- Submissions

Full Text
Novel Practices in Medical Study
Exploring the Effect of Neurological Disorders and Diseases: A Review
Radwa Abdallnasser Amen*
Biotechnology Department, Faculty of Science, Cairo University, Egypt
*Corresponding author:Radwa Abdallnasser Amen, Biotechnology Department, Faculty of Science, Cairo University 424010, Egypt
Submission: July 10, 2024;Published: July 23, 2024

NPMSVolume1 Issue3
Abstract
Neurological disorders include a wide range of ailments that impact both the central and peripheral nervous systems; neurodegenerative disorders, which are characterized by neuron loss, include Alzheimer’s disease and Parkinson’s disease, as well as epilepsy, multiple sclerosis, and stroke. These illnesses cause considerable problems because of their various presentations and complex underlying mechanisms. the neurological mechanisms that underpin illnesses, focusing on neural communication, neurotransmission, neuroplasticity, neurodevelopment, neuroinflammation, neuroendocrinology, and neurovascular coupling. Understanding these pathways is critical for determining illness pathophysiology and designing effective therapies. Understanding paraneoplastic neurological disorders, brain metastases, primary brain tumors, neurological side effects of cancer treatment, and the developing area of neuro-oncology. Recognizing and addressing neurological problems in cancer patients is critical for improving their prognosis and quality of life. Although numerous medications are currently approved to treat neurodegenerative illnesses, the vast majority of them simply address accompanying symptoms. The absence of pathogenesis-targeting therapeutics is primarily owing to the Blood-Brain Barrier (BBB), which keeps nearly 99% of all foreign chemicals out of the brain.
Keywords:Dementia; Alzheimer’s disease; Parkinson’s disease; Disorientation
Introduction
Figure 1:Showing how brain effect in neurological disorder.
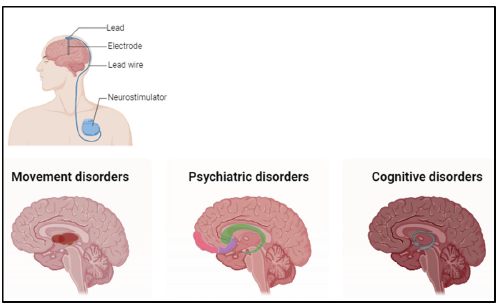
Neurological Disorders (ND) (Figure 1) are diseases affecting the central or peripheral nervous systems. In other words, they impact the brain, spinal cord, cranial nerves, peripheral nerves, nerve roots, vegetative nervous system, neuromuscular junction, and muscles. These disorders include epilepsy, Alzheimer’s disease and other dementias, cerebrovascular diseases such as stroke, migraines, and other headaches, multiple sclerosis, Parkinson’s disease, nervous system infections, brain tumors, traumatic nervous system disorders such as head injuries, and neurological disorders caused by malnutrition. These abnormalities have an impact on human voluntary everyday life movement. In truth, while the attainment of human voluntary movement appears simple, it is actually quite difficult. Because it is a highly sophisticated mechanism that enables various nerve structures to make decisional and/or reflexive choices. This mechanism then defines and controls the movement via nerve impulses sent towards the musculoskeletal system. It is also known that ND is the primary cause of disability and the second leading cause of death in the globe [1-4].
The aetiology of ND is quite diverse due to the intricacy of the neurological system. There are several causes of ND, including lifestyle, infections, genetics, food, and/or environmental effects. Genetic, epigenetic, and external variables, such as physical trauma, infection, and other features of the environment, can all have a role in the onset and progression of ND. Hormonal, immunological, and molecular/cellular pathways all have an impact on the clinical presentation of ND, which involves various systems [5]. Furthermore, gut dysbiosis (microbiota dysregulation) has been linked to several neurodegenerative disorders [6]. ND may have a deleterious impact on bone physiology, reducing bone mineral density and content, altering bone microarchitecture, and decreasing bone strength, all of which contribute to the development of osteopenia/osteoporosis and increasing the risk of fracture [5]. Neurodegeneration is evident in various ND. This disorder arises when the nervous system or neuron loses structure, function, or both, resulting in gradual degeneration or neuron death, as well as well-defined tissue system linkages, which cause clinical manifestations. According to studies, neuroinflammation precedes neurodegeneration in many ND. In this regard, matrix metalloproteinases appear to play a critical role in the evolution of ND linked to neurodegeneration, however the aetiology and probable causes are broadly indefinable [7].
Symptoms differ according to the type of ND and the affected area. Symptoms may include: i) entire or partial paralysis, ii) muscle weakness, iii) partial or complete loss of sensation, iv) convulsions, v) headache, vi) pain without apparent reason, vii) reduced coordination, and viii) a diminished degree of consciousness [8]. They can be investigated individually or together. Because the nervous system is intricately related to behavior, several neurological disorders result in emotional or behavioral disturbances. In this context, the symptoms can include sudden changes in mood or unexpected outbursts of anger, melancholy, decreased memory, hallucinations, sleep difficulties and mental confusion [9]. The evaluation in ND can discover indicators that signal nervous system changes and recommend the most relevant supplemental examinations to confirm an accurate diagnosis. Among the complementary exams are: i) Magnetic Resonance Imaging, Computed Tomography, positron emission tomography, Ultrasonography, and Doppler; ii) physiological studies such as neurophysiological examinations electroencephalogram, electroneuromyography, and evoked potentials; iii) neuropsychological tests that involve interviews, questionnaire applications, and specific tests, with the aim of testing areas such as attention, memory, language, reasoning, and learning. vi) Biopsies of nerve tissue, skin, or muscles. Rapid and precise diagnosis of ND allows for early treatment, increasing the quality of life and prognosis of the condition, and is frequently the difference between life and death [10].
ND are complex and can impair multiple aspects of functionality; if left untreated, they can have catastrophic implications. The evolution and results are determined by the severity of the condition, the type of disease, the interval between symptom start and therapy, and other factors. Thus, the therapy of ND may include medication, surgery, interdisciplinary interventions, and other sorts of available treatments to aid in the improvement of these people. Physical therapy and other treatments include: i) movement, exercise, and physical activity therapies to increase the individual’s motor capacity. ii) speech therapy, which improves swallowing and language function; iii) occupational/ cognitive therapies, which stimulate functionality by focusing on affected cognitive areas such as memory, verbal and written communication, language, and so on; and iv) psychotherapy, which treats the disease’s emotional components. Selective serotonin reuptake inhibitors, antipsychotics, and anti-epilepsy medicines play distinct and overlapping functions in mediating bone loss [5,11]. Individuals with ND’s functional ability and quality of life can be affected in a variety of ways depending on the injured area, the extent of the injury, the duration of the injury, and the patient’s age. The symptoms linked with each ND vary and can be connected to deficits in movements, cognition, behavior, balance, tone, bone, and spasticity, among others [12,13].
