- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Knowledge and Practice of Breast Self-Examination Among Female Health Workers in Northern Sudan
Elsayed Basheer El-haj Elnour1, Hider Osman Jafar Mohammed1, Abdallah Omer1, Motwakil Imam AwadelkareimImam1, Tibyan Abdalmajed Altaher2, Rania Saad Abdulgader Suliman3, Ghanem Mohammed Mahjaf4 and Mosab Nouraldein Mohammed Hamad5*
1Department of Medicine and Surgery, Faculty of Medicine, Shendi University, Sudan
2Department of Clinical Chemistry, Faculty of Medical Laboratory Sciences, Shendi University, Sudan
3Department of Clinical Laboratory Sciences, Prince Sultan Military College for Health Sciences, Saudi Arabia
4Department of Medical Microbiology, Faculty of Medical Laboratory Sciences, Shendi University, Sudan
55Microbiology Department, Faculty of Medicine, Elsheikh Abdallah Elbadri University, Sudan
*Corresponding author:Mosab Nouraldein Mohammed Hamad, Assistant professor, Microbiology Department, Faculty of Medicine, Elsheikh Abdallah Elbadri University, Sudan
Submission:June 23, 2025;Published: September 09, 2025

ISSN: 2577-2015 Volume5 Issue3
Abstract
Background: Cancer is a lethal disease that claims millions of lives each year. Among all types of cancer, breast cancer is the most prevalent and the leading cause of mortality among women in developing countries. In Sudan, its incidence rate is 25.1 per 100,000 population, making it the most commonly diagnosed primary malignancy among women. Breast Self-Examination (BSE) is considered a key method for identifying early breast cancer.
Objectives: To assess the awareness of breast cancer and the practice of self-breast examination among female health workers in Shendi and Al-Matammah towns from November 2023 to January 2024.
Methods: This is a descriptive, cross-sectional, hospital-based study examining awareness of breast cancer signs, risk factors, and the practice of Self-Breast Examination (SBE) among female health workers across all health institutions in Shendi and Al-Matammah localities, involving 335 female health workers to evaluate their knowledge of breast cancer signs, risk factors, and examination practices.
Results: The study was conducted among medical staff in the Shendi locality and involved 335 participants. Thirty-one participants (9.3%) reported not knowing the importance of early detection of breast cancer, while 113 participants (33.7%) stated they have average knowledge, and 191 participants (57.0%) indicated they possess good knowledge.
Conclusion: The prevalence of breast self-examination among healthcare professionals is notably low. This emphasizes the need for ongoing medical education on breast cancer and breast self-examination to enhance the knowledge and skills of female healthcare providers. Continuous medical education programs are urgently needed.
Keywords:Breast self-examination; SBE; Breast cancer; Female healthcare
Introduction
Breast cancer is a disease condition that is characterized by the abnormal growth of cells in the breast [1]. Cancer is a lethal disease that claims millions of human lives every year [2]. Among all cancers, breast cancer is the most prevalent and the leading cause of mortality among women in developing countries [3]. It is estimated that 1 in every 200 women will develop breast cancer before the age of 40 [4]. According to estimates from the international agency for research on cancer, there were 19.3 million new cancer cases and 10.0 million cancer deaths in 2020 [5]. Despite the decline in breast cancer mortality rates over the past 3 decades, the number of women living with breast cancer is expected to continue growing in some regions of the world [6]. In recent years, the growing rates of breast cancer and the rising mortality associated with it have become significant health issues in developing nations [7]. A woman’s lifetime risk of developing breast cancer can be as high as 1 in 10 [8]. The main contributor to the increasing mortality rate is the late diagnosis of the disease, coupled with insufficient early detection initiatives [9]. Late detection and presentations have been caused by several factors, including a lack of organized screening programs, a lack of readily available and efficient treatment choices, a lack of public awareness of breast cancer and environmental screening, and-above allcultural beliefs [10]. Education (to promote early diagnosis) and screening are the two main components of early detection [11]. There are many contemporary screening methods available, including breast magnetic resonance imaging, sonography, and mammography [12]. Other techniques for identifying any changes in the breast include Self-Breast Examination (SBE) and Clinical Breast Examination (CBE). In SBE, the lady examines and feels her breasts for lumps, size, shape, texture, and contour.
