- Submissions

Full Text
Gerontology & Geriatrics Studies
Mental Health Problems Posed by COVID-19
James Paul Pandarakalam*
Consultant Psychiatrist, Immunopsychiatry Study Centre, Lea Court Independent Hospital, UK
*Corresponding author: James Paul Pandarakalam, Consultant Psychiatrist, Immunopsychiatry Study Centre, Lea Court Independent Hospital, UK
Submission: May 10, 2021;Published: May 25, 2021

ISSN 2578-0093Volume7 Issue1
Abstract
Background: The impact of COVID-19 pandemic on global population is beyond description. The impact of the ongoing pandemic on mental and physical health, jobs and relationships could be catastrophic warranting collective actions. A sound knowledge of all aspects of COVID-19 becomes essential to deal with the aftermaths of this unprecedented pandemic and mental health professionals will have to refresh their knowledge of virology and immunology. Historically, epidemics have substantial effect on mental health. Senior citizens have been deemed to be more vulnerable to COVID infection and they are the ones who had to bear the main brunt of this epidemic.
Aim: To evaluate the magnitude of mental health impacts of COVID-19 among the psychiatric population, public and health professions as well as to gain some useful insights into the associated predictor factors of COVID-19.
Materials and methods: Published studies concerning mental health problems associated with the COVID-19 outbreak and other previous global infections have been considered and reviewed. Selective survey of the literature including narrative reviews to collect different interpretations which also help to form a framework to study the psychiatric implications of the ongoing pandemic has been carried out. Psychological, psychopathological, and neurological effects are separately analysed.
Results: The immune response to SARS-CoV-2 itself can directly result in psychiatric sequelae or by the morbid psychological factors and in some case both factors precipitate psychiatric symptomatology. Most of the people infected with COVID-19 might not pose any major mental health issues, even among those with extreme cases that require hospitalization, yet some are conceivably vulnerable to mental health issues. It has been observed that severe inflammation leads to worse depression. Everybody has to address transient psychological problems that require development of new coping strategies, but patients with enduring mental illness need additional support. Social isolation and the loneliness due to physical distancing rules have a negative impact on the mental health of geriatric population compared to the young people.
Conclusion: COVID-19 infection poses alarming impact of on mental health. It is feared that this toxic viral infection would result in a surge of cases of anxiety disorders, PTSD, and depression, and lead to an amplification of existing mental health issues. The current insights on immune-inflammation in psychiatry need further elaboration to assess the psychopathology of COVID-19 survivors. The neurotoxic effects due to the cytokine storm, an autoimmune reaction occurring in some cases of COVID-19 evokes a renewed interest in the viral and autoimmune aetiology of a subset of schizophrenia.
Keywords: COVID-19; PTSD; Depression; Anxiety; OCD; Bereavement; Neurotoxicity; Mental health; Geriatric population
Introduction
The impact of the current pandemic on mental health is expected to be very profound [1]. The pandemic has immediate and long-term psychological impacts. Available data suggest that confusion and delirium are common features in the acute stage of COVID-19 and the data collection on psychopathological aspects in the post-illness period is still evolving [2,3]. Patients with COVID-19 are at accelerated risk for delirium due to several reasons [4]. According to Kotfis et al. [4] these factors include direct Central Nervous System (CNS) invasion, induction of CNS inflammatory mediators, secondary effect of other organ system failure and effect of sedative strategies. Prolonged mechanical ventilation time, immobilization, and other needed but unfortunate environmental factors including social isolation and quarantine without family are also contributing causes. The immune response to the virus SARS-CoV-2 itself can directly result in psychiatric sequelae or by the morbid psychological factors such as psychological effect of a new severe and potentially fatal illness, fears about infecting others, and stigma; psychiatric consequences to COVID-19 can be caused by all these factors [5]. People affected by COVID-19 may have a high burden of mental health problems, including anxiety disorders, depression, panic attack, stress reactions, irrational anger, impulsivity, somatization disorder, sleep disorders, emotional disturbance, posttraumatic stress symptoms, and suicidal behavior.
Aging occurs when immunity weakens. The geriatric population obviously have reduced immunity which makes them highly vulnerable to COVID-19 and there also other co-morbid factors. Lockdown measures to curb the pandemic have resulted in worsening of social isolation and loneliness in the elderly population and such a situation is associated with significantly increased morbidity and mortality among them. Technologybased social interactions with loved ones, engaging in physical activity, spiritual or religious prayers and activities remotely, and community services have been helpful to minimize social isolation and loneliness [6]. In spite of such efforts, the geriatric population have been the real victims of the pandemic. While many older adults are adjusting to COVID-19 restrictions, some are really struggling to address the psychological suffering and unmet medical needs with persistent loneliness [7]. Social isolation and loneliness in the older adults are associated with negative outcomes including anxiety, depression, cognitive decline, and mortality [8]. This paper narrates the psychiatric concerns posed by the COVID-19 pandemic among the population as a whole including the older adults.
Vulnerable Groups
Subjective feelings of stress have individual variations and accordingly, stress responses also diverge in different individuals. Such a conjecture has neurophysiological basis. A recent MRI scanning of brain revealed that enhanced subjective feelings were associated with more active functional neural connection between the hippocampus and the hypothalamus whereas more active functional connectivity between the hippocampus and the lateral prefrontal cortex were associated with lower levels of feelings of stress [9]. The unprecedented stress of the ongoing pandemic affect people differently and they riposte variably. People who are disproportionally exposed to risk are considered vulnerable and this group can change dynamically. Thus, people who are not considered vulnerable at the onset of the pandemic can become vulnerable depending upon what life brings to them during the course of the pandemic and are always at risk of developing mental health problems.