Therapeutic treatments are established according on the kind and progression of ND. These techniques can include pharmaceutical and non-pharmacological interventions, neurological physical therapy, biochemical and molecular approaches, among others that attempt to control the ND, enhancing functionality, everyday activities, and quality of life for these patients [14,15]. This review attempts to provide an overview of the current understanding of neurological disorders and diseases, including clinical characteristics, underlying mechanisms, diagnostic techniques, and treatment strategies. By synthesizing current advances in neurology research, an investigation of neural communication, neurotransmission, neuroplasticity, neurodevelopment, neuroinflammation, neuroendocrinology, and neurovascular coupling, Furthermore, this review will look at the relationship between neurology and other medical disciplines, particularly oncology, focusing on the neurological consequences of cancer and the nervous system’s role in tumor growth and progression. Understanding these interrelationships is critical for designing comprehensive patient care strategies and improving treatment outcomes.
Neurological Disorder
Neurological diseases are a broad category of conditions that affect both the central and peripheral nervous systems, including the brain, spinal cord, and peripheral nerves. Here are a few significant neurological disorders. Alzheimer’s disease is a progressive neurological ailment marked by memory loss, cognitive impairment, and behavioral abnormalities. Alzheimer’s disease is the leading cause of dementia, impacting millions of individuals worldwide. It is the most common form of dementia (60-80% of cases), with clinical symptoms including progressive anterograde episodic memory impairment that affects memory, reasoning, and behavior. The majority of patients with Alzheimer’s are over the age of 65 [16]. Early-onset Alzheimer’s affects those under the age of 65. It is the sixth biggest cause of mortality in the United States, and its global prevalence is estimated at 24 million. The early indication is trouble recalling recently acquired information. Disorientation, mood and behavior changes, confusion about events, time and place, unjustified suspicions about family, friends, and professional cares, and difficulties speaking, swallowing, and walking are all symptoms that can worsen and interfere with daily activities [17].
Parkinson’s disease is a chronic and progressive movement illness caused by the loss of dopamine-producing neurons in the brain. Common symptoms include tremors, bradykinesia (slow movement), rigidity, and postural instability. It is a neurodegenerative illness affecting dopamine-producing neurons in the substantia nigra. It is the world’s second most common neurodegenerative illness, causing a major physical, mental, social, and financial burden on sufferers and cares. The incidence of it increases with age, however only 4% of persons are diagnosed before the age of 50. Parkinson’s disease is believed to affect over ten million individuals globally. [18] The cardinal features are resting tremor, cogwheel rigidity, bradykinesia, and postural instability, which are frequently preceded by prodromal symptoms such as autonomic dysfunction that occur 5 to 20 years earlier. Symptoms typically appear gradually over time and vary from person to person due to the disease’s variability [19]. Multiple Sclerosis (MS) is an autoimmune illness in which the immune system assaults the myelin sheath that protects nerve fibers in the central nervous system. This causes demyelination, inflammation, and nerve fiber destruction, resulting in a variety of symptoms including fatigue, muscular weakness, numbness, and decreased coordination. It is regarded as the most common chronic inflammatory illness of the central nervous system, associated with inflammatory demyelination and astroglial activation, with neuronal and axonal destruction being the primary causes of impairment [20].
In general, those between the ages of 20 and 40 are more susceptible, and late-onset multiple sclerosis is defined by symptoms that start more than 50 years later. Globally, there are about 2,500,000 people who suffer from multiple sclerosis. Each person experiences distinct symptoms based on where in the body the neurological lesion occurred. The most frequent ones include exhaustion, blurred vision, inability to control bladder, and loss of equilibrium. Demyelinating lesions in the brain and spinal cord have a detrimental effect on daily activities, social interactions, and cognition, contributing to the progression of disability. [21] The neurological condition known as epilepsy is typified by recurring seizures, which are abrupt, uncontrollable electrical disruptions in the brain. The intensity and presentation of epileptic seizures can vary greatly, from brief periods of unconsciousness to convulsions or periods of intense gazing. A neurological condition called epilepsy can result in seizures or strange feelings and behaviors. It is a longterm, noncommunicable brain illness that can strike anyone at any age. Epilepsy affects over 50 million individuals worldwide, making it one of the most prevalent neurological conditions. Individual differences in epilepsy symptoms are largely dependent on the kind of seizure. They can include brief periods of disorientation, periods of intense gazing, jerky or twitchy arm and leg movements, loss of consciousness or awareness, and psychological symptoms including anxiety and panic. Genetic alterations that run-in families, head trauma or injury, neurological illnesses, infectious brain diseases like meningitis, birth trauma or injury, and brain developmental abnormalities like autism are among the factors that can lead to epilepsy.
A physical examination and further tests to verify the brain’s proper functioning are part of the diagnosis [22]. These can include a neuropsychological assessment, Electroencephalogram (EEG), Functional Magnetic Resonance Imaging (fMRI), Positron Emission Tomography (PET), Single Photon Emission Computed Tomography (SPECT), Complete Blood Count (CBC), neurological examination, CT scan, and Magnetoencephalography (MEG). Medication is the mainstay of treatment for epilepsy. When medication fails, other approaches, such as surgery, are advised. Drugs like lamotrigine, valproate, and carbamazepine are used to lessen the frequency and severity of seizures. A chest implant is sometimes used to stimulate the vagus nerve and lessen seizures. Additionally, it has been found that children on a ketogenic diet experience less seizures. If epilepsy is not treated, long-term consequences include status epilepticus, falls that result in harm or death, drowning while swimming, heightened risk of car accidents, complications during pregnancy, psychological problems such as depression and suicide thoughts, and the uncommon but potentially deadly sudden unexpected death in epilepsy [23]. Lou Gehrig’s disease, often known as Amyotrophic Lateral Sclerosis (ALS), is a progressive neurological illness that damages motor neurons in the brain and spinal cord. Within a few years of the commencement of symptoms, it usually results in respiratory failure, muscular weakness, and paralysis.
It is described as a progressive neurodegenerative illness that damages brain and spinal cord nerve cells, impairing the ability to control voluntary muscle action and making activities like chewing, walking, and talking difficult. Since this illness progresses, the symptoms worsen with time [24]. In the United States, the prevalence is estimated to be 5 per 100,000, meaning that 30,000 people have this illness. Fasciculations (muscle twitches) in the arm, leg, shoulder, or tongue, cramping in the muscles, spasticity (tight and stiff muscles), weakness in the muscles influencing the arm, leg, neck, or diaphragm, nasal and slurred speech, and trouble eating or swallowing are among the usual symptoms [25]. A stroke is a type of cerebrovascular event in which there is a reduction or interruption of blood flow to a specific area of the brain, resulting in brain damage. Strokes can be either hemorrhagic (resulting from brain hemorrhage) or ischemic (resulting from a blockage in a blood vessel), and they frequently induce abrupt neurological deficits such paralysis, difficulty speaking, or sensory abnormalities. There are three different types of strokes: hemorrhagic stroke which can be either an intracerebral or subarachnoid hemorrhage, ischemic stroke which occurs when blood flow through an artery to the brain becomes blocked, such as blood clots); and transient ischemic attack which occurs when blood flow to the brain is blocked for only a brief period of time [26].