This is done so that any woman can learn about the geography of her breasts, understand how they feel normally, and recognize any changes in the future. According to reports, SBE has a beneficial impact on the early identification of breast cancer, although its sensitivity and specificity values are challenging to ascertain [13]. One benefit of SBE is that it’s a straightforward, low-cost, noninvasive technique that helps women understand their breasts and identify any changes [14]. Because of the drawbacks of frequent breast healthcare visits, a higher number of benign biopsy results, more biopsies that increase the risk of breast cancer, and higher healthcare expenses, recent studies no longer advise using SBE for breast cancer screening as they once did [15]. By providing positive role models, promoting social norms that are favourable to screening, and assisting in the development of supporting institutional policies, health workers play a significant role in fostering an environment that supports screening behaviours [16]. Globally, breast cancer is the most prevalent cancer to be diagnosed in women. In Africa, it typically manifests much later than in Europe. In Sudan, as in the rest of Africa, it is the most prevalent primary cancer in women and typically manifests as stage III or stage IV disease. This study is intended to analyse the level of breast cancer awareness among women in Sudan.
Methodology
a. Study design: This descriptive, cross-sectional, hospitalbased study examined the awareness of breast cancer signs, risk factors, and Self-Breast Examination (SBE) practices among female health workers in all health institutions in the Shendi and Al-Matammah localities. Three hundred thirty-five female health workers participated to assess their awareness of breast cancer signs, risk factors, and SBE practices from November 2023 to January 2024.
b. Study area: Shendi is a city in northern Sudan on the east bank of the Nile, 150 km northeast of Khartoum. It is also about 45 km southwest of the ancient city of Meroe. Located in River Nile State, Shendi serves as the center of the Ja’aliin tribe and is an essential historic trading hub. The population of this town is estimated to be 55,516 people according to the 2007 census. Al-Matama is a city in the Nile River state in northern Sudan, at 379 meters (1,243.43 feet) above sea level and 152 kilometers (94.44miles) away from Khartoum. El-Mak Nimer Hospital, Shendi Teaching Hospital, and the Tumour Therapy and Cancer Research Center (TTCRC) in Shendi are specialized facilities affiliated with Shendi University. Aliaa Hospital is located in Al- Matammah
c. Study population: This study focuses on female health workers in the towns of Shendi and Al-Matammah.
d. Sample size: Three hundred thirty-five female health workers participated in this study.
e. Data collection: The researchers developed a standard closed-ended interview questionnaire based on available literature to investigate the awareness of signs and risk factors of breast cancer and the practice of SBE among female health workers.
f. Data collection technique: Data was collected over 3 months. A female health professional filled out each questionnaire.
g. Data Analysis: The collected data were statistically analyzed using SPSS version 28, with the correlation test, oneway ANOVA, and logistic regression analysis; a P-value of less than 0.05 was considered significant.