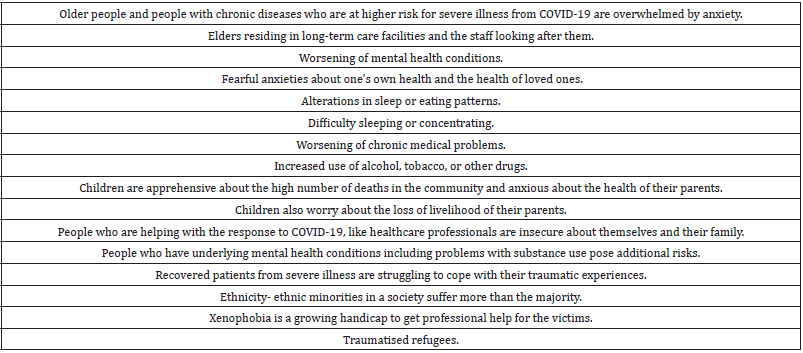
COVID-19 affects all sets of people in society, but individual responses are variable. Subsyndromal mental health problems are a common response to the COVID-19 pandemic and certain groups of the population have been identified as particularly vulnerable to mental health issues associated with the COVID-19 pandemic [10]. The vulnerable groups identified include older adults [11], the homeless [12], migrant workers [13], the mentally ill [14,15], pregnant women [16] and Chinese students studying overseas [17] or overseas students as a whole. A particularly vulnerable community that has received relatively little attention is elders residing in long-term care facilities [18]. The staff looking after these senior members of the community are also highly vulnerable because of high infection rate in such settings and the close contact with the residents. The above studies are country based and do not reflect the global psychological aftermath of the pandemic but alert the world community to take special precautions for rescue of the mentally afflicted (Table 1). Ethnic minorities and young people are taking a disproportionate financial and employment hit from the coronavirus pandemic and the psychological impact is still unknown. The pandemic has intensified the challenges and struggles for patients with geriatric population, intellectual disabilities, and neurodevelopmental disorders in creating the normal out of chaos. Senior adults are understood to experience loneliness, age discrimination, and unwarranted worry. Consequently, greater negative outcomes related to the COVID-19 pandemic given their increased isolation and risk for complications than younger adults have been anticipated [19].
Table 1:Vulnerability factors.
Anxiety,Depression and Behavioural Problems
Several psychosocial stressors have been found to be induced by COVID-19. Globally, the behavioral and emotional health of people have been affected by the current pandemic. It has evoked antisocial behavior, fear, paranoia, and anxiety in people. There might be lasting effects of psychological and emotional issues including Post-Traumatic Stress Disorder (PTSD), depression, and cognitive impairments on ventilator-dependent patients. The pandemic has created so many uncertainties which together with the fear of infection can fuel anxiety, and thereby influencing paranoia [20]. In a study by Mazza et al. [5] 402 adults surviving COVID-19 were followed up for psychiatric symptoms and observed that a significant proportion of patients self-rated in the psychopathological range: 28% for PTSD, 31% for depression, 42% for anxiety, 20% for OCD symptoms, and 40% for insomnia and female patients scored more for both anxiety and depression [5]. During the follow-up, the researchers observed that the baseline systemic immune-inflammation index, which reflects immune and systemic inflammation responses positively associated with depression and anxiety scores. They also pointed out that patients who have had a positive previous psychiatric diagnosis showed increased scores on most psychopathological measures, with similar baseline inflammation.
Results from a study evaluating the effect of COVID-19 on depression levels among adults in the US showed that during the pandemic, symptoms were almost three times higher and that among those already at an increased risk of infection, the burden of infection was greatest [21]. The study by a team from the Boston School of Public Health, Massachusetts, used two population-based surveys of US adults aged 18 years and over. The study data revealed that 8.5% of adults had depression before COVID-19 and during the pandemic, this increased to 27.8%. Likewise, the prevalence of both mild (24.6% vs 16.2%) and severe (5.1% vs 0.7%) depression increased during the pandemic. Worthy of note is the association of a higher incidence of depression with lower income, lower savings, and vulnerability to stressors such as a job loss [22].
Many COVID-19 patients, especially those in Intensive Care Units (ICU), are seriously affected by anxiety. For example, after some patients have gained consciousness, they can be terrified, and may think that they have gone out of mind or there is a conspiracy to steal their organs or to torture them. Patients with sleep deprivation, hallucinations, and nightmares were also at a higher risk of developing psychological disorders. Isolated cases of first episode psychosis have been reported following COVID-19 infection [23,24]. Internet betting and domestic abuse may become the consequence of being isolated in the house, prompting relationship breakdowns [25]. COVID-19 has brought about the pandemic of loneliness - the most dangerous threat to our survival is the feeling of being excluded and rejected. When people are walking through the “valley of death,” only a drop of love or human touch can fill their empty hearts. Crisis often affects the human mind in crucial ways, increasing threat arousal and snowballing the anxiety; rational and logical decisions are replaced by subjective and flawed decisions [26].