Eighty-seven percent of strokes are ischemic strokes. Every year, around 795,000 people suffer from a stroke. This condition can cause sudden numbness or weakness in one or both eyes; sudden confusion; sudden difficulty speaking or understanding speech; sudden difficulty walking; sudden dizziness; sudden loss of balance or coordination; and sudden severe headache without apparent cause are just a few of the symptoms. A stroke is a medical illness in which inadequate blood flow to the brain results in cell death. It is sometimes referred to as a Cerebrovascular Accident (CVA) or brain assault. This is a major medical emergency that has to be treated right away. Paralysis or numbness in the arm, face, or leg, particularly on one side of the body, difficulty speaking or understanding others, slurred speech, confusion, disorientation, or lack of responsiveness, abrupt behavioral changes, vision issues, difficulty walking, loss of balance or coordination, dizziness, headaches that are severe and abrupt, seizures, nausea, or vomiting are some of the symptoms that can indicate a stroke [27]. Physical examination, blood tests, CT scan, ultrasound, MRI, cerebral angiography, and echocardiogram are all used in the diagnosis of stroke.
The type of stroke will determine the available treatment options. Surgery is advised for hemorrhagic stroke, while medicine or both may be advised for ischemic stroke or transient ischemic attack. Diet and healthy eating, cutting back on cholesterol and saturated fat, managing diabetes, keeping an eye on blood pressure, abstaining from illegal substances, exercising, giving up alcohol and smoking, and controlling blood pressure are all important stroke prevention strategies. Among them are Prodrome symptoms which include constipation, mood fluctuations, food cravings, increased thirst and urination, and frequent yawning that point to an impending migraine. Aura: Nervous system symptoms that appear before or during a migraine, including altered vision, visual abnormalities, altered hearing, and trouble speaking. discomfort on one or both sides of the head, discomfort radiating to the jaw, throbbing or pulsating pain, sensitivity to light, sound, smell, and touch, eye pain, nausea and/or vomiting, blurred vision, lightheadedness, and/or fainting are all considered symptoms of a migraine episode. Post-drome: The period following a migraine attack, characterized by light and sound sensitivity, dizziness, mood fluctuations, weakness, exhaustion and momentary blindness. A migraine’s agony can be quite incapacitating [28].
A migraine might linger for several hours or up to three days. The symptoms of a migraine vary depending on its stage. Among them are Prodrome: Symptoms include constipation, mood fluctuations, food cravings, increased thirst and urination, and frequent yawning that point to an impending migraine. Aura: Nervous system symptoms that appear before or during a migraine, including altered vision, visual abnormalities, altered hearing, and trouble speaking. discomfort on one or both sides of the head, discomfort radiating to the jaw, throbbing or pulsating pain, sensitivity to light, sound, smell, and touch, eye pain, nausea and/or vomiting, blurred vision, lightheadedness, and/or fainting are all considered symptoms of a migraine episode. The period following a migraine attack, characterized by light and sound sensitivity, dizziness, mood fluctuations, weakness, and exhaustion. There isn’t one particular explanation for migraines; instead, a combination of genetics and environmental factors may be involved [29]. Family history, aging, emotional anxiety, environmental factors like weather or altitude changes, abnormal brain structures, imbalances in brain chemicals like serotonin, hormonal changes in women, certain foods or food additives that can act as triggers, alcohol consumption, stress, irregular sleep patterns, and medications like birth control pills are just a few of the many risk factors that have been identified. Evaluation of symptoms and imaging studies to look for any abnormalities in the brain are part of the diagnosis process for migraines.
These consist of a physical examination, blood work, CT scans, MRIs, and analyses of Cerebral Spinal Fluid (CSF). Migraine treatment alternatives assist in managing symptoms and averting episodes. Ibuprofen, Acetaminophen, Sumatriptan, Naratriptan, Ergotamine, Dihydroergotamine, Lisinopril, Propranolol, Metoprolol tartrate, Venlafaxine, Ethosuximide, Naloxone, Carbamazepine, Divalproex, Ethosuximide, and Chlorpromazine are among the medications used to treat migraines. Transcutaneous Supraorbital Nerve Stimulation (t-SNS) and Learning To Cope (LTC) are two methods of treating migraines. A migraine can be prevented by abstaining from migraine-causing foods and activities, exercising frequently, maintaining a healthy weight, and drinking plenty of water. [30] An inherited neurodegenerative disease called Huntington’s disease is marked by gradual motor dysfunction, cognitive impairment, and psychiatric symptoms. It is brought on by a mutation in the HTT gene, which causes aberrant protein aggregates to build up in the brain. A neurodegenerative condition that is largely hereditary is Huntington’s disease. It causes the brain’s nerve cells to gradually deteriorate, which has an impact on emotions, movement, and cognitive abilities. Huntington’s disease symptoms fall into three categories: mental disorders, motor disorders, and cognitive disorders. Movement disorders include tremors, delayed or irregular eye movements, stiffness or contracture of muscles, decreased walking, posture, and balance, difficulties speaking or swallowing, and chorea (involuntary jerking or writhing movements). Cognitive disorders include issues with planning, setting priorities, maintaining attention on tasks, becoming stuck on ideas, actions, or behaviors, losing control of urges, not realizing one’s own actions, processing thoughts slowly, having trouble picking up new information, having trouble speaking, and dysgraphia.
Mental health conditions include mania and/or depression, agitation, social disengagement, sleeplessness, exhaustion, suicidal ideation or impulses, and apathy. Causes a hereditary gene flaw passed down from parents causes Huntington’s disease [31]. However, a novel mutation may be the cause of up to 10% of instances. The first step in diagnosing Huntington’s disease is a physical examination and review of medical history. Brain imaging, genetic testing, and neurological and psychiatric evaluation are further diagnostic techniques. Huntington’s disease cannot be cured, however there are therapies, drugs, and lifestyle modifications that can help the patient manage the illness. Tetrabenazine, Amantadine (monoamine depletory: drugs to treat writhing and involuntary movements), Fluoxetine, Sertraline (antidepressants: drugs to treat depression), Olanzapine, Quetiapine, Risperidone, and Olanzapine (antipsychotic drugs: drugs to reduce symptoms of mood disorders and psychosis), Valproate, and Carbamazepine (mood stabilizers: drugs to manage bipolar disorder symptoms). Huntington’s disease prevention involves family planning after speaking with a genetic counsellor, genetic testing, and contemplating in vitro fertilization using donor eggs or sperm. If in vitro fertilization is chosen, genetic testing of the embryos before implantation is recommended [32].
Peripheral neuropathy is a problem of the peripheral nerves that can be brought on by a number of factors, such as toxins, autoimmune illnesses, diabetes, and infections. Symptoms of peripheral neuropathy may include tingling, discomfort, weakness, and numbness in the extremities. The disorder known as peripheral neuropathy affects the nerves that are not part of your brain or spinal cord. This can result in a range of symptoms and have multiple underlying causes. The type of nerve injured and whether it affects one, multiple, or all of the body’s nerves determine the symptoms of peripheral neuropathy. The following are the most typical symptoms: tingling in the hands or feet, discomfort from stabbing, numbness in the hands or feet, A weak, heavy sensation in the arms and legs, frequent dropping of objects from your hands, a buzzing or startling sensation, a drop-in blood pressure, constipation, problems digesting food, diarrhea, excessive perspiration, and sexual dysfunction, particularly in men [33]. Peripheral neuropathy has a variety of causes. Frequently, no clear reason is identified. It is most commonly caused by diabetes.