Result
This is a cross-sectional, hospital-based study to assess awareness of the importance of early detection of breast cancer. The study involved 335 medical staff participants from the Shendi locality. Three hundred thirteen participants (93.4%) have heard of breast self-examination, while 22 participants (6.6%) have not. Additionally, 272 participants (81.2%) know how to perform breast self-examination, whereas 63 participants (18.8%) do not. One hundred eighty-one participants (54.0%) perform breast selfexamination, while 154 participants (46.0%) do not (Table 1). Eighty participants (24.0%) have a family member who has had breast cancer or been exposed to it, while 254 participants (76.0%) have not. Among those with a family history of breast cancer, 35 participants (43.75%) consulted a doctor or visited a specialized center, while 45 participants (56.25%) did not (Table 2). Sixteen participants (4.8%) believe that the most at-risk age group for breast cancer is under 20 years old, 138 participants (41.2%) think it is from 20 to 40 years old, and 181 participants (54.0%) say it is over 40 years old (Table 3). Two hundred seven participants (61.8%) think most breast lumps affecting women are not cancerous, while 57 participants (17.0%) disagree, and 71 participants (21.2%) are unsure (Table 4). Regarding the best time for self-examination, 253 participants (75.5%) said it is monthly after menstruation, 42 participants (12.5%) said it is monthly before menstruation, and 40 participants (11.9%) said once yearly (P value=0.000) (Table 5).
Table 1:Knowledge and practices related to Breast Self-Examination (BSE) and breast cancer screening methods.
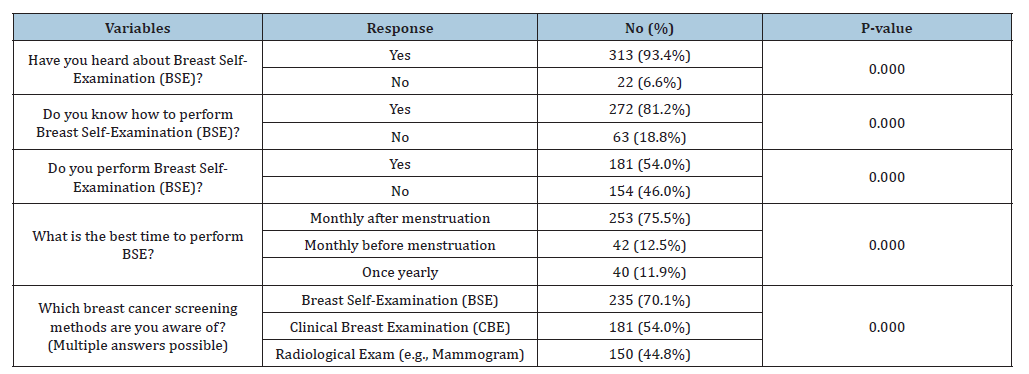
Table 2:Family history and medical consultation behavior regarding breast cancer.
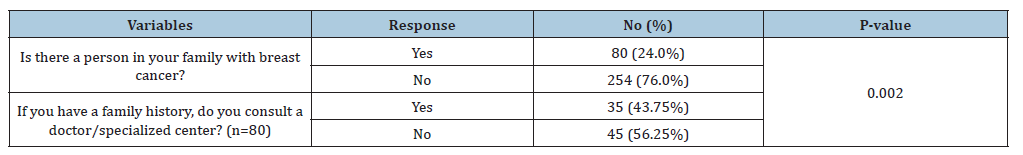
Table 3:Knowledge of the age group at highest risk for breast cancer.
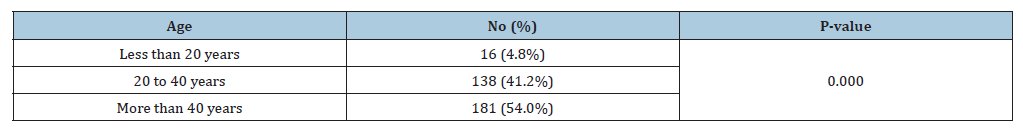
Table 4:Knowledge about the nature of breast lumps.
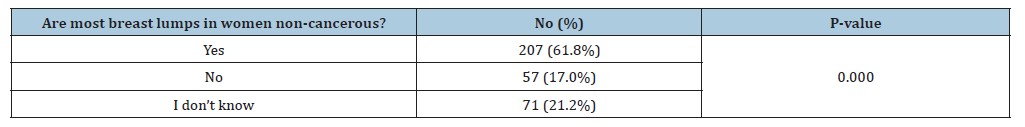
Table 5:Participants’ knowledge of true breast cancer risk factors and common misconceptions.
