- Submissions

Full Text
Novel Research in Sciences
Transversus Abdominis Plane Blocks for Pain Management Following a Laparoscopic Bariatric Surgery – Data from a Clinical Trial
Haitov Ben Zikri Zoya1, Kais Hasan2, Dovzhenko Sergii1, Volis Marina1, Alon Hana1, Bar Yehuda Sara1*, Gofman Vladislav1 and Mazor Andrie1
1Anesthesiology Department, Shamir Medical Center, Tel Aviv University, Israel
2Division of Surgery, Shamir Medical Center, Sackler Faculty of Medicine, Tel Aviv University, Israel
*Corresponding author:Sara Bar Yehuda, Anesthesiology Department, Shamir Medical Center, Aviv University, Zerifin, 70300, Israel
Submission: May 24, 2024;Published: June 27, 2024
.jpg)
Volume16 Issue1 June 27, 2024
Abstract
Bariatric surgery has been shown to successfully achieve sustainable weight-loss in Class II obesity or in patients with body mass index >35 kg/m2. Even though that the bariatric surgery is considered to be a minimally invasive procedure and is performed with a laparoscopic approach, moderate to severe pain often occurs during the immediate postoperative period. One of the anesthetics regularly used to relieve pain after surgery are opioids. However, opioids have numerous side effects and carry the risk of long-term abuse. The use of abdominal wall blocks, such Transversus Abdominis Plane (TAP) block or Subcostal TAP block, has been suggested as an effective strategy to reduce postoperative pain after abdominal surgery. The aim of the current study was to compare the efficacy of ultrasound guided TAP block and the Subcostal TAP block on pain intensity and the use of pain relief medications, 2 and 24 hours after bariatric surgery. The data revealed that the peripheral nerve blocks TAP and Subcostal TAP reduced significantley pain intensity and the analgesic consumption during the first 24 hours after bariatric surgery, compared to patients who did not receive a block treatments.
Keywords:Bariatric surgery; Pain management; Transversus abdominis plane block; Subcostal TAP block
Introduction
Obesity is a complex and multifactorial disease which carries with it comorbidities, morbidity, mortality and decreased quality of life [1]. The incidence of obesity has been increasing in the last three decades so much so that it has become an epidemic and a global health problem [2]. Diet and physical activity, as well as lifestyle changes and medical treatments are the most common approaches to fight obesity. However, the results are not satisfactory and do not so much achieve the goal of weight loss. Currently, the most effective treatment option for morbid obesity is bariatric surgery [3].
Bariatric surgery has been shown to successfully achieve sustainable weight-loss in Class II obesity or patients with body mass index >35 kg/m2 [4]. Performing a bariatric surgery in obese patients was found to reduce the risk of 5-year mortality and to result in a long lasting improvement in quality of life [5]. Bariatric surgery is usually performed via a laparoscopic approach, which is considered to be safer and is associated with reduced hospital stay and faster recovery of the patient, than open procedures [7]. The most commonly performed bariatric procedures are the laparoscopic sleeve gastrectomy and the laparoscopic Roux-en-Y gastric bypass [7].
Even though that the bariatric surgery is considered to be a minimally invasive procedure and is performed with a laparoscopic approach, moderate to severe pain often occurs during the immediate postoperative period [8]. The abdominal pain upon bariatric surgery is caused by the abdominal wall which is hurt throughout the insertion of the ports and by the visceral organs upon damaging the gastrointestinal serosa [Coşkun 2019 - 9]. Pain located under the left shoulder also appears. This pain stems from associated CO2 pneumoperitoneum [9,10].