Long-term exposure to high blood sugar levels can harm nerves. Excessive alcohol consumption, some medications (such as chemotherapy and HIV treatment), iron or folate vitamin deficiencies, poisons (such as pesticides and solvents), certain cancers such as multiple myeloma and lymphoma, and chronic liver disease are additional risk factors. Peripheral neuropathy is diagnosed through physical examination and a few diagnostic procedures. These consist of tests for blood sugar, Thyroid Function Tests (TFTs), vitamin B12, complete metabolic panel, nerve conduction test, X-ray, CT scan, MRI, study of Cerebrospinal Fluid (CSF), Electromyography (EMG), nerve biopsy, skin biopsy, and heavy metal panel. Certain underlying causes of peripheral neuropathy may respond better to treatment alternatives [34]. Controlling diabetes should be the top priority if it is the cause of the ailment. Pregabalin, Gabapentin, Nortriptyline, Venlafaxine, and Ibuprofen are among the medications used to treat peripheral neuropathy. Plasmapheresis and Transcutaneous Electrical Nerve Stimulation (TENS) are two treatments for peripheral neuropathy. In the event of diabetic neuropathy, prevention of peripheral neuropathy entails managing blood sugar levels, engaging in regular exercise, giving up smoking, consuming less alcohol, and preserving a healthy body weight and blood pressure. Long-term untreated peripheral neuropathy can result in consequences such diabetic foot ulcers, gangrene, cardiovascular automatic neuropathy, burns, and wounds that become numb or lack sensation [35].
Damage to the brain brought on by an external force, such as a blow to the head or a penetrating injury, is known as Traumatic Brain Injury (TBI). TBIs can range in severity from minor concussions to severe brain trauma and cause emotional instability, motor deficiencies, and cognitive impairments. It is defined as an external mechanical force causing injury to the brain that results in either transient or permanent secondary effects. This modification may lead to altered consciousness and impairment of physical, cognitive, and psycho-social functions. In this disease, an increase in oxidative responses triggered by free radicals produced by the injury is the primary mechanism causing neuronal damage. It is thought to be the primary cause of death, illness, and disability globally. In the United States, an estimated 5.3 million people (2 percent of the population) have a handicap as a result of their injury [36]. The indications and manifestations of mild traumatic brain injuries include the following: bodily symptoms, such as headache, nausea or vomiting, exhaustion or drowsiness, difficulty speaking, dizziness or loss of balance, auditory symptoms, such as fuzzy vision, ringing in the ears, an unpleasant taste in the mouth, or alterations in the sense of smell; sensitivity to light or sound; symptoms related to cognition, behavior, or mental health; brief to prolonged loss of consciousness; confusion, disorientation, or dazed state in the absence of loss of consciousness; difficulties concentrating or remembering things; mood swings or changes in mood; feeling depressed or anxious; trouble falling asleep; sleeping more than usual [37].
Taking into consideration the possibility of mild to severe traumatic brain injuries: physical symptoms, unconsciousness ranging from minutes to hours, headaches that don’t go away or get worse, frequent vomiting, nausea; convulsions or seizures, dilated pupils in one or both eyes, clear fluids dripping from the nose or ears, difficulty waking up from sleep, numbness or weakness in the fingers and toes, loss of coordination, profound confusion in cognitive or mental symptoms, agitation, slurred speech, coma, and other consciousness disorders [38]. Brain lesions that occur before, during, or soon after birth can cause irreversible brain damage that results in cerebral palsy, a complex movement condition at the level of the central nervous system. Among children, it is the most prevalent physical impairment. Individual differences exist in the ways it affects them, potentially impairing reflex, balance, posture, muscular tone, control, coordination, and movement of the body. Though certain symptoms of cerebral palsy can get better or worse over time, the condition is permanent. It affects around 18 million people globally, with an incidence of 1 in 700 live births. Along with a reduction in typical motor patterns, it is common to see a reduction in the motor repertoire of gestures and a loss in movement quality. It is a collection of conditions affecting posture, balance, muscle tone, and mobility. It is brought on by an anomaly or disturbance in brain development, frequently as a result of genetic abnormalities, infections contracted during pregnancy, or head trauma sustained in infancy [39].
Cerebral palsy symptoms can vary considerably from person to person and typically manifest in infancy or preschool. Among them include involuntary movements, impaired muscle coordination, and disproportionate or unusual reflexes, sluggish and thrashing motions, decreased joint movability, Spastic paralysis, abnormal posture, unsteady walking, abnormal touch and pain sensations, abnormal hearing and vision, abnormal drooling, difficulty speaking, abnormal posture, abnormal swallowing, abnormal touch and pain sensations, intellectual disabilities, mental disorders, and urinary incontinence are some of the conditions that can cause spasticity. The child’s development is the basis for the cerebral palsy diagnosis. To rule out other potential explanations, medical imaging and blood tests may be utilized [40]. A laboratory examination, an Electroencephalogram (EEG), cranial ultrasonography, and Magnetic Resonance Imaging (MRI) may be performed. Medication, physical and occupational therapy, psychiatric counselling, and operations to enhance quality of life are among the treatment options available for cerebral palsy. Drugs including Baclofen, Diazepam, Dantrolene, and Onabotulinumtoxin A (Botox injections) are utilized. Dorsal rhizotomy and orthopedic surgery are two possible procedures. Physical therapy, occupational therapy, speech and language therapy, and recreational therapy are a few examples of therapies.
Vaccinating against rubella or other infectious diseases prior to becoming pregnant, seeing a doctor frequently while pregnant, and guarding against brain trauma for the unborn child are all ways to avoid cerebral palsy. Brain palsy complications can include muscle shortening or contracture, epilepsy or seizures, blindness, deafness, malnourishment from trouble eating or swallowing, social isolation and depression, lung disease and breathing difficulties, early onset of osteoarthritis, and osteopenia or fractures from low bone density [41].
A neurodevelopmental illness known as Autism Spectrum Disorder (ASD) is typified by limited interests, repetitive behaviors, and difficulties in social communication. This neurobiological condition is impacted by environmental and genetic variables that have an impact on the growing brain. It is estimated that 1 in 59 children, or roughly 1.68% of American children aged 8 years, have an ASD diagnosis. This statistic can be expanded to include children globally. When it comes to behavior, these people may exhibit aggression, self-mutilation, crying, a lack of eye contact, shouting, hyperactivity, impulsivity, inappropriate social interaction, irritability, repetitive movements, meaningless word repetition, or persistent word or action repetition; when it comes to cognitive functioning, they may exhibit learning disabilities or delays in speech; when it comes to psychological symptoms, they may exhibit depression or a tendency to ignore other people’s emotions; when it comes to speech, they may exhibit speech disorders or loss of speech. These people may also exhibit tics, anxiousness, tiptoeing, a lack of empathy, or sensitivity to sound. It also often called autism spectrum condition (ASC), characterizing by confined and repetitive patterns of behavior as well as deficiencies in social communication [42].