Feinberg ME et al. [27] collected data from 129 families with children for whom the average age was 9.9 years [27]. They noted that there was a clear change towards worsening of measures compared with data obtained before the pandemic. The authors noted that the data were consistent with elevated levels of parent and child stress and mental health difficulties during the pandemic. Such findings warrant a need for a more widespread family intervention to reduce both parental and child mental health and behavioral problems through screening as these problems were likely to persist after the pandemic [27].
PTSD, Suicides
A sizeable number of people will develop PTSD which is being seen among patients who have recovered after being seriously ill with COVID-19. The risk of PTSD among frontline health workers and social care workers are extremely high and is at par with soldiers returning from war zone or surviving other mass casualty events. High risk group of developing COVID related PTSD and mental health problems may include patients with severe disease, health and social care workers witnessing high numbers of patient deaths, those who have lost their loved ones due to COVID-19, and patients with existing psychiatric illness. Tang et al. [28] investigated the PTSD and depressive symptoms in the 2485 participants from 6 universities using online survey versions of the PTSD Checklist Civilian Version and the 9-question Patient Health Questionnaires (PHQ-9), and data on sleep durations, exposure, home-quarantine time, and socio-demographic variables were also collected [28]. They found that the PTSD and depression prevalence were 2.7% and 9.0%. Subjectively, feeling extreme fear was the most significant risk factor for psychological distress, followed by short sleep durations and living in severely afflicted areas. Sleep durations was a mediator between exposures and mental health problems [28].
The pandemic could negatively affect the known suicide precipitants. History has it that viral epidemics have brought about a spike in suicides. It is reported that of the recovered cases of the SARS pandemic, 50% of the patients are still in the condition of anxiety and apprehension, and there has been an increase of 30% in suicides among patients aged 65 and above [29]. There is ample psychiatric literature supporting the increasing rate of COVID-19 related suicides [30,31]. A career in medicine comes with a huge strain in the best of times [32]. Economic problems caused by the COVID-19 pandemic will most likely be a factor to an increase in suicide rate [33]. The psychiatric toll of the COVID-19 crisis will gradually unfold in the coming years as the consequences of chronic anxiety, prolonged distress, physical distancing, loneliness, death of loved ones and job losses manifest.
Obsessive Compulsive Disorder
Rigid handwashing and the fear of developing an infection can be associated with symptoms of obsessive disorder [34]. The impact of handwashing procedures in preventing toxic pathogens among OCD sufferers is yet to be understood. As the ongoing pandemic breeds uncertainties, OCD may be exacerbated. Excess hand washing is encouraged during the pandemic and it seems to have a detrimental effect on individuals who are plagued with the thoughts of contamination and extreme cleanliness. Some patients are washing their until they bleed and crack. One such patient has remarked that she could see germs on her hands whenever she looked at them. Patients with OCD are known to have obsessive thoughts of contamination fear. There are case reports of OCD patents who have been well-controlled prior to the outbreak of COVID-19 have presented acutely with a significant exacerbation of OCD symptoms precipitated by media reports of COVID-19 [35].
Over one-third of the patient sample in an Italian study reported a significant emergence of new obsessions since the pandemic and compulsions phenotypes along with a significant exacerbation of past ones [36]. They were more frequently found to experience suicidal ideation, increased internet checking, sleep disturbances, avoidance behaviors, and work difficulties warranting therapy adjustments. Advice on measures of precaution provided by print media, social media, and electronic sources are radically repetitive, and in individuals suffering from OCD, these can result in mental health anxiety [37]. They get disturbed as they struggle to cope with new routines such as washing and sanitizing hands and wearing masks or gloves, being added to their usual routines. The media is adding to the confusion that OCD sufferers already have by portraying that coronaviruses as entities that possess human-like characteristics. An individual’s identity is violated or threatened by such a depiction. These life forms can threaten the self as the result of a fear of inner corruption characterizing those with OCD and the person with OCD may act as if they are acting upon reality when they fear contagion but are in effect only acting upon an underlying fear of inner corruption that is confused with reality itself [38].
OCD sufferers fighting compulsions along with the corona fears have become the normal. Keeping busy has been the natural distraction for OCD sufferers and during this time of restricted social activities, they do not get any respite [39]. The pandemic is leaving them panicking as a result of so much panic around. Patients who previously found some form of self-acceptance through the human contact in the National Health Service (NHS) network are missing it because of the imposed seclusion of the pandemic. The mental health of OCD sufferers as well as their state of relaxation is impacted adversely by the routine measures put in place to prevent COVID-19 outbreak. There ought to be therapy adjustments to deal with the new obsessions.
Substance Abuse
Addiction to alcohol and drug especially opioid abuse, has been reported to be seriously high due to the pandemic. Substance abusers have seized on the coronavirus pandemic as a rare opportunity or excuse to rationalize their problem. Covid-19 coupled with its uncertainty, isolation, and financial distress poses high-risk for developing a substance abuse disorder, or relapsing. It looks as though a silent and long-existed pandemic has been inserted into the newly arrived Corona pandemic. The drug-seeking behaviors due to the isolation brought about by the pandemic could increase exposure to infection for addicts, their families, and healthcare professionals [40]. The development of alcohol use disorder in atrisk individuals, alcohol misuse, and relapse may increase during this period of isolation [40]. There are signs that individuals with the alcohol issue are expending liquor far in abundance as adapting the system to manage the isolation and loneliness. For them, reliance will be additionally activated by mourning, job insecurity or failed relationships.