Insufficient control of postoperative pain is associated with delayed recovery, higher rate of complications, longer opioid usage, as well as extension of hospitalization. In addition, functional impairment and lower quality of life could occur [11]. The issue of pain control is much more significant when it comes to treating obese patients. Impaired movement is a common characteristic of obese people. Postoperative pain in obese patients increases the immobilization, there by intensifies the risk of deep vein thrombosis, atelectasis, respiratory depression and pulmonary embolism [12,13]. Thus, controlling the pain in this patients’ population poses a very critical issue. Systemic analgesic, long-acting local analgesic infiltration of trocar site, as well as epidural analgesia are the most common methods used to manage postoperative pain [9].
One of the anesthetics regularly used to relieve pain after surgery are opioids. However, opioids have numerous side effects, including respiratory depression, postoperative ileus, nausea and vomiting. In addition, the opioids carry the risk of long-term abuse [14]. It has been demonstrated that obese patients are at high risk to develop opioids dependence [15]. Not only that, an increased rate of respiratory depression upon treatment with opioids was found among morbid obese patients [16]. Thus, controlling the pain in this patients’ population poses a challenge to the anesthetists.
The use of abdominal wall blocks has been suggested as an effective strategy to reduce postoperative pain after abdominal surgery [17]. The Transversus Abdominis Plane (TAP) block is an afferent block of the anterior abdominal wall that can reduce pain and opioid use following lower abdominal surgery [17,18]. The TAP block is targeting the plane between the obliquus internus and transversus abdominis muscles, exiting the T6 to L1 spinal roots [10,19]. TAP block has been demonstrated to relief pain upon various upper and lower abdominal surgical procedures, including laparoscopic cholecystectomy, open appendectomy and cesarean section [17,19]. The impact of TAP block on immediate postoperative pain after various bariatric surgery, including sleeve gastrectomy and Roux-en-Ygastric bypass, has been investigated in some clinical studies [17,20,21]. Subcostal TAP block, has also been reported to provide analgesia for incisions extending above the umbilicus [22]. This kind of block could extend the analgesic effect up to a larger area of spread, T7-T12 nerve, where the epigastric port of laparoscope is inserted [19,23]. The aim of the current study was to compare the efficacy of an ultrasound guided TAP block and the Subcostal TAP block on pain intensity and the use of pain relief medications 2 and 24 hours after bariatric surgery, compared to patients who did not receive a block treatments.
Methods
Study design
Patients undergoing laparoscopic single anastomosis gastric bypass for morbid obesity were prospectively enrolled to the study and received ultrasound-guided abdominal wall nerve blocks. This study group was randomly assigned into two groups based on type of abdominal wall nerve block: Ultrasound-guided bilateral TAP block, and ultrasound-guided bilateral TAP block + ultrasoundguided bilateral Subcostal TAP block. The study group was compared to historical controls that underwent the same type of surgery during 2018 without any abdominal wall nerve blocks. The study was approved by the institutional review board. All patients signed an informed consent form.
Anesthesia process
The anesthesia was performed by a specialist anesthesiologist with over 10 years’ experience who had over two years’ practice in the administration of the tested peripheral blocks.
In the operating room, the patient was attached to a standard monitor, recording electroencephalogram, non-invasive blood pressure and saturation. Preoxygenation was performed for 4 minutes with 2μg/kg Fentanyl administered intravenously 2 minutes of 2mg/kg Propofol and 0.5mg/kg Rocuronium. The patient was then intubated and connected to an anesthesia machine. The anesthesia was maintained by Izoflurane 1 MAC, muscle relaxants according to monitoring (3-4μg/kg Febtanyl). Additional monitoring of end-tidal carbon dioxide, body temperature, anesthetic gases and breathing parameters was conducted after intubation.
The administration of the ultrasound guided abdominal wall nerve blocks was done after the patient was connected to the anesthesia machine, prior to the surgical incision. The blocks included 0.25% MARCAINE (totally 30ml) and 2mg Dexamethasone. All patients were extubated in the operating room at the end of the surgical procedure and transferred to the post-anesthesia care unit.