It is classified as a spectrum disorder as each person experiences it in a unique way. ASD symptoms include issues with verbal and nonverbal communication, social interaction, repetitive behavior, and narrow interests. Additional typical indicators are hyper- or hyperreactivity to sensory input, persevering interests, verbal and nonverbal communication issues, stereotypical body motions (stimming), difficulty with social contact, and routine preferences. ASD has a complex aetiology with numerous unknown variables. Family history, specific genetic disorders, having elderly parents, taking certain prescription medications, and prenatal and neonatal health concerns are risk factors. Clinical observation of behavior and development, along with extensive diagnostic testing carried out by a team of certified experts comprising psychiatrists, clinical psychologists, neuropsychologists, pediatricians, and speechlanguage pathologists, are the foundations for the diagnosis of ASD. The utilization of a patient’s verbal and written history of autism symptoms becomes more significant for adults. Applied behavior analysis, cognitive behavioral therapy, occupational therapy, psychotropic medication, and speech-language pathology are all involved in the management of ASD. Maximizing a person’s quality of life and functional independence is the aim of management [43].
A mistake in the transmission of nerve impulses to muscles characterizes Myastenia Graves, an autoimmune illness of neuromuscular transmission that causes disabling fatigability and variable weakness. Two times as many women as males are predicted to be impacted by the prevalence, which is roughly 20 cases per 100,000 people. However, when taking older people into account, it appears that men are afflicted more frequently. Muscle weakness is the primary symptom, which gets worse during active periods and gets better after rest times. In general, although not always, compromised are muscles that govern the movement of the eyes and eyelids, facial expression, chewing, talking, and swallowing. Ocular myasthenia, ptosis, diplopia, dysarthria, and weakness in the arms, hands, fingers, legs, and neck are among the symptoms that may manifest. Respiratory failure may result from myasthenia gravis’s extreme weakness. Skeletal muscle weakness is a result of neuromuscular disease called myasthenia gravis. Symptoms: Rather than a generalized weakness, the first signs are usually specific muscular weakness and fatigability [44].
With exercise and as the day goes on, weakness gets worse. Usually, it affects the muscles in the eyes first, followed by the muscles in the face and limbs. Eye issues include drooping and double vision, as well as difficulties speaking, swallowing (which makes choking easy), and chewing, can all be symptoms. Reasons: As an autoimmune condition, myasthenia gravis results from your body being wrongly attacked by your immune system. It can occasionally be linked to an anomalous thymus gland tumor or enlargement. Congenital cases, or those that exist from birth, are rare. Complications: When breathing muscles are impacted, it can cause a Myasthenic crisis, which is potentially fatal if left untreated for an extended length of time. Myasthenia Gravis patients are more likely to develop thymus cancer. Numerous issues might arise from variations in the synthesis of hormones. Diagnosis: A physical examination and testing to look for neurological issues are part of the diagnosis process [45]. Treatment: Although there isn’t a known cure for myasthenia gravis, drugs can help control and lessen symptoms. Among the medications are pyridostigmine (a cholinesterase inhibitor) and immunosuppressants such as prednisolone, triamcinolone, and methylprednisolone. To treat the symptoms, an oversized thymus may occasionally be removed. Prevention: Although there is no known way to stop the illness from getting worse, patients can lessen their chances of aggravating it by avoiding triggers such mental stress, exposure to high temperatures, fever, infections, certain drugs, and overexertion [46].
Accidents or violent incidents frequently result in spinal cord injuries. Serious clinical-neurological impairments resulting in long-lasting physical and psychological consequences are often linked to this illness. A violent attack (such as a stabbing or gunshot), plunging too shallow into the water and hitting the bottom, head or spinal injuries sustained in a car accident (such as injuries to the face, neck, or back), falling from a considerable height, electrical accidents, and car crashes can all result in it. An estimated 327 million individuals are impacted by this illness each year. A headache, pain, pressure, and stiffness in the back or neck region, signs of shock, difficulty walking, loss of control over the bladder or bowels, immobility of the arms and legs, spreading numbness or tingling in the extremities, and abnormal head positioning are some of the possible symptoms. A Spinal Cord Injury (SCI) is a grave ailment that can profoundly affect an individual’s life. Here are some essential details regarding this condition: Signs: The location and extent of the injury determine the symptoms of a spinal cord injury [47].
Walking difficulties, weakness, loss of control over one’s bladder or bowels, sensations of spreading numbness or tingling in the extremities, unconsciousness, headaches, breathing difficulties, coughing, and back pain are typical symptoms. Causes: Spinal cord damage from car accidents, sports injuries, violent incidents like shootings or stabbings, vascular diseases, tumors, infectious diseases, developmental disorders, spondylosis, and osteoporosisrelated vertebral fractures are among the most common causes. Complications: Complete permanent paralysis and shock could result from this if left untreated for an extended length of time. Diagnosis: The diagnosis entails a physical assessment and scrutiny of the motions and functions of the senses. Bony irregularities in the vertebrae, tumors, suspected spinal cord lesions, ligamentous injuries, herniated discs, blood clots, or other masses that may be compressing the spinal cord are all detectable with medical imaging techniques like CT scan, X-ray, and MRI. Treatment: Medication is used to reduce symptoms, and surgery is performed to realign the spine. Medications include Methylprednisolone (Steroid therapy: To decrease the adverse effects of SCI), Codeine, Hydrocodone, Oxycodone, Methadone (Analgesics: To relieve pain). Spinal traction is used to maintain the spine immobilized, and spinal surgery is used to stabilize the spine. Treatment plans frequently include rehabilitation, which includes physical and occupational therapy, pain management techniques, and the use of assistive equipment including leg braces, wheelchairs, and walkers. Avoidance: Using a seatbelt while driving, donning the appropriate protective gear when participating in sports, staying out of small swimming pools, and avoiding heavy lifts are some preventative measures [48].
The Effect of Viruses on Neurodegenerative Diseases
Viral infections can induce pathological indications through immunological responses or create neurological symptoms. One or more of these disorders have been linked to viruses from the families Herpesviridae, Orthomyxoviridae, Flaviviridae, and Retroviridae. It is true that neurological problems can be significantly impacted by viral infections. Relationship Between Viral infections and Neurodegenerative Diseases. Previous studies have discovered connections between the chance of developing Alzheimer’s disease and other neurodegenerative diseases and specific viral infections. The findings imply that avoiding viral infections such as the flu may help prevent some neurodegenerative illnesses. forty-five correlations between viruses and neurodegenerative disorders were discovered [49]. Twenty-two of these were also found in another investigation. The strongest correlation was found between Alzheimer’s Disease (AD) and viral encephalitis, or virally-induced brain inflammation.
The likelihood of diagnosing AD in a person with viral encephalitis was 30 times higher than in a person without encephalitis. The pathophysiology of COVID-19-related neurological complications: Given the high number of infected patients, neurological sequelae from SARS-CoV-2 infection are rather uncommon, but they have the potential to cause severe long-term morbidity and mortality [50]. Many common neurological illnesses, such as encephalopathy, encephalitis, acute demyelinating encephalomyelitis, stroke, and Guillain-Barré syndrome, are now differentially diagnosed with COVID-19. Viral Infections and Molecular Mimicry where a variety of viral infections, such as HIV, Epstein-Barr virus, and herpes simplex virus, have been linked to delayed induction of post-viral autoantibodies or molecular mimicry between viral proteins and neuronal antigens. Risk of Neurodegenerative illness as 45 viral exposures were shown to be substantially linked to an elevated risk of neurodegenerative illness.