Considering that SARS-Cov-2 affects pulmonary function, the co-occurrence of substance use disorder and COVID-19 could be particularly lethal. A US study has elaborated this risk by referring to the statistics that 10.8% of adults in the US have a substance use disorder including alcohol and tobacco and chronic use of tobacco, alcohol and other drugs is associated with cardiovascular, pulmonary, and metabolic diseases all of which are risk factors for COVID-19 infection and for worse outcomes [41]. Preliminary reports regarding higher risk for adverse outcomes with COVID-19 and smoking have been inconclusive and currently there is little research on the effects of other drugs including opioids, by individuals with a substance use disorder. As a result of a possible compromised pulmonary health, they may be more vulnerable to respiratory complications of COVID-19. At the start of lockdown, in the streets of London, a different scenario unfolded where 5600 rough sleepers were accommodated with various co-morbidities including substance misuse. There was a sudden disappearance of the begging money, a scarcity of class A drugs and dealers had no way to buy cheap alcohol. The local GPs who were not opiate-substitution specialists had to face bewildered patients withdrawing from drugs and alcohol and needing urgent support [42].
Grief, Bereavements
The words grief and bereavement are commonly used interchangeably, but these words differ slightly in meaning. Grief results from the loss of anything that is of intrinsic value and figuratively, it is the penance one has to pay for enjoying love and attachments. Our response to this loss is called grief while the entire process of grief is referred to as bereavement. To put it differently, grief can be described as though it is like reaching out for something that is familiar, only to find that when we need it one more time, it is no longer there. Corona pandemic has broken many loving hearts and resulted in massive grief reactions during its global destructive march. Dying with someone present by the bedside has considerable social and existential consequences for both patients and families [43]. One can just envision the self-blame sentiments and guilt feelings of the bereaved who were forced to leave the dying in their final transition.
Young people and children are affected by grief in various ways depending on their age, their level of understanding, and the changes the death means for their daily life. They regularly feel floods of powerful emotions like misery, blame, stun, and anger, which they may battle to communicate. Having thoughts that are stressful over other people and deciding to change one’s behavior is normal and acceptable. It is a difficult task to support a child when parents themselves are lamenting. The way out is to listen attentively and carefully and to answer questions appropriately. The renowned Irish grieving custom of “wake” that had a restorative impact has gotten confined in Ireland because of the pandemic regulations. A deferred epidemic of obsessive distress and depression is envisaged by mourning advisors [44]. It is the absence of the onetime presence and relationship of people who have left us in death that hurts most, and people feel left alone in a desolate island because of the pandemic. The grieving people feel disconnected in loneliness. When emotional storms hit someone, instead of leaning on the community, they suffer alone in the pandemic which has deprived everyone the anchor of mutual connections.
During mourning period, normally people go back to their friendly groups over and over creating a ritual. They spend quality time with this ritual where people gather around a fire or in a prayer circle and engage in talking openly about the qualities of the dead loved ones, sharing the fond memories, and the happy as well as sad times spent together, grieving, and externalizing the pent-up feelings. It is all about forming a micro community with kindred spirits, a sort of tiny temporary sanctuary. Many people had to go through the hardest time of life because of the loss of close friends or much-loved family members, during this self-imprisonment imposed by the lockdown unable to find an intellectual and spiritual way out.
Amplification of Symptomatology
Patients who are already suffering from psychotic conditions are expected to show a higher burden of the disease. Worsening of existing mental health conditions, substance abuse, and grief reactions can be regarded as a consequence of this pandemic. As in the case of other major social crises, this pandemic will color the psychotic symptomatology of patients. “Covid paranoia” is already in the scene. Those suffering from psychotic disorders could be more vulnerable to subsume COVID-19 related threat preoccupations into their delusional systems [45]. A lot of psychiatric patients may not be able to adhere to the preventive measures of COVID-19 due to cognitive deficits and they can put themselves at risk of the toxic pathogenic infections. Bipolar and schizophrenia sufferers are at a higher risk. In order to alleviate the pandemic stress, some patients are already requesting for extra anxiolytics and hypnotics. The pandemic may present new and difficult challenges for patients who are already suffering from psychotic disorders or other mental health issues. Increased social isolation, loneliness, health anxiety, stress, and an economic downturn are a lethal combination that will adversely affect the existing mental health problems.
Patients with severe mental disorders have been reported to react to the pandemic and the lockdown restrictions with higher anxiety levels compared to the general public, and this suggests that this domain could be a gauge for early intervention strategies and closer follow-up [46]. A Chinese study revealed that more than one-third of existing psychiatric patients might fulfil the diagnostic criteria for PTSD, and more than one-quarter of psychiatric patients suffered from moderately severe to severe insomnia. Morillo- Gonzales et al. [47] have described the case of a psychotic patient whose delusional thought content was focused on COVID-19 and who subsequently developed behavioural disturbances that resulted in severe ocular damage [47].
Neurotoxic Effects
SARS-CoV-2 virus is a “neurotropic” virus because it can enter nerve cells. Neurotropic viruses include the mumps, rabies, and Epstein-Barr viruses. While some neurotropic viruses cause milder symptoms, others can cause swelling in the brain, paralysis, and death. SARS-CoV-2 is associated with several neurological symptoms and syndromes, including headache, fatigue, anosmia, ageusia, anorexia, myalgias, asthenia, meningitis, encephalitis, Guillain-Barré Syndrome, altered consciousness, syncope, and stroke [48-50]. Neurological effects of coronaviruses (including SARS-CoV-2) may be triggered by direct cytopathic effects of the virus, secondary effects of severe pulmonary infection, a cytokine storm, or a combination of these [51].