Bariatric surgery procedure
The surgery was performed via a laparoscopic approach using four ports of 5 to 10mm. The gastric pouch was made using laparoscopic staplers, and a single anastomosis was made between the gastric pouches in the small intestine 2m distal to the ligament of Treitz.
Monitoring the intensity of pain and the use of painkillers
The intensity of pain and the use of painkillers were monitored in the post-anesthesia care unit (2 hours after surgery) and in the surgical department (24 hours after surgery).
Time. Pain intensity was monitored by the Visual Analogue Scale (VAS) scale.
Painkillers included NSAIDs and opioids. The consumption of the following painkillers was monitored: Paracetamol (1gr.), Tramal (100-200mg.), Morphine (10mg.), IV Dipyrone (1gr.) and Voltaren (75mg.).
Pain records and analgesia regimen data were collected by the professional staff who were blind to the randomization of the study.
Statistical analysis
Analysis was conducted using IBM SPSS Statistics version 29.0. Descriptive statistics were performed mainly with rates and means, parametric and non-parametric tests were performed. Comparing continuous variables (age, pain levels and number of medications between the treatment groups was performed using t-test, one way ANOVA and Kruskal–Wallis H one-way ANOVA with Bonferroni correction, as appropriate. Categorical variables (gender and rates of medication consumption) were analysed using Chi-square test. Boxplot diagrams were used for descriptive demonstration of the distributions. Pearson correlation coefficient was performed to estimate the correlation between age and pain intensity among the 3 treatment groups. Differences considered as statistically significant at Pv of < 0.05.
Result
Study population
The study included 66 patients, 36 of them (54.5%) served as control, 15 (22.7%) were treated with TAP block and 15 (22.7%) were treated with Subcostal TAP + TAP blocks. Most of the patients were females and the average age was similar in all groups (Pv=0.436) (Table 1).
Table 1:Demographic characterizations of the study population.

Pain
Pain intensity was statistically significantly lower between the control group and the TAP block or the TAP +Subcostal TAP blocks groups, both at 2 hours and 24 hours after surgery (Pv<0.001) (Table 2). Nevertheless, Post Hoc Tests revealed that there was no statistically significant difference in the pain intensity between the two treatments arms, the TAP block vs. the TAP +Subcostal TAP blocks (Pv=1.000 2 hours after the surgery and Pv=0.257 24 hours after the surgery).
Table 2:Pain intensity at 2 and 24 hours after surgery.

A 2 tailed Pearson Correlation revealed that there was no correlation between age and pain intensity, 2 and 24 hours after surgery in the control group (r=206, Pv = 0.228 at 2 hours and r=-0.250, Pv = 0.141 at 24 hours after surgery), in the TAP block treatment group (r=-0.394, Pv = 0.146 at 2 hours and r=0.420, Pv = 0.119 at 24 hours after surgery) and in the TAP block + Subcostal TAP block treatment group (r=0.174, Pv = 0.534 at 2 hours and r=- 0.007, Pv = 0.981 at 24 hours after surgery).
A two sided t-test analysis revealed that there was no correlation between gender and pain intensity at 2 and 24 hours after surgery in the control group (Pv = 0.500 and 0.950), in the TAP block treatment group (Pv = 0.423 and 0.977) and in the TAP block + Subcostal TAP block treatment group (Pv = 0.327 and 0.962).
