- Submissions

Full Text
Modern Research in Dentistry
Intraosseous Transmigration of Mandibular Premolar into the Mandibular Ramus: A Case Report
Anand Francis Farias, Lynn Lilly Varghese, Kanwardeep kaur and Auric Bhattacharya*
Assistant Professor, Department of Oral and Maxillofacial Surgery, Melaka Manipal Medical College, Malaysia
*Corresponding author:Auric Bhattacharya, Assistant Professor, Department of Oral and Maxillofacial Surgery, Melaka Manipal Medical College, Malaysia
Submission: August 08, 2020;Published: April 26, 2021

ISSN:2637-7764Volume6 Issue2
Abstract
Background: Literature survey indicates that intraosseous transmigration is uncommon. Transmigration of mandibular premolars to distant sites like the ramus are rare and is often detected by chance.
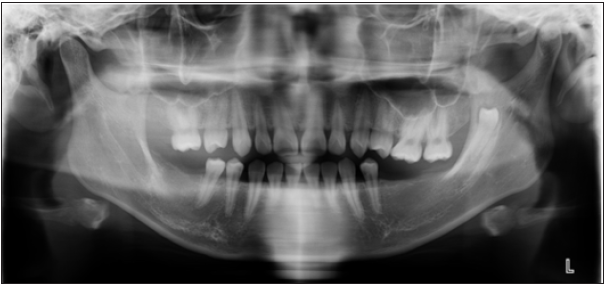
Case description: A 19-year-old female reported seeking replacement of her missing teeth. Clinical examination showed multiple missing teeth and a history of early loss of permanent molars. Panoramic radiographs revealed a transmigrated mandibular premolar in the ramus of the mandible surrounded by well a circumscribed radiolucent area.
Practical implications: Transmigrated premolars in the ramus can cause complications like cystic lesions, weakened ramus, and susceptibility to fracture. Young females undergoing early extraction of permanent molars are at increased risk.
Introduction
Intrabony migration of impacted teeth is a rare phenomenon of unknown etiology.
Peck has reported that the most common teeth to transmigrate are the Mandibular Canines
followed by the Mandibular Second Premolars [1]. The estimated prevalence rate is 0.2% for
the mandibular second premolar [2]. Studies have suggested that there is female predilection.
2, 3 These teeth migrate distally and have been found in the mandibular ramus and coronoid
processes. Unilateral transmigrations are more common [3-5].
Ectopia is defined as “an abnormal congenital or acquired position of an organ or part”.
Ectopic tooth eruption is defined as “a condition in which the permanent teeth, because of
deficiency of growth in the jaw or segment of the jaw, assume a path of eruption that intercepts
a primary tooth, causes its premature loss and produces a consequent malposition of the
permanent tooth” [6]. The term “transmigration” is however, the term assigned to ectopia
when the teeth are present in areas distant from the alveolar process [4].
Case Report
A 19-year-old Chinese female patient reported to the outpatient department requesting
for the replacement of her missing upper and lower back teeth. History revealed that the
teeth were extracted approximately 6 years ago due to dental caries. Clinical examination
revealed that four teeth were missing in the maxillary arch (1,2, 5,12) and seven teeth missing
in the mandibular arch (17,18,19,20,30,31,32). When informed, the patient insisted that
her maxillary right second molar had never erupted and that she had had only four teeth
extracted in her lower arch. The disparity in clinical findings, patient’s history and a need
for comprehensive prosthodontic treatment planning necessitated further radiographic
investigation.
The panoramic radiograph revealed a transmigrated mandibular second premolar
vertically impacted in the left ramus, closer to the anterior border. The crown was facing the
sigmoid notch. The root appeared to be completely formed and parallel to the anterior border
of the ramus. A radiolucent area was visible surrounding the crown suggesting a possible
bony crypt (Figure 1). The tooth was asymptomatic.
Figure 1: Panoramic radiograph showing the transmigrated left 2nd Premolar in the ramus.
Discussion
Intraosseous transmigration of the mandibular premolar is a
rare occurrence with few reported cases in the dental literature [4-
8]. Asymptomatic Transmigration of the teeth poses a diagnostic
challenge, as these teeth are not routinely visible during a clinical
examination or in routine periapical radiographs. Panoramic
radiographs or CBCT are recommended as a diagnostic tool [9].