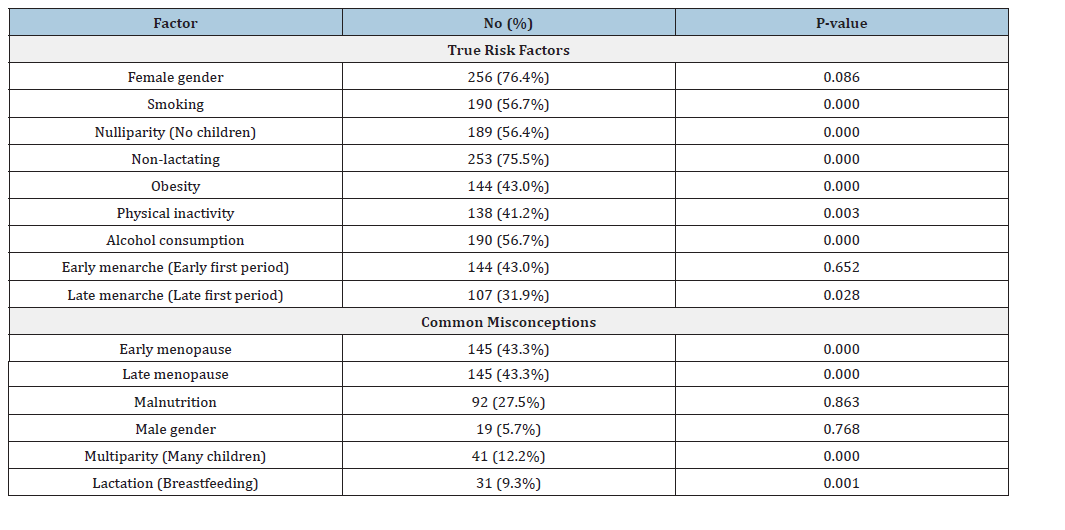
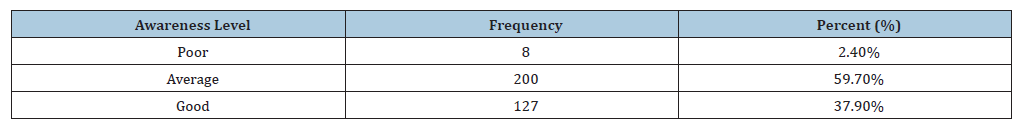
Concerning breast cancer screening methods, 181 participants (54.0%) are aware of clinical breast examinations, 235 participants (70.1%) know about self-examination, and 150 participants (44.8%) are aware of radiological examinations (P value=0.000) (Table 6). Regarding breast cancer risk factors, participant responses were as follows: “Female gender” was noted by 256 participants (76.4%) (p value=0.086), “male gender” by 19 participants (5.7%) (p value=0.768), “late menarche” by 107 participants (31.9%) (p value=0.028), “early menopause” by 144 participants (43.0%), “late menopause” by 145 participants (43.3%), “nulliparous” by 189 participants (56.4%), “multiparous” by 41 participants (12.2%), “lactation” by 31 participants (9.3%), “non-lactating” by 253 participants (75.5%), “obesity” by 144 participants (43.0%), “smoking” by 190 participants (56.7%), “malnutrition” by 92 participants (27.5%), “alcohol consumption” by 190 participants (56.7%), and “physical inactivity” by 138 participants (41.2%). Overall, based on participant responses, 8 participants (2.4%) have poor awareness regarding the early detection of breast cancer, 200 participants (59.7%) have average awareness, and 127 participants (37.9%) have good understanding.
Table 6:Overall awareness level regarding early detection of breast cancer.