Medications
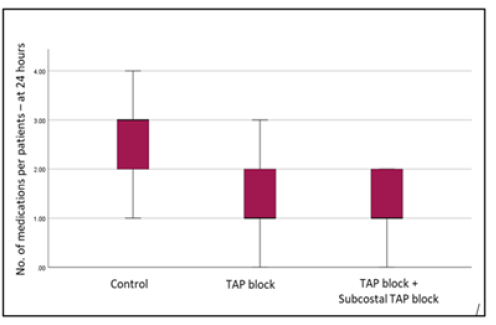
Overall, 2 hours after the surgery 100.0% of the patients in the control group, 100.0% and 86.7% of the patients in the TAP block and in the TAP block + Subcostal TAP block groups requested pain relief medications (Pv=0.030, between the groups). At 24 hours after the surgery, 100.0% of the patients in the control group, 93.3% and 80.3% of the patients in the TAP block and in the TAP block + Subcostal TAP block groups received medications (Pv=0.026, between the groups) (Table 3). Moreover, the number of medications used per patient was lower among the block treated groups compared to the control group, both at 2 hours and 24 hours after the surgery (Mean±SD: 2.72±0.94, 2.13±0.64 and 1.73±1.10 for the control group, TAP and TAP+Subcostal TAP groups, respectivlly, Pv= 0.002 at 2 hours and 2.60±0.60, 1.47±0.83 and 1.20±0.77, for the control group, TAP and TAP+Subcostal TAP groups respectively, Pv <0.001, respectively, control vs. treatments at 24 hours) (Table 3).
Table 3:Percent of patients consuming various painkillers and no. of medications per patients at 2 and 24 hours after the surgery.

Post Hoc Tests revealed that at 2 hours there was a significant difference in the mean number of medications used by the control group vs. the TAP+Subcostal TAP treatment group (Pv=0.003) and 24 hours after surgery there were significant differences in the mean number of medications used by the control group vs. the TAP as well as TAP+Subcostal TAP treatment groups (Pv<0.001 for both comparisons). There was not a statistical difference between the treatments arms (Pv=0.722 at 2 hours after surgery and Pv=0.906 after 24 hours after surgery). These findings are also presented in box-plot comparison in Figure 1a & 1b (Kruskal-Wallis tests)
Figure 1a:Number of medications used per patients at 2 hours after the surgery.
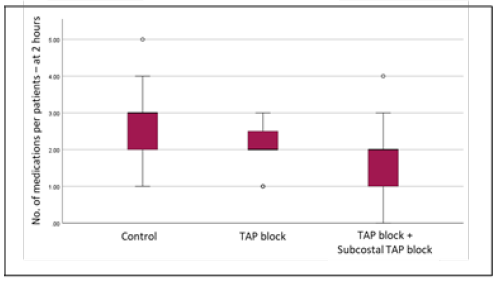
Figure 2a:Number of medications used per patients at 24 hours after the surgery.
Acamol was used by 53.0% of the patients at 2 hours after the surgery. Interestingly, while 38.9% of the patients in the control group got the drug, 80.0% and 60.0% of the patients in TAP block group and in the TAP block + Subcostal TAP block group used this medication, respectively (Pv=0.023, control vs. treatments). Tramal was used by 45.5% of the patients at 2 hours after the surgery. However, while 61.1% of the patients in the control group got the drug, only 33.3% and 20.0% of the patients in TAP block group and in the TAP block + Subcostal TAP block group, respectively used it (Pv=0.015, control vs. treatments).
Optalgin was used by 43.9% of the patients at 2 hours after the surgery. The percent of patients among the block treated group used was significantly lower compared to the control, 33.3% and 20.0% of the patients in TAP block group and in the TAP block + Subcostal TAP block group respectively, and 58.3% in the control group (Pv=0.027, control vs. treatments). Most of the patients in the study were treated with Morphine, 78.8% at 2 hours after surgery. Although less patients treated with the blocks got Morphine compared to the control, the difference was not statistically significant, 66.7% and 73.3% of the patients in TAP block group and in the TAP block + Subcostal TAP block group, respectively and 86.1% in the control group (Pv=0.254, control vs. treatments). Voltaren was used only by 15.2% of the patients. Whereas 27.8% of the patients in the control group used the drug, no patient from the TAP or the TAP block + Subcostal TAP block groups was treated with Voltaren (Pv=0.007) (Table 4).
Table 4:Percent of patients consuming various painkillers at 2 and 24 hours after the surgery.