In the present case, transmigration of missing mandibular second
premolar was a chance finding. It was noticed when panoramic
radiograph was taken to assess the status of the remaining teeth
and bone for a prosthetic treatment plan.
Impacted teeth when left undetected can lead to complications
like cystic lesions, neoplasm, temporomandibular joint disorders
and weakening of ramus, which could increase susceptibility to
fracture. The distally transmigrated mandibular second premolar
was housed in the mid-portion of the left ramus. This is comparable
to other reported cases of transmigration of mandibular second
premolar to the same location [4,5,10].
Several theories have been proposed to explain the
transmigration [9,11,12]. The most likely explanation for
transmigration in the present case could be the early loss of both
the permanent molars. Shapira et al9 suggested that the developing
tooth bud of the mandibular second premolar has a variable degree
of distal inclination under the distal root of the primary deciduous
molar. This distal angulation coupled with the early loss of the
permanent first molar could contribute to transmigration. In the
present case, the patient had experienced early removal of both
mandibular molars, which possibly allowed for a transmigration
path to the ramus of the mandible. The present case was a 19-yearold
female Chinese patient. Mattesson et al. [2] reported that
transmigration of mandibular premolar showed female predilection
(1.7:1 ratio), but no age or racial predilection. Other reasons could
be genetic predilection or idiopathic.
The treatment of a transmigrated tooth depends on the
position of the tooth, symptoms, and infection. The treatment
options include leaving the tooth in-situ if there is no infection or
pain or surgical removal of the tooth if the patient reports pain or if
there is evidence of cystic formations [1,4,7,8,13]. Early, detection
of transmigrating tooth buds can be transplanted as a natural
replacement in young patients with tooth loss [9]. In the present
case, the patient did not report pain, but the presence of bony crypt
warrants a careful observation. Hence, it was decided to leave the
tooth in position and observe the patient during the follow-up
phase of her treatment.
Conclusion
Removal of the mandibular molars before the eruption of the mandibular second premolars is a likely cause for transmigration of the unerupted second premolar. Hence, young female patients who undergo early extraction of permanent first molar should be monitored carefully.
References
- Peck S (1998) On the phenomenon of intraosseous migration of nonerupting teeth. Am J Orthod Dentofacial Orthop 113(5): 515-517.
- Matteson SR, Kantor ML, Proffit WR (1982) Extreme distal migration of the mandibular second bicuspid. A variant of eruption. Angle Orthod 52(1): 11-18.
- Sutton PR (1968) Migrating nonerupted mandibular premolars: A case of migration into the coronoid process. Oral Surg Oral Med Oral Pathol 25(1): 87-98.
- Alves DB, Pedrosa EF, Andreo JC, Carvalho LM, Rodrigues AC (2008) Transmigration of mandibular second premolar in a patient with cleft lip and palate-case report. J Appl Oral Sci 16(5): 360-363.
- Nelson G (1997) Journey through time. Am J Orthod Dentofacial Orthop 111(4): 451-452.
- Nikiforuk G (1948) Ectopic eruption: Discussion and clinical report. J Ont Dent Assoc 25: 243-246.
- Okada H, Miyake S, Toyama K, Yamamoto H (2002) Intraosseous tooth migration of impacted mandibular premolar: Computed tomography observation of 2 cases of migration into the mandibular neck and the coronoid process. J Oral Maxillofac Surg 60(6): 686-689.
- Infante Cossio P, Hernandez Guisado JM, Gutierrez Perez JL (2000) Removal of a premolar with extreme distal migration by sagittal osteotomy of the mandibular ramus: Report of case. J Oral Maxillofac Surg 58(5): 575-577.
- Shapira Y, Kuftinec MM (2003) Intrabony migration of impacted teeth. Angle Orthod 73(6): 738-743.
- Loh HS, Ho KH (1986) Unerupted and ectopic mandibular premolars. Oral Surg Oral Med Oral Pathol 62(3): 358.
- Shapira Y, Mischler WA, Kuftinec MM (1982) The displaced mandibular canine. J Dent Child 49(5): 362-364.
- Miranti R, Levbarg M (1974) Extraction of a horizontally transmigrated impacted mandibular canine: report of case. J Am Dent Assoc 88(3): 607-610.
- Lehman R (1987) A deviate eruption pattern. Am J Orthod Dentofacial Orthop 91(5): 427-428.
© 2021 Auric Bhattacharya. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