SARS-CoV-2 may cause neurological disorders by directly infecting the brain or as a result of the strong activation of the immune system. Recent studies have detected the novel coronavirus in the brains of fatal cases of Covid-19. It has also been suggested that infection of olfactory neurons in the nose may enable the virus to spread from the respiratory tract to the brain. Olfactory and gustatory dysfunctions are now recognized clinical symptoms, and these symptoms indicate the viral affinity of the nervous system. Two-thirds of patients were observed to initially suffer from olfactory and gustatory symptoms, and the fatigue experienced by most patients is suggestive of neurotoxicity [52]. Several neurological and neuroradiological phenotypes have already been reported and several laboratories have already studied SARS-CoV in a number of animal species, including primates, mice, rats, hamsters, and moss [53].
Once the virus enters the brain, further infection is almost inevitable-there are ACE2 (Angiotensin-converting enzyme 2) membrane receptors on the surface of the brain cells through which the virus easily penetrates the tissue, causing inflammation. These viruses have similar receptor sites that bind to angiotensin converting enzyme 2 (ACE2) (SARS-CoV-1 and SARS-CoV-2) and CD26 (MERS/SARS-CoV-2), respectively [54,55]. Both ischaemic and haemorrhagic strokes have been reported in COVID-19 cases. In milder cases, encephalitis can cause flu-like symptoms; in more severe cases, it might bring seizures, paralysis, and confusion. Almost a third of SARS and MERS patients hospitalized experienced confusion while treated in the hospital [2]. Early evidence from the COVID-19 pandemic suggests that delirium could be a similar common problem. The impacts of COVID-19 on the brain and the effects of potentially altered brain function on mental health issues are both unclear.
SARS is known to be clinically neurotoxic, causing mental health and neurological disorders including neuromuscular and joint findings [41]. COVID-19 has also been linked with encephalitis [56] and Guillain-Barré syndrome [57-59], where the immune system attacks the nerves-an overreaction of the immune cells in an attempt to thwart the viral pathogen. This is akin to a cytokine storm. It is unclear if the encephalitis encountered in COVID-19 is due to a direct invasion of the virus into the nervous system or the destruction is due to the overactivity of the immune system. Again, the mechanisms of Guillain-Barré appear to be associated with the normally protective antibodies of immune system, which are also thought to occasionally go ‘haywire’ by attacking the nerves and their coating.
COVID-19 needs to be further explored due to the possibility of it causing immune-mediated neurotoxic effects on the brain-just like SARS. From 1918 to 1919, a Spanish flu pandemic emerged, which was traced to a spike in Parkinson’s disease after the virus caused degeneration of nerve cells. Hearing loss has been reported in several cases of recovered COVID-19 patients. Even in asymptomatic cases, COVID-19 infection could have deleterious effects on cochlear hair cell functions [60]. Typically, virus-induced hearing loss is sensorineural, although conductive and mixed hearing losses can be seen following infection with certain viruses. Cytokine storm, an autoimmune reaction occurring at the height of the infection in some individuals is thought to be mainly responsible for the complications of COVID-19 [61-63]. Butler et al. [64] have summarised the neuropsychiatric complications of COVID-19 and suggested that the biological mechanism including autoimmunity could enlighten the aetiological research of psychotic disorders [64].
Tiredness or fatigue has become a recognized symptom among patients infected with COVID-19, reportedly affecting between 44% and 69% of individuals [65]. The study of Townsend et al. [65] concluded that COVID-19 creates a huge burden of fatigue which is likely to impair quality of life necessitating management strategies for convalescing patients [65]. Reports suggest that some of the recovered patients may continue to experience fatigue after several months of recovery. Autoreactive antibodies are thought to be responsible for “long Covid” symptoms that linger months after the apparent recovery from the viral infection. In similar ways, an autoimmune-like reaction and autoreactive antibodies could be postulated as aetiological mechanism of a subset of schizophrenia and COVID-19 could generate an interest in immunopsychiatry. A recent analysis of over a quarter of a million patients has shown that six months after infection with COVID-19, there is a substantial neurological and psychiatric morbidity [66]. While the pandemic is going on, the time is ripe for the development of an immunitybased psychiatry. This fledgling field of immunopsychiatry has great potential in the aetiological research of psychotic disorders for finding new treatment strategies. Psychotic symptoms are conjectured to be the outcome of autoimmune antibodies against the brain and later shaped by neurological and psychosocial factors [67].
Psychosocial Impact
Pandemics extend beyond pathophysiology and medical phenomena to associations with intense psychosocial impact. The interruption in the school system of the youngsters has befuddled them, while senior residents have to isolate themselves, the cares and individuals recuperating from the disease and those with long term clinical conditions will all face their own psychological issues. As far as securing psychological wellness, the significance of remaining connected with friends and family, working out, and keeping busy are useful adapting procedures. Long-term behavioural changes like vigilant handwashing and avoidance of crowds as well as a delayed return to normality even after many months after the quarantine due to SARS had been reported [68]. The same scenario could be repeated in post COVID period. Thus, the quarantine period seems to have important and dysfunctional psychological consequences on the individual’s mental health not only in the short-term but even in the long-term period [69].