Twente-two relationships were replicated in the analysis, including the link between multiple sclerosis and the Epstein-Barr virus. Up to 15 years following infection, some of these exposures were linked to a higher risk of neurodegeneration. It is true that viral exposure raises the risk of neurodegenerative illnesses. Using longitudinal data, a previous study found that 45 viral exposures were substantially linked to an elevated probability of post-exposure neurodegenerative illness onset following multiple test correction during the discovery phase. The cross-sectional data from the UK Biobank confirmed 22 of these correlations [51]. Epstein-Barr Virus and Multiple Sclerosis where previous study also confirmed the link between Epstein-Barr virus exposure and multiple sclerosis 5-15 years before to diagnosis. Viral exposures raise the risk of neurodegenerative illness later in life, with the elevated risk remaining considerable up to 15 years after some episodes. Viral infections and Neurodegeneration: Certain viral infections may contribute to neurodegeneration. Researchers discovered that some viral compounds encouraged the intercellular spread of protein clumps, which are characteristic of brain illnesses such as Alzheimer’s. These findings could help explain how acute or chronic viral infections can contribute to neurodegeneration. Common Viruses and Long-term Risk of Neurodegenerative Diseases. Viral exposure may raise the risk of future Neurodegenerative Disorders (NDDs) in older persons [52].
Neurology and Cancer
Paraneoplastic Neurological Syndromes (PNS) Some malignancies can create antibodies or immune system components that react with normal nervous system proteins, causing neurological dysfunction. These are referred to as paraneoplastic neurological syndromes. Examples are paraneoplastic cerebellar degeneration, Lambert-Eaton Myasthenic Syndrome (LEMS), and limbic encephalitis. Early diagnosis and treatment of these illnesses is critical for better outcomes. It is a set of disorders that affect persons who have cancer, usually systemic malignancies. They are the outcome of an immune response to a distant malignancy. Symptoms include fever, nocturnal sweats, weight loss, and decreased appetite. PNS can influence a variety of organ systems, including the neurological and endocrine hormone systems. Polyneuropathy, cerebellar degeneration, encephalitis, uncontrollable eye movements, rapid contractions of the arms and legs, and chorea are all examples of neurologic syndromes or symptoms. Causes: The primary tumor and its metastases do not cause PNS. The symptoms are induced by tumor-generated chemicals such as hormones and cytokines or antibodies created by the immune system to attack cancer cells. Complications: The risks include morbidity, muscle loss, memory loss, and cognitive impairment. To diagnose the disorder, a physical examination as well as blood testing are required. Further tests, including as imaging and electrophysiology, are requested based on the symptoms and results. Antibody tests are performed to detect paraneoplastic antibodies in the blood. Treatment consists of treating the underlying malignancy and inhibiting the immune responses that cause the signs and symptoms. Certain medications may be prescribed to treat certain symptoms [53].
Prednisone (corticosteroids: inhibits inflammation), Azathioprine, and Cyclophosphamide (immunosuppressants: inhibits or prevents immune system function). Prevention: Strategies for preventing the disorder have not yet been developed. However, early detection can assist to avoid additional difficulties. Cancer can spread to the brain from original tumors located elsewhere in the body, such as the lungs, breasts, or skin (melanoma). Symptoms of brain metastases include headaches, convulsions, cognitive impairment, and localized neurological impairments. Surgery, radiation therapy, chemotherapy, and targeted medicines are among treatments used to manage the condition. Neurology is also strongly linked to primary brain tumors, which develop within the brain tissue itself. Examples include gliomas (such as glioblastoma multiforme), meningiomas, and medulloblastomas. Headaches, seizures, weakness, sensory abnormalities, and cognitive impairment are all neurological symptoms that can be caused by these tumors, depending on their location and size. Surgery, radiation therapy, chemotherapy, and targeted medicines are all potential treatment choices. Several cancer treatments, including chemotherapy, radiation therapy, immunotherapy, and targeted therapies, can have neurological adverse effects [54].
Neurological issues experienced by cancer patients during or after treatment include Chemotherapy-Induced Peripheral Neuropathy (CIPN), cognitive impairment (chemo brain), and radiation-induced brain injury. Management frequently includes supportive care, symptom management, and, on occasion, dose adjustments or treatment modifications. Neuro-oncology is a specialization of neurology and oncology that specializes in the diagnosis and treatment of brain tumors and neurological consequences of cancer. Neuro-oncologists collaborate with neurologists, neurosurgeons, radiation oncologists, medical oncologists, and other experts to offer complete care for patients with brain tumors and accompanying neurological problems [55].
Neurological Complications in Cancer Patients
Neurological issues in cancer patients can vary greatly and may result from the illness itself or its treatment. Brain Metastasis, where Symptoms of cancer spreading to the brain from other parts of the body include headaches, seizures, and changes in mental status. Leptomeningeal metastasis is When cancer cells travel to the membranes that surround the brain and spinal cord, they can cause symptoms like headaches, neck stiffness, and impaired mental function. Spinal Metastasis is cancer that has progressed to the spine, causing pain, weakness, and sensory alterations in the limbs. Paraneoplastic syndromes develop when the immune system mistakenly targets the nervous system in response to cancerfighting components. Symptoms may include muscle weakness, sensory abnormalities, and cognitive impairment. Chemotherapyinduced peripheral neuropathy occurs when certain cancer therapies produce discomfort, numbness, or weakness in the hands and feet. Ischemic stroke is caused by blood coagulation abnormalities or infections associated with cancer or its treatment [56].
Neurological Mechanism
Neuronal Communication occurs when the nervous system communicates using electrochemical signals transmitted by neurons. Neurons receive signals via dendrites, analyze them in the cell body, and send them along the axon as action potentials. At synapses, neurotransmitters are released from the presynaptic neuron and traverse the synaptic cleft to bind to receptors on the postsynaptic neuron, therefore generating a new signal. Neurotransmitters are chemical messengers that carry signals between neurons or from neurons to other cells, such muscle cells or glands. Different neurotransmitters have varying impacts on neuronal activity and play roles in a variety of physiological functions such as cognition, emotion, and motor control. The brain’s capacity to reorganize and adapt in response to experiences, learning, and injury. Neuroplasticity includes structural changes such synaptic pruning, dendritic arborization, and neurogenesis, as well as functional changes in neuronal circuits and connections [57]. Neurodevelopment is the process by which the nervous system grows from embryonic precursors to a sophisticated network of neurons and glial cells. Cell proliferation, migration, differentiation, and synaptogenesis are all controlled by genetic programs, environmental cues, and activity-dependent mechanisms throughout neurodevelopment. Neuroinflammation is the nerve system’s immunological reaction to an injury, infection, or disease.