Discussion
Breast cancer is the most prevalent type of cancer in women globally and the primary cause of cancer-related deaths among this demographic. An anticipated 2.3 million additional cases are reported by GLOBOCAN (2020) [5]. Almost one out of every twelve women will get breast cancer at some point in their life. Up to 2020, around 685,000 women died from breast cancer, making it the largest cause of cancer-related deaths in women [17]. Most of the participants had heard about breast self-examination (93.4%) and knew that early diagnosis can save the patient’s life (92.2%), but only about half of them perform it (54.0%). Compared to a study involving female medical graduates in the Majmaah University in Saudi Arabia, which showed that only about 28.4% perform it [18]. Most of the participants who have a family history of breast cancer had not consulted a doctor or visited a specialized center (56.25%). Less than a third of participants know that looking for lumps is not the sole purpose of self-examination (31.1%), and about half of the participants know the age group at more risk (54.0%). Slightly more know that most breast lumps in women are not cancerous (61.8%) and the best time for breast self-examination (75.5%). Concerning breast cancer screening methods, the most well-known method is breast self-examination (known by 70.1% of participants), followed by clinical breast examination (known by 54.0% of participants), and lastly radiological examination (known by 44.8% of participants). Regarding risk factors of breast cancer, the most well-known risk factor by participants is female gender (76.4%), followed by smoking (56.7%). The latter ratio is very consistent with a study conducted among female students at the University of Sharjah by Syed Azizur Rahman, Amina Al–Al-Al- Marzouki, et al, in which smoking was correctly identified as a risk factor by (59.3%) [19].
The least known risk factor is late menarche (31.9%), followed by early menarche and obesity (43.0% for both), compared to (40.2%) and (25.7%) of participants in the previous study have identified late menopause and obesity, respectively, as risk factors of breast cancer. The most commonly falsely believed factor to increase the risk of breast cancer is early menopause (43.3%), followed by malnutrition (27.5%). Overall, we found that almost a third of participants have good awareness regarding early detection of breast cancer (37.9%), and most of them have average awareness (59.7%). Only a few participants have poor awareness (2.4%). In contrast to a study conducted on female medical graduates in Majmaah University in Saudi Arabia, the study showed that (37.1%) have good awareness, (42.2%) have average awareness, and (20.7%) have poor awareness [18]. Concerning Awareness and practice of self-breast examination among female nurses at the Federal Teaching Hospital Ido-Ekiti, Nigeria, More than half (64.7%) of the nurses in this study had good knowledge of the warning signs of breast cancer, only 15.3% of the respondents had good knowledge of breast cancers which include ninety nurse which is less than our study which include 335 female health worker that show Two-hundred fifty-eight participants (77.0%) said they know the first signs of breast cancer, while 77 participants (23.0%) said they don’t know [20]. Primary health care nurses’ knowledge practice and client teaching of early detection measures of breast cancer in Ibadan show 120 nurse at primary health care center revealed that though 80.9% acknowledged BSE as an early diagnostic modality, but only 40.8% were aware of the correct timing of performance of BSE regarding to our study Concerning the best time for a self-examination, 253 participants (75.5%) said it is monthly after menstruation, 42 participants (12.5%) said it is monthly before menstruation and 40 participants (11.9%) said once yearly [21].
Conclusion
The prevalence of breast self-examination among healthcare professionals was only 54% of health workers who practiced SBE. This highlights the necessity for continuous medical education on breast self-examination and breast cancer to improve the understanding and practice of female healthcare professionals.
Recommendation
Women can undergo the desired change with the help of a community-based educational intervention program that emphasizes the value of early detection in the treatment of breast cancer. Advertising campaigns on WhatsApp /radio discussing the importance of early detection of breast cancer, as well as the significance of monthly self-examinations and how to perform breast self-examinations and how to perform breast selfexamination.
Limitations
Because the population surveyed consisted of health personnel, who are probably more knowledgeable about health issues than the general public, study bias was probable. Additionally, since the goal of this study was to examine the participants’ shared views, it is impossible to completely rule out the possibility that alternative beliefs within the community were overlooked.
Acknowledgement
We deeply appreciate the contributions of all respondents who participated in our survey.