Hopefully, the mass disasters can bring about unity in order to curb the situation, and that will improve mental health. Individual mental wellbeing can be assisted by the ‘big group energy effect.’ In health crisis, social environment is an important factor to consider in order to maintain mental health, yet it is under consistent threat. Feelings of insecurity creeps in when we lose control of our environment, and there is anxiety as a result of the obscure end of the existence of the current medical crisis. Psycho-spiritual preparedness is important at this stage to face the pandemic challenges. For effective combat with present and future pandemics, psychiatric and psychological aspects of COVID-19 from the perspectives of public and global mental health have to be studied [70].
India is currently in the grip of a monstrous second wave of the pandemic and the psychological casualties could be beyond anybody’s imagination. India has a population of 1.3 billion and it is experiencing the worst outbreak the world has seen. In an average day, over 300,000 cases have been documented and the estimated total number of deaths has recorded up to 200,000 as of May 6th,2021. When Covid cases receded in September,2020, there was a relaxed attitude and a sense of triumph in the name of herd immunity. Consequently, mass gatherings such as political rallies and religious events were allowed to take place. New variants of the coronavirus emerged, and all these factors have partly led the surge. The possibility of a third wave cannot be ruled out. The compound family system of India acts as a buffer to deal with many collective sufferings, but the current crisis could bust such psychosocial coping mechanisms. While developed countries appear to have made a truce with the viral conqueror through vaccinations, developing countries are still highly vulnerable to the viral assaults.
Conclusion
Studies have now clearly established that people with existing mental disorders are prone to relapses compounded with the fear of social isolation, fear of death, consequences of the obliged quarantine, fear of the infection, or a complicated grief for the unexpected loss of beloved people and stress of coping with COVID-19 prevention measures. Anxiety symptomatology, aggravation of OCD symptoms, depression and suicidal thoughts during the pandemic have been documented in most studies. There is an overall increase of alcohol and substance abuse. Reactive psychiatric symptoms have been widely described as secondary effects of the pandemic. Certain groups of people have been identified as particularly vulnerable to the onslaught of the viral pandemic. Geriatric population have been undoubtedly victimised by this pandemic. Even though richer countries have been successful in controlling the epidemic through effective vaccination programmes to some extent, poor countries are still struggling with the assaults of the viral invader and it would be a long way for these countries to gain the benefits of preventive vaccinations.
A body-mind-spirit approach may be desirable to deal with the physical and psychological aftermath of COVID-19. There is an agreement in all the relevant studies that health care professionals are at an increased risk of getting infected with the virus, high levels of stress, anxiety, depression, burnout, addiction, and PTSD, which could have long-term professional and psychological consequences. The last few months have witnessed unprecedented cases of bereavement. People should find time in comforting and uplifting others through phone calls, texts, emails and skype interviews. It is as though people have to give grief permission to loosen its grip on themselves with the help of social connections. A scientific monitoring of the ongoing pandemic is highly significant for mental health professionals. They will have to collaborate with the colleagues from other medical specialities and with lived experiences of COVID to improve the prospects for well-being of the society. Knowledge generated during the pandemic may inform future intervention studies as well as mental healthcare policies. The pandemic has spawned an urgent need for integrating technology into innovative models of mental healthcare. The practical constraints in the management of psychiatric patients due to the ongoing pandemic have required the promotion of telepsychiatry, but overuse of digital mental health services has its own pitfalls that need to be identified further. While using modern technology to provide psychiatric service, the human aspects should be given due considerations. Psychiatrists may have a modified role in the digital and AI (artificial intelligence) post COVID era.
Cytokine storm in severe cases of COVID-19 leading to complications including neurotoxic effects also illustrate how an abnormal autoimmune reaction could lead to the formation of psychotic symptoms and strengthen the autoimmune etiology of psychotic disorders. These observations may pave the path to the establishment of immunopsychiatry and immuno-neuropsychiatry. Such endeavours would promote investigating how the immuneinflammatory response translates into psychiatric illness shedding more light into the study of the etiopathogenesis of these disorders.
Limitations
1. It may be too early to make any firm conclusions about the different epidemiological and clinical aspects of a new viral infection as well as the concomitant psychological impacts.
2. The research studies have been hasty because scientific community was unprepared for a pandemic. Most of the studies have been observational rather than interventional.
3. The pathogenesis of COVID-19 has not been completely mapped out-the neurotoxic effects are only evolving.
4. The cross-sectional nature of many of the reported studies does not allow interpretation for causality.
5. Most studies are single-centre study without a control group of patients, lack of information on symptom history before COVID-19 illness and the lack of details on symptom severity.
6. The initial studies consisted of small sample of patients and that limited the interpretability. Follow up studies are restricted because of the shorter time period.
7. COVID-19 is now a global pandemic, but the differences between countries may limit generalizability; psychiatric symptoms are culture bound.
Recommendations
1. More multicultural studies are vital while studies are mostly limited to European countries and China, yet the pandemic has become global.
2. More international research collaboration is warranted.
3. The complications of cytokine storm, an autoimmune reaction could give a new impetus for the autoimmune aetiological search for psychotic disorders. The neurotoxic effects of the COVID-19 might offer new conceptual models in cognitive sciences with regard to the causation of neurological and psychiatric disorders.
4. The lessons learnt from the ongoing pandemic should be rerouted to the prevention of major medical crisis, chemical warfare, and nuclear disasters of the future years.