Neuroinflammation is caused by the activation of microglia, the brain’s immune cells, as well as the production of cytokines, chemokines, and other inflammatory mediators. Acute inflammation protects against infections and promotes tissue regeneration, while persistent neuroinflammation can lead to neurodegenerative illnesses and neurological problems [58]. Neuroendocrinology is the study of how the neurological and endocrine systems interact to govern hormone secretion and physiological functions as metabolism, reproduction, and stress response. Neuroendocrine signals are sent through neurohormones generated by specialized neurons in the brain, which influence hormone production by the pituitary gland and other endocrine organs. Neurovascular coupling is the intimate link between neuronal activity and cerebral blood flow, which ensures that active brain regions receive enough oxygen and nutrients. Neurovascular coupling is characterized by complex signaling processes between neurons, glial cells, and blood arteries that are mediated by neurotransmitters, vasoactive chemicals, and metabolic factors. Understanding these pathways is critical for better understanding the pathophysiology of neurological illnesses and devising tailored therapies to improve neuronal function, increase neuroprotection, and restore neurological health [59].
Conclusion
A wide range of disorders affecting the central and peripheral nerve systems are referred to as neurological diseases, and they offer serious difficulties for patients and medical professionals. Each ailment has its own distinct clinical symptoms and complications, ranging from the crippling cognitive decline of Alzheimer’s disease to the motor dysfunction of Parkinson’s disease, the autoimmunemediated demyelination of multiple sclerosis, and the unpredictable seizures of epilepsy. The wide range of neurological disorders is further expanded by chronic problems like peripheral neuropathy and migraines, acute cerebrovascular events like stroke, and progressive neurodegenerative diseases like Huntington’s disease. Alzheimer’s disease is a primary cause of dementia globally, characterized by cognitive decline and memory loss. Parkinson’s disease is characterized by abnormalities in movement caused by the loss of dopamine neurons. Numerous neurological symptoms are caused by demyelination mediated by the immune system in multiple sclerosis. Recurrent seizures are the hallmark of epilepsy, whereas motor neuron damage from Amyotrophic Lateral Sclerosis causes paralysis and muscle weakness. A cerebrovascular event, such as a stroke, results in abrupt neurological impairments, while migraines induce excruciating headaches. Completing the spectrum are Huntington’s disease, peripheral neuropathy, and traumatic brain injury, each of which poses distinct difficulties in terms of diagnosis and treatment.
Understanding neurological pathways is essential to know the pathophysiology of these conditions and creating successful treatment plans. Neurotransmission, neural communication, neuroinflammation, neuroplasticity, and neurodevelopment are all important processes in both health and illness. Neurovascular connection and the complicated relationship between the neural system and the endocrine system further emphasize the intricacy of neurological regulation and function. Moreover, the relationship between neurology and cancer emphasizes how critical it is to identify and treat neurological side effects in cancer patients. To maximize patient outcomes and quality of life, a multidisciplinary strategy combining neurologists, oncologists, and other experts is required for paraneoplastic neurological syndromes, brain metastases, primary brain tumors, and treatment-induced neurological sequelae. showing potential for enhancing the prognosis and treatment of these difficult illnesses. In the field of neurology and beyond, interdisciplinary collaboration is crucial to tackling the complex nature of neurological disorders and improving patient outcomes.
References
- Feigin VL, Abajobir AA, Abate KH (2017) Global, regional, and national burden of neurological disorders during 1990-2015: A systematic analysis for the global burden of disease study 2015. The Lancet Neurology 16(11): 877-897.
- Feigin VL, Vos T, Alahdab F , Amit AML, Bärnighausen TW, et al. (2021) Burden of neurological disorders across the US from 1990-2017: A global burden of disease study. JAMA Neurology 78(2): 165-176.
- Chin JH, Vora N (2014) The global burden of neurologic diseases. Neurology 83(4): 349-351.
- Erkkinen MG, Kim MO, Geschwind MD (2018) Clinical neurology and epidemiology of the major neurodegenerative diseases. Cold Spring Harb Perspect Biol 10(4): a033118.
- Kelly RR, Sidles SJ, LaRue AC (2020) Effects of neurological disorders on bone health. Frontiers in Psychology 11: 612366.
- Gubert C, Kong G, Renoir T, Hannan AJ (2020) Exercise, diet and stress as modulators of gut microbiota: Implications for neurodegenerative diseases. Neurobiology of Disease 134: 104621.
- Behl T, Kaur G, Sehgal A, Bhardwaj S, Singh S, et al. (2021) Multifaceted role of matrix metalloproteinases in neurodegenerative diseases: Pathophysiological and therapeutic perspectives. International Journal of Molecular Sciences 22(3): 1413.
- Borsook D (2012) Neurological diseases and pain. Brain 135(2): 320-344.
- Butler C, Zeman AZJ (2005) Neurological syndromes which can be mistaken for psychiatric conditions. Journal of Neurology Neurosurgery Psychiatry 76(suppl 1): i31-i38.
- Boersma I, Miyasaki J, Kutner J, Kluger B (2014) Palliative care and neurology: Time for a paradigm shift. Neurology 83(6): 561-567.
- Ortuño MJ, Robinson ST, Subramanyam P, Paone R, Huang YY, et al. (2016) Serotonin-reuptake inhibitors act centrally to cause bone loss in mice by counteracting a local anti-resorptive effect. Nature Medicine 22(10): 1170-1179.
- Nonnekes J, Goselink RJ, Růžička E, Fasano A, Nutt JG, et al. (2018) Neurological disorders of gait, balance and posture: A sign-based approach. Nature Reviews Neurology 14(3): 183-189.
- Duclos H, Desgranges B, Eustache F, Laisney M. (2018) Impairment of social cognition in neurological diseases. Revue Neurologique 174(4): 190-198.
- Tamburin S, Lacerenza MR, Castelnuovo G, Agostini M, Paolucci S, et al. (2016) Pharmacological and non-pharmacological strategies in the integrated treatment of pain in neurorehabilitation. Evidence and recommendations from the Italian consensus conference on pain in neurorehabilitation. European Journal of Physical and Rehabilitation Medicine 52(5): 741-752.
- Pieramico V, Esposito R, Cesinaro S, Frazzini V, Sensi SL (2014) Effects of non-pharmacological or pharmacological interventions on cognition and brain plasticity of aging individuals. Frontiers in Systems Neuroscience 8: 153.
- Shea YF, Pan Y, Mak HKF, Bao Y, Lee SC, et al. (2021) A systematic review of a typical Alzheimer’s disease including behavioural and psychological symptoms. Psychogeriatrics 21(3): 396-406.
- Fowler NR, Judge KS, Lucas K, Gowan T, Stutz P, et al. (2021) Feasibility and acceptability of an acceptance and commitment therapy intervention for caregivers of adults with alzheimer’s disease and related dementias. BMC geriatrics 21(1): 127.
- Postuma RB, Berg D (2016) Advances in markers of prodromal Parkinson disease. Nature Reviews Neurology 12(11): 622-634.
- Muangpaisan W, Mathews A, Hori H, Seidel D (2011) A systematic review of the worldwide prevalence and incidence of Parkinson’s disease. Journal of the Medical Association of Thailand 94(6): 749-755.
- Dobson R, Giovannoni G (2019) Multiple sclerosis-a review. European Journal of Neurology 26(1): 27-40.
- Hauser SL, Cree BA (2020) Treatment of multiple sclerosis: A review. The American Journal of Medicine 133(12): 1380-1390.