Interestingly, regarding the consumption of each of the medication, the use of Tramal, Optalgin and Voltaren were significantly higher in the control group compared to the TAP block and the TAP block + Subcostal TAP block groups (Pv = 0.007, 0.012 and 0.023, respectively).
As for the medications used 24 hours after surgery, Acamol was used by 57.6% of the patients. Here also 44.4% of the patients in the control group used the drug, while 80.0% in the TAP block group and 66.7% in the TAP block + Subcostal TAP block group (Pv=0.046, control vs. treatments). Tramal was the most used medicine 24 hours after the surgery, 75.8%. Almost all the patients in the control group used Tramal - 97.2%, Whereas 53.3% and 46.7% of the patients in the TAP and the TAP block + Subcostal TAP block groups required the drug (Pv<0.001, control vs. treatments). Half of the patients received Optalgin 24 hours after the surgery, however 94.4% of the patients from the control group compared to no patients in the TAP and in the TAP block + Subcostal TAP block groups (p<0.001, control vs. treatments) used this drug. Interestingly, while Morphine was the most used medication 2 hours after the surgery almost no patient was treated with the drug 24 hours after the surgery, 78.2% compared to 4.6%.
No patient in the control group got Morphine, while 13.3% and 6.7% were treated with the drug in the TAP and the TAP block + Subcostal TAP block groups, respectively, but the difference was not statistically significant (Pv=0.109, control vs. treatments). Voltaren was used by 13.6% of the patients 24 hours after the surgery, however 25.0% in the control group while no patient in the TAP and the TAP block + Subcostal TAP block groups used Voltren (Pv=0.013, control vs. treatments) (Table 4). A significant higher percent of patients in the control group used Acamol, Tramal, Optalgin and Voltaren compared to the TAP block group (Pv= 0.00, <0.001, 0.001 and 0.033, respectively). When comparing the percent of patients who used each of the medications in the control group vs. the TAP block + Subcostal TAP block it was found that a significant higher percent of patients from the control group used Tramal, Optalgin and Voltaren (Pv<0.001, <0.001 and =0.033, respectively). Nevertheless, as with the pain intensity there was no difference in the percent of patients who used medications between the TAP block treatment group and the TAP block + Subcostal TAP block treatment group at 2 and 24 hours after the surgery.
Discussion
Postoperative pain management is crucial, especially among obese patients who underwent a bariatric surgery. Reduction of postoperative pain is consequently associated with improved patient’s compliance and reduction of early postoperative complications. Hence, in 2016, the Enhanced Recovery After Surgery (ERAS) society guidelines for bariatric surgery declared that a multimodal analgesic approach should be considered the gold standard for pain management after the surgery [9]. In 2019, the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) developed its own ERAS protocol, called Bariatric Surgery Targeting Opioid Prescriptions (BSTOP). These new guidelines were developed in order to improve the postoperative pain management, while decreasing opioid use [24].
In order to achieve the goal of reducing the opioid consumption, TAP blocks have been suggested to be performed in case of analgesia of the abdominal wall above the umbilicus is required. There is data from studies which compared the TAP or the Subcostal TAP block to various commonly used analgesic techniques aimed to reduce postoperative pain following laparoscopic bariatric surgery. The analgesic effect of an ultrasound-guided TAP was compared to erector spine plane block in 60 patients who underwent a laparoscopic bariatric surgery. The mean VAS score during the first 24h after the surgery was higher among the TAP block treated group than in the erector spine plane block. Also, the time to first use of analgesia was longer with the rector spine plane block. Thus, in this study, the erector spine plane block was more effective in reducing the postoperative pain and analgesia consumption than the TAP block [25]. As for the Subcostal TAP block, in a study conducted by Coşkun et al., 45 patients who underwent a laparoscopic sleeve gastrectomy were randomized to be treated with a TAP block or a trocar site infiltration. VAS values measured while resting, coughing, and post-mobilization did not show significant differences. There were no significant differences between the groups in the VAS values and Tramadol use. In this case the authors concluded that the trocar site infiltration is the consistent preferred intervention to control postoperative pain after laparoscopic sleeve gastrectomy [26].