Consent
The patient’s written consent has been collected.
Ethical Approval
The Department of Community in the College of Medicine, Shendi University, approved the study. The study matched the ethical review committee. The aims and benefits of this study were explained with the assurance of confidentiality. All protocols in this study were done according to the Declaration of Helsinki (1964).
References
- (2021) What is breast cancer? Centers for disease control and prevention.
- Malvezzi M, Carioli G, Bertuccio P, Levi F, Negri E, et al. (2019) European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann Oncol 30(5): 781-787.
- Bray F, Ferlay J, Joannie LT, Anderson BO, Jemal A, et al. (2015) International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev 24(10): 1495-1506.
- Jones AL (2006) Fertility and pregnancy after breast cancer. Breast Suppl 2: S41-S46.
- Sung H, Ferlay J, Siegel RL, Jemal A, Bray F, et al. (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3): 209-249.
- Baijal P, Periyakoil V (2014) Understanding frailty in cancer patients. Cancer J 20(5): 358-366.
- Modeste NN, Drayton VLC, Montgomery S (1999) Barriers to early detection of breast cancer among women in a Caribbean population. Rev Panam Salud Publica 5(3): 152-156.
- Salem OAA, Hassan MA (2007) Breast self-examination among female nurses in Jordan. Shiraz E-Med J 8(2): 51-57.
- Pinotti JA, Barros AC, Hegg R, Zeferino LC (1993) Breast cancer control programme in developing countries. Eur J Gynaecol Oncol 14(5): 355-362.
- Wadler BM, Judge CM, Prout M, Allen JD, Geller AC (2010) Improving breast cancer control via the use of community health workers in South Africa: A critical review. J Oncol 2011: 1-8.
- (2010) World Health Organization (WHO). Screening and early detection of cancer.
- Misauno MA, Anosike IH, Ojo EO, Ismaila BO (2011) Knowledge and attitude to breast self-examination among a cohort of medical students in Nigeria. J Med Trop 13(1): 32-35.
- Phillips JM, Wilbur J (1995) Adherence to breast cancer screening guidelines among African-American women of differing employment status. Cancer Nurs 18(4): 258-269.
- Miedema BB, Tatemichi S (2003) Breast and cervical cancer screening for women between 50 and 69 years of age: What prompts women to screen? Women's Health Issues 13(5): 180-184.
- Kevin CO, Smith RA, Ruth E, James SM, Louise CW, et al. (2015) Breast cancer screening for women at average risk: 2015 guideline update from the American cancer society. JAMA 314(15): 1599-1614.
- Bastani R, Marcus AC, Hollatz BA (1991) Screening mammography rates and barriers to use: A los angeles county survey. Prev Med 20(3): 350-363.
- Shang C, Xu D (2022) Epidemiology of breast cancer. Oncologie 24(4): 649-663.
- Mohamed EY, Sami W, Almutairi AM, Tahir A, Alhusainy KM, et al. (2016) Breast cancer awareness and breast self-examination among future female university graduates: Comparison between medical and nonmedical students. Int J Res Med Sci 4(3): 685-689.
- Rahman SA, Otim M, Amina AM, Yousuf R, Rahman P, et al. (2019) Awareness about breast cancer and breast self-examination among female students at the university of Sharjah: A cross-sectional study. Asian Pac J Cancer Pre 20(6): 1901-1908.
- Gabriel OE, Ajetunmobi OA, Shabi OM, Toyin EO, Dada AS, et al. (2016) Awareness and practice of self-breast examination among female nurses at the federal teaching hospital ido-ekiti, Nigeria. J Public Health Afr 7(1): 528.
- Oluwatosin O (2012) Primary health care nurses' knowledge practice and client teaching of early detection measures of breast cancer in Ibadan. BMC Nurs 11(22): 1-8.
© 2025 Mosab Nouraldein Mohammed Hamad. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