5. Health professionals and the general public should become more cognizant of balancing immunity.
References
- Holmes EA, Connor RC, Perry VH, Tracey I, Wessely S, et al. (2020) Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7(6): 547-560.
- Jonathan PR, Edward C, Oliver D, Pollak TA, McGuire P, et al. (2020) Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7(7): 611-627.
- Vindegaard N, Eriksen Benros M (2020) COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 89: 531-542.
- Kotfis K, Roberson SW, Wilson JE, Dabrowski W, Pun BT, et al. (2020) COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit Care 24(1): 176.
- Mazza MG, Lorenzo R, Conte C, Poletti S, Vai B, et al. (2020) Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun 89: 594-600.
- Cudjoe TK, Kotwal AA (2020) Social distancing” amidst a crisis in social isolation and loneliness. J Am Geriatr Soc 68(6): E27-E29.
- Steinman MA, Perry L, Perissinotto CM (2020) Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Intern Med 180(6): 819-820.
- Gorenko JA, Moran C, Flynn M, Dobson K, Konnert C (2021) Social isolation and psychological distress among older adults related to covid-19: a narrative review of remotely delivered interventions and recommendations. J Appl Gerontol 40(1): 3-13.
- Rallwage M, Loosen A, Hauser TU, Moran R, Raymond JD, et al. (2020) Confidence drives a neural confirmation bias. Nature Communications 11(1): 2634.
- Philip PP (2020) COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry 52: 102066.
- Yang Y, Li W, Zhang Q, Zhang L, Cheung T, et al. (2020) Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 7 (4): e19.
- Tsai J, Wilson M (2020) COVID-19: a potential public health problem for homeless populations. Lancet Public Health 5(4): e186-e187.
- Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ (2020) The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry 7(4): e20.
- Yao H, Chen JH, Xu YF (2020) Rethinking online mental health services in China during the COVID-19 epidemic. Asian J Psychiatr 50: 102015.
- Hu Y, Chen L, Ji H, Xi M, Fang Y, et al. (2020) The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci Bull 36(3): 299-302.
- Fakari FR, Simbar M (2020) Coronavirus pandemic and worries during pregnancy, a letter to the editor. Arch Acad Emerg Med 8(1): e21.
- Zhai Y, Du X (2020) Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry 7(4): e22.
- Yen MY, Schwartz J, King CC, Lee CM, Hsueh PR (2020) Recommendations for protecting against and mitigating the COVID-19 pandemic in long-term care facilities. J Microbiol Immunol Infect 53(3): 447-453.
- Lebrasseur A, Bédard NF, Lettre J, Raymond E, Bussières EL, et al. (2021) Impact of the COVID-19 pandemic on older adults: Rapid review. JMIR Aging 4(2): e26474.
- Freeman D, Garety PA, Bebbington PE, Smith B, Rollinson R, et al. (2005) Psychological investigation of the structure of paranoia in a non-clinical population. Br J Psychiatry 186: 427-435.
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, et al. (2020) Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 3(9): e2019686.
- Sasha R, Talia S, Neal K, Catherine KE, Hernandez M, et al. (2020) Depression and anxiety during the covid‐19 pandemic in an Urban, low‐income public university sample. Journal of Traumatic Stress 34(1): 12-22.
- Abhinav V, Saleem A, Dian D, Qasim A (2020) COVID-19 diagnostic difficulties and acute psychosis. BJMP 13(1): a002.
- Susana M, Espada CSM, Pérez J, Antonio Z, Alberto B, et al. (2020) Case with psychotic disorder as a clinical presentation of COVID‐19. Psychiatry and Clinical Neurosciences 74(10): 551-552.
- Roesch E, Amin A, Gupta J, Garcia C (2020) Violence against women during covid-19 pandemic restrictions. BMJ 369: m1712.
- Debanjan B, Mayank R (2020) Social isolation in Covid-19: The impact of loneliness. International Journal of Social Psychiatry 66(6): 525-527.
- Feinberg ME, Mogle JA, Lee JK, Tornello SL, Hostetler ML, et al. (2021) Impact of the COVID-19 pandemic on parent, child and family functioning. Fam Progress.
- Wanjie T, Tao HB, Hu C, Jin G, Wang C, et al. (2020) Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders 274: 1-7.
- Wang QQ, Kaelber DC, Xu R, Volkow ND (2020) COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry 26(1): 30-39.
- Greenberg N, Docherty M, Gnanapragasam S, Wessely S (2020) Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368: m1211.
- Chiappini S, Guirguis A, John A, Corkery JM, Schifano F (2020) COVID-19: The hidden impact on mental health and drug addiction. Front Psychiatry 11: 767.
- Sher Leo (2020) The impact of the COVID-19 pandemic on suicide rates. QJM 113(10): 707-712.
- Kawohl W, Nordt C (2020) COVID-19, unemployment, and suicide. Lancet Psychiatry 7(5): 389-390.
- Abramowitz JS, McKay D, Storch EA (2017) The Wiley handbook of obsessive-compulsive disorders. John Wiley & Sons, Chichester, USA.
- French I, Lyne J (2020) Acute exacerbation of OCD symptoms precipitated by media reports of COVID-19. Ir J Psychol Med 37(4):291-294.
- Benatti B, Albert U, Maina G, Fiorillo A, Celebre L, et al. (2020) What happened to patients with obsessive compulsive disorder during the covid-19 pandemic? A multicentre report from tertiary clinics in Northern Italy. Front Psychiatry 11: 720.