- Yuen AW, Keezer MR, Sander JW (2018) Epilepsy is a neurological and a systemic disorder. Epilepsy & Behavior 78: 57-61.
- Milligan TA (2021) Epilepsy: A clinical overview. The American Journal of Medicine 134(7): 840-847.
- Bumas ES (2004) Lou Gehrig's disease and everyone else's. Southwest Review 89(2/3): 253-268.
- (2012) Engdahl S (Ed.), Lou Gehrig's Disease. Greenhaven Publishing LLC, USA.
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, et al. (2017) Heart disease and stroke statistics-2017 update: A report from the American heart association. Circulation 135(10): e146-e603.
- Esmael A, Elsherief M, Eltoukhy K (2021) Predictive value of the Alberta Stroke Program Early CT Score (ASPECTS) in the outcome of the acute ischemic stroke and its correlation with stroke subtypes, NIHSS, and cognitive impairment. Stroke Research and Treatment 2021(1): 5935170.
- Pollock RD, Rafferty GF, Moxham J, Kalra L (2013) Respiratory muscle strength and training in stroke and neurology: A systematic review. International Journal of Stroke 8(2): 124-130.
- Messé SR, Gronseth GS, Kent DM, Kizer JR, Homma S, et al. (2020) Practice advisory update summary: Patent foramen ovale and secondary stroke prevention: Report of the guideline subcommittee of the American academy of neurology. Neurology 94(20): 876-885.
- Katz DI, Bernick C, Dodick DW, Mez J, Mariani ML, et al. (2021) National institute of neurological disorders and stroke consensus diagnostic criteria for traumatic encephalopathy syndrome. Neurology 96(18): 848-863.
- McColgan P, Tabrizi SJ (2018) Huntington's disease: A clinical review. European Journal of Neurology 25(1): 24-34.
- Walker FO (2007) Huntington's disease. The Lancet 369(9557): 218-228.
- Selvarajah D, Kar D, Khunti K, Davies MJ, Scott AR, et al. (2019) Diabetic peripheral neuropathy: Advances in diagnosis and strategies for screening and early intervention. The lancet Diabetes & Endocrinology 7(12): 938-948.
- Castelli G, Desai KM, Cantone RE (2020) Peripheral neuropathy: Evaluation and differential diagnosis. American Family Physician 102(12): 732-739.
- Wang W, Ji Q, Ran X, Li C, Kuang H, et al. (2023) Prevalence and risk factors of diabetic peripheral neuropathy: A population‐based cross‐sectional study in China. Diabetes/Metabolism Research and Reviews 39(8): e3702.
- Kaur A, Jaiswal G, Brar J, Kumar P (2021) Neuroprotective effect of nerolidol in traumatic brain injury associated behavioural comorbidities in rats. Toxicology Research 10(1): 40-50.
- Risdall JE, Menon DK (2011) Traumatic brain injury. Philosophical Transactions of the Royal Society B: Biological Sciences 366(1562): 241-250.
- Maas AI, Menon DK, Manley GT, Abrams M, Åkerlund C, et al. (2022) Traumatic brain injury: Progress and challenges in prevention, clinical care, and research. The Lancet Neurology 21(11): 1004-1060.
- McNamara L, Scott KM, Boyd RN, Novak I (2021) Consensus of physician behaviours to target for early diagnosis of cerebral palsy: A Delphi study. Journal of Paediatrics and Child Health 57(7): 1009-1015.
- McMorris CA, Lake J, Dobranowski K, McGarry C, Lin E, et al. (2021) Psychiatric disorders in adults with cerebral palsy. Research in Developmental Disabilities 111: 103859.
- Vitrikas K, Dalton H, Breish D (2020) Cerebral palsy: An overview. American Family Physician 101(4): 213-220.
- Lord C, Brugha TS, Charman T, Cusack J, Dumas G, et al. (2020) Autism spectrum disorder. Nature reviews disease primers 6(1): 1-23.
- Hirota T, King BH (2023) Autism spectrum disorder: A review. Jama 329(2): 157-168.
- Trouth AJ, Dabi A, Solieman N, Kurukumbi M, Kalyanam J (2012) Myasthenia gravis: A Review. Autoimmune Diseases 2012(1): 874680.
- Narayanaswami P, Sanders DB, Wolfe G, Benatar M, Cea G, et al. (2021) International consensus guidance for management of myasthenia gravis: 2020 update. Neurology 96(3): 114-122.
- Lin Y, Kuang Q, Li H, Liang B, Lu J, et al. (2023) Outcome and clinical features in juvenile myasthenia gravis: A systematic review and meta-analysis. Frontiers in Neurology 14: 1119294.
- Ahuja CS, Wilson JR, Nori S, Kotter M, Druschel C, et al. (2017) Traumatic spinal cord injury. Nature Reviews Disease Primers 3(1): 1-21.
- Lo J, Chan L, Flynn S (2021) A systematic review of the incidence, prevalence, costs, and activity and work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: a 2019 update. Archives of Physical Medicine and Rehabilitation 102(1): 115-131.
- Karim S, Mirza Z, Kamal MA, Abuzenadah AM, Azhar EI, et al. (2014) The role of viruses in neurodegenerative and neurobehavioral diseases. CNS & Neurological Disorders-Drug Targets 13(7): 1213-1223.
- Leblanc P, Vorberg IM (2022) Viruses in neurodegenerative diseases: More than just suspects in crimes. PLoS Pathogens 18(8): e1010670.
- Dhouib IE (2020) Does coronaviruses induce neurodegenerative diseases? A systematic review on the neurotropism and neuroinvasion of SARS-CoV-2. Drug Discoveries & Therapeutics 14(6): 262-272.
- Zhou L, Saksena MM, Saksena NK (2013) Viruses and neurodegeneration. Virology journal 10: 1-17.
- (2017) In: Schiff D, Arrillaga I, Wen PY (Eds.) Cancer neurology in clinical practice: neurological complications of cancer and its treatment. Humana Press Publishing Company, USA.
- Magiera AG, Bobola A, Robek A, Krzystanek E, Gisterek I (2022) Selected neurological complications of oncological treatment-literature overview. Oncology in Clinical Practice 19(5).
- Armstrong C, Sun LR (2020) Neurological complications of pediatric cancer. Cancer and Metastasis Reviews 39(1): 3-23.
- Giglio P, Gilbert MR (2010) Neurologic complications of cancer and its treatment. Current Oncology Reports 12(1): 50-59.
- Teleanu RI, Niculescu AG, Roza E, Vladâcenco O, Grumezescu AM, et al. (2022) Neurotransmitters-key factors in neurological and neurodegenerative disorders of the central nervous system. International Journal of Molecular Sciences 23(11): 5954.
- Baldaia IL, Fernandes VM, Ackerman SD (2020) More than mortar: Glia as architects of nervous system development and disease. Frontiers in Cell and Developmental Biology 8: 611269.
- Liu X, Hua F, Yang D, Lin Y, Zhang L, et al. (2022) Roles of neuroligins in central nervous system development: Focus on glial neuroligins and neuron neuroligins. Journal of translational medicine 20(1): 418.
© 2024. Radwa Abdallnasser Amen. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






