. Not only LMCA stenosis but also complete blockage of the ostium by the catheter and deep or subselective engagement of the catheter in a blocked coronary branch can result in ventricularization. Additionally, a stenosis in the right coronary artery (RCA) may also cause ventricularization. Such a change is more significant when accompanied by the stenosis of the left main coronary artery or severe left coronary arterial stenosis. Placing the catheter in a narrowed coronary ostium reduces both systolic and diastolic pressures. The decrease in diastolic pressure, however, is sharper (Figure 2).
Figure 2: Ventricularization, during which aortic and systolic pressures mildly decrease while diastolic pressure significantly lowers.
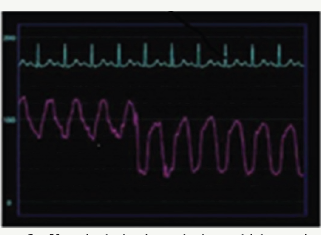
Sometimes, a catheter may enter the left ventricle during catheter manipulation. In such a case, during which ventricular pressure is observed, catheter is re-manipulated by pulling the catheter in the aortic root. Ventricularization is distinguished from actual ventricular pressure with its some characteristics. Left ventricular systolic pressure is equivalent to aortic pressure, whereas diastolic pressure is significantly lower (<20mmHg) [1]. In ventricularization morphology, there is pre-systolic deviation difference, and ventricularization resembles to the "a wave" corresponding the atrial systole. The ascending pressure curve of the ventricularization wave is slower compared to the aortic pressure while and its descending curve is steeper [1].
In case of pressure ventricularization, evaluation is performed by pulling the catheter into the aortic root. Subsequently, catheter is carefully placed back into the coronary ostium and image can be obtained with a small amount of opaque material by mildly pulling the catheter back during cineangiography. The fact that the test doses administered do not go back into the aortic root or that the contrast agent accumulate in the proximal and mid regions of the vessel refers to ostial stenosis. As with damping, it is possible with another approach to prevent ventricularization and damping through nonselective assessment of the ostial lesion at the level of sinus valsalva or by ensuring the preservation of antegrade flow through the replacement of a standard catheter with a side-hole catheter [5].
Conclusion
In conclusion, in ventricularization and damping cases which may have resulted from causes such as selection of catheter incompatible with coronary ostium, ostial stenosis, coronary spasm and catheter instability, repetitive injections that can lead to ventricular fibrillation or dissection in proximal of the coronary artery should be avoided. In such cases, major ischemic sequelae or catastrophic outcomes can be avoided through various solutions including the withdrawal of the catheter to the aortic root while administering a small amount of opaque material during cineangiography, replacement of the catheter with a new catheter compatible with the anatomical structure of the artery, use of a side-hole catheter, non-selective imaging of the aortic root, intracoronary nitroglycerin injection, and proper placement of the catheter into the coronary ostium.
References
- Kern MJ (1999) Coronary Hemodynamics Section I: Coronary catheter pressures. Hemodynamic Rounds: Interpretation of cardiac pathophysiology from pressure waveform analysis. (2nd edn), Wiley Liss, New York, USA, pp. 229-232.
- Lim ST (2012) Guide catheters and wires. In: Eeckhout E, Serruys PW, Wijns W, Vahanian A, Sambeek M, Palma RD (Eds.), The PCR-EAPC1 Percutaneous Interventional Cardiovascular Medicine Textbook. (1st edn). Europa Edition, Spain, pp. 3-7.
- Bitar S, Kern MJ (2003) Angiographic data. In: Kern MJ (Ed.), The cardiac catheterization handbook. (4th edn). Mosby, Philadelphia, USA, pp. 248250.
- Pacold I, Hwang MH, Piao ZH, Scanion PJ, Loeb HS (1989) The mechanism and significance of ventricularization of intracoronary pressure during coronary anjiography. Am Heart J 118(6): 1160-1166.
- Baim DS (2006) Coronary angioraphy. Grossman's cardiac catheterization, angiography, and intervention. (7th edn), Lippincott Williams & Wilkins, Philadelphia, USA, pp. 190-191.
© 2018 Nuray Kahraman Ay. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