- Sulaimani MF, Bagadood NH (2020) Implication of coronavirus pandemic on obsessive-compulsive-disorder symptoms. Rev Environ Health 36(1): 1-8.
- Aardema F (2020) COVID-19, obsessive-compulsive disorder and invisible life forms that threaten the self. J Obsessive Compuls Relat Disord 26: 100558.
- Nera H, Mevludin H, Izet P (2020) COVID-19 affected mental health of at-risk groups of psychiatric patients: two case reports. Psychiatria Danubina 32(2): 294-299.
- Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FHP, et al. (2020) The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res 289: 113096.
- MClay J, Parker M (2020) Alcohol use and misuse during COVID-19 pandemic: a potential public health crisis? Lancet Public Health 5(5): e259.
- Beale D (2020) Bright idea. RCPsych Insight 13: 20.
- Strang P, Bergström J, Martinsson L, Lundström S (2020) Dying from covid-19: loneliness, end-of-life discussions, and support for patients and their families in nursing homes and hospitals. A national register study. J Pain Symptom Manage 60(4): e2-e13.
- Mahony SO (2020) Mourning our dead in the covid-19 pandemic. BMJ 369: m1649.
- Mathew H, Bullimore ED, Rory CO, Holmes EA (2020) The scope of mental health research during the COVID-19 pandemic and its aftermath. British Journal of Psych 217(4): 540-542.
- González-Blanco L, Santo FD, Álvarez LG, Tomás LF, Lacasa CM, et al. (2020) COVID-19 lockdown in people with severe mental disorders in Spain: Do they have a specific psychological reaction compared with other mental disorders and healthy controls? Schizophr Res 223: 192-198.
- Morillo-González J, Huerta DH, Henríquez AG, Palacio AC, Nogueira PP (2020) Beyond the respiratory system: a case report highlighting the impact of covid-19 in mental illness and its physical consequences. The Journal of Clinical Psychiatry 81(4).
- Koralnik IJ, Tyler KL (2020) COVID-19: A global threat to the nervous system. Ann Neurol 88(1): 1-11.
- Román GC, Spencer PS, Reis J, Buguet A, Faris MEA, et al. (2020) The neurology of COVID-19 revisited: A proposal from the environmental neurology specialty group of the world federation of neurology to implement international neurological registries. J Neurol Sci 414: 116884.
- Anna SN, Kiran TF, Willey JZ, Thakur KT, Boehme AK (2020) Potential neurological manifestations of COVID-19. Neurol Clin Pract 11(2): e135-e146.
- Lechien JR, Estomba CM, Siati DR, Horoi M, Bon SD, et al. (2020) Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicentre European study. Eur Arch Otorhinolaryngology 277(8): 2251-2261.
- Callaway E (2020) Lab’s rush to study coronavirus in transgenic animals-some are in short supply. Nature 579(7798): 183.
- Khan S, Siddique R, Shereen MA, Ali A, Liu J, et al. (2020) The emergence of a novel coronavirus (SARSCoV-2), their biology and therapeutic options. J Clin Microbiol 58: e01297-e01320.
- Vankadari N, Wilce JA (2020) Emerging WuHan (COVID-19) coronavirus: glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26. Emerg Microbes Infect 9(1): 601-604.
- Stainsby B, Howitt S, Porr J (2011) Neuromusculoskeletal disorders following SARS: a case series. J Can Chiropr Assoc 55(1): 32‐39.
- Garg RK, Paliwal VK, Gupta A (2020) Encephalopathy in patients with COVID-19: A review. J Med Virol 93(1): 149-150.
- Scheidl E, Canseco DD, Naumov AH, Bereznai B (2020) Guillain-Barré syndrome during SARS-CoV-2 pandemic: A case report and review of recent literature. J Peripher Nerv Syst 25(2): 204-207.
- Fokke C, Berg B, Drenthen J, Walgaard C, Doorn PA, et al. (2014) Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain 137(Pt 1): 33-43.
- Zhao H, Shen D, Zhou H, Liu J, Chen S (2020) Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 19(5): 383-384.
- Mustafa MWM (2020) Audiological profile of asymptomatic Covid-19 PCR-positive cases. Am J Otolaryngol 41(3): 1024833.
- Azkur AK, Akdis M, Azkur D, Sokolowska M, Veen W, et al. (2020) Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy 75(7): 1564-1581.
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, et al. (2020) COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet 395(10229): 1033‐1034.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497‐506.
- Mathew B, Thomas AP, Alsadair GR, Benedict DM, Timothy RN (2020) Neuropsychiatric complications of Covid-19. BMJ 371: m3871.
- Townsend L, Dyer AH, Jones K, Dunne J, Mooney A, et al. (2020) Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE, p. e0240784.
- Taquet M, John G, Masud H, Paul H (2021) Six-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8(5): 416-427.
- Pandarakalam JP (2020) Neuropsychiatric complications of COVID-19. BMJ 371: m3871.
- Cava MA, Fay KE, Beanlands HJ, McCay EA, Wignall R (2005) The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs 22(5): 398-406.
- Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, et al. (2020) The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine 113(8): 531-537.
- Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I (2020) COVID-19 pandemic and public and global mental health from the perspective of global health security. Psychiatr Danub 32(1): 6-14.
© 2021 James Paul Pandarakalam. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