The analgesic effect of the TAP block was compared to the one induced by Subcostal TAP block in patients who underwent laparoscopic cholecystectomy. The data from this study demonstrated that subcostal TAP block treatment resulted with a better postoperative analgesia as compared to the TAP block. Nevertheless, early recovery and discharge from hospital was the same among both treatments [23]. On the contrary, we have lately demonstrated that there was no significant difference in the pain scores when patients who underwent a laparoscopic cholecystectomy were treated with TAP or Subcostal TAP alone, nor when the patients were treated with a combination of Subcostal TAP block with a TAP block. However, the combination of the peripheral nerve blocks reduced the use of analgesic consumption during the 24 hours after laparoscopic cholecystectomy surgery, compared to standalone blocks [19].
To the best of our knowledge, this is the first randomized controlled study comparing the analgesic effect of the TAP block to the TAP block + Subcostal TAP block in patients with obesity undergoing laparoscopic bariatric surgery. The data from the current study demonstrated that the treatment of both, TAP or TAP + Subcostal TAP blocks significantly reduced pain intensity at 2 and 24 hours following the bariatric surgery, compared to the control group. Consequently, significantly less patients who were treated with the blocks requested pain relief medications than in the control group. Not only that, but the number of medications used per patients was significantly lower among patients treated with the blocks in comparison to the patients who were not treated with the blocks. Interestingly, there was no statistically significant difference in the pain scores or medication consumption between the two treatments, TAP vs. TAP + Subcostal TAP blocks. Moreover, it is very important to note that both interventions, the TAP and the TAP block + Subcostal TAP blocks seemed to be safe, since no complications were reported.
Conclusion
The results of the present study indicated that the peripheral nerve blocks TAP and Subcostal TAP reduced pain intensity and the analgesic consumption during the first 24 hours after bariatric surgery, compared to patients who did not receive a block treatments.
In light of those findings we recommend adding the treatment option of peripheral nerve blocks to the ERAS guidelines as part as the multimodal analgesic approach in order to achieve pain relief and to reduce the requirement for analgesics, especially opioids, shortly after bariatric surgery.
Our study also had some limitations. The design of the study was based on comparing a prospective cohorts to a retrospective historical cohort, although both main outcomes, VAS scores and analgesic use, were routinely precisely recorded in both time frames. The sample size is relatively small, but was sufficient to show statistically significant difference the control and the treatments arms.
References
- Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. (2009) Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet 373(9669): 1083-1096.
- Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, et al. (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10): 1822-1832.
- Alamuddin N, Bakizada Z, Wadden TA (2016) Management of obesity. J Clin Oncol 34(35): 4295-4305.
- Phillips BT, Shikora SA (2018) The history of metabolic and bariatric surgery: Development of standards for patient safety and efficacy. Metabolism 79: 97-107.
- Omotosho P, Mor A, Shantavasinkul PC, Corsino L, Torquati A (2016) Gastric bypass significantly improves quality of life in morbidly obese patients with type 2 diabetes. Surg Endosc 30(7): 2857-2864.
- Cantore F, Boni L, Di Giuseppe M, Giavarini L, Rovera F, et al. (2008) Pre-incision local infiltration with levobupivacaine reduces pain and analgesic consumption after laparoscopic cholecystectomy: a new device for day-case procedure. Int J Surg 6(Suppl 1): S89-S92.
- Arterburn DE, Telem DA, Kushner RF, Courcoulas AP (2020) Benefts and risks of bariatric surgery in adults: A Review. JAMA 324(9): 879-887.
- Albrecht E, Kirkham KR, Endersby RV, Chan VWS, Jackson T, et al. (2013) Ultrasound-guided Transversus Abdominis Plane (TAP) block for laparoscopic gastricbypass surgery: A prospective randomized controlled double-blind trial. Obes Surg 23(8): 1309-1334.
- Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, et al. (2016) Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) society recommendations. World J Surg 40(9): 2065-2083.
- Ruiz Tovar J, Garcia A, Ferrigni C, Gonzalez J, Levano LC, et al. (2018) Laparoscopic-Guided Transversus Abdominis Plane (TAP) Block as Part of Multimodal Analgesia in Laparoscopic Roux-en-Y Gastric Bypass Within an Enhanced Recovery After Surgery (ERAS) Program: A Prospective Randomized Clinical Trial. Obes Surg 28(11): 3374-3379.
- Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10: 2287-2298.
- Talab HF, Zabani IA, Abdelrahman HS, Bukhari WL, Mamoun I, et al. (2009) Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg 109(5): 1511-1516.
- Atilla N, Arpag H, Bozkus F, Kahraman H, Cengiz E, et al. (2017) Can we predict the perioperative pulmonary complications before laparoscopic sleeve gastrectomy: Original research. Obes Surg 27(6): 1524-1528.
- Horsley RD, Vogels ED, McField DAP, Parker DM, Medico C, et al. (2019) Multimodal postoperative pain control is effective and reduces opioid use after laparoscopic Roux-en-Y Gastric Bypass. Obes Surg 29(2): 394-400.
- Okifuji A, Hare BD (2015) The association between chronic pain and obesity. J Pain Res 8: 399-408.
- Booth HP, Khan O, Fildes A, Prevost AT, Reddy M, et al. (2016) Changing epidemiology of bariatric surgery in the UK: cohort study using primary care electronic health records. Obes Surg 26(8): 1900-1905.
- Emile SH, Abdel Razik MR, Elbahrawy K, Elshobaky A, Shalaby M, et al. (2019) Impact of ultrasound-guided transversus abdominis plane block on postoperative pain and early outcome after laparoscopic bariatric surgery: A Randomized Double-Blinded Controlled Trial. Obes Surg 29(5): 1534-1541.
- Baeriswyl M, Kirkham KR, Kern C, Albrecht E (2015) The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: A meta-analysis. Anesth Analg 121(6): 1640-1654.
- Haitov Ben Zikri Z, Volis M, Mazur A, Orlova T, Alon H, et al. (2023) The effect of various combinations of peripheral nerve blocks on postoperative pain in laparoscopic cholecystectomy: A Comparative Prospective Study. Int J Clin Pract 2023: 8864012.
- Grape S, Kirkham KR, Albrecht E (2020) The analgesic efficacy of transversus abdominis plane block after bariatric surgery: A systematic review and meta-analysis with trial sequential analysis. Obes Surg 30(10): 4061-4070.
- Földi M, Soós A, Hegyi P, Kiss S, Szakács Z, et al. (2021) Transversus abdominis plane block appears to be effective and safe as a part of multimodal analgesia in bariatric surgery: A Meta-analysis and systematic review of randomized controlled trials. Obes Sur 31(2): 531-543.
- Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, et al. (2011) Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia 66(6): 465-471.
- Khan KK, Khan RI (2018) Analgesic effect of bilateral subcostal tap block after laparoscopic cholecystectomy. J Ayub Med Coll Abbottabad 30(1): 12-15.
- (2021) Join Bariatric Surgery Targeting Opioid Prescriptions (BSTOP) American College of Surgeons.
- Elshazly M, El-Halafawy YM, Mohamed DZ, Wahab KA, Mohamed MK (2022) Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: A randomized comparative trial. Korean J Anesthesiol 75(6): 502-509.
- Coşkun M, Yardimci S, Arslantaş MK, Altun GT, Uprak TK, et al. (2019) subcostal transversus abdominis plane block for laparoscopic sleeve gastrectomy, Is It Worth the Time? Obes Surg 29(10): 3188-3194.
© 2024 Bar Yehuda Sara. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






