- Submissions

Full Text
Gerontology & Geriatrics Studies
Incidence and Clinical Outline of Medical Comorbidities Among Old Schizophrenic Patients: An Initial Local Review
Saeed Shoja Shafti*, Alireza Memarie, Masomeh Rezaie and Behjat Rahimi
Professor of Psychiatry, University of Social Welfare and Rehabilitation Sciences, Razi Psychiatric Hospital, Tehran, Iran
*Corresponding author: Saeed Shoja Shafti, Professor of Psychiatry, University of Social Welfare and Rehabilitation Sciences, Razi Psychiatric Hospital, Tehran, Iran
Submission: March 18, 2020;Published: April 30, 2020

ISSN 2578-0093Volume5 Issue5
Abstract
Introduction: Comorbidity between mental disorders and physical illnesses is the rule rather than the exception. Approaches to study the impact of comorbidity become challenging also due to lack of consensus about how to define and measure the concept of comorbidity. The aim of the present study was to evaluate the clinical profile of medical comorbidity among a group of local chronic elderly schizophrenic patients to see their prevalence and physiognomies.
Methods: while the geriatric section of Razi psychiatric hospital had been selected as the field of investigation, all elderly schizophrenic patients, who have been hospitalized there for lifelong, had been selected as accessible sample and surveyed with respect to recorded checkups and comorbid medical diagnoses. Psychiatric diagnosis was in essence based on ‘Diagnostic and Statistical Manual of Mental Disorders’, 5th edition (DSM-5) and medical diagnosis was principally based on ‘International Classification of Diseases’, 10th
Results: Assessment had been performed on 168 aged schizophrenic patients (≥65 years old), including 101 men and 67 women. According to the results, 89% (n=151) of the elderly patients had some kind of registered non-psychiatric co-morbidity, which was meaningful higher than the frequency of comorbidity among a senior group of local residents. Amongst recorded co-morbidities: falls, hypertension and osteoarthritis were the most prevalent comorbidities with a frequency around 48.8%, 44.6% and 39.2%, respectively. Hypertension, renal disease and malnutrition were significantly more prevalent among male patients (p<0.0000, p<0.0045 and p< 0.0018, in turn) and hyponatremia, aspiration/asphyxiation and seizure were meaningfully more prevalent among female patients (p<0.0075, p<0.0000 and p<0.0009, one-to-one). As stated by the findings and in comparison, with the senior group of local people, while diabetes, renal diseases and malnutrition were significantly more frequent, coronary artery disease, gastrointestinal disorder and osteoarthritis were significantly less frequent among the present sample of elderly schizophrenic patients.
Conclusion: While in comparison with a senior group of local people, the rate of medical co-morbidities, particularly diabetes, renal diseases and malnutrition, were significantly higher in chronic elderly schizophrenic patients, a significant difference; as well, was the interrelated items between male and female patients, which demands further methodical and gender-based studies to define proper care and interventions for this vulnerable group of patients.
Keywords: Schizophrenia; Psychiatric disorders; Medical comorbidity; Elderly mental patients; Senior group of people; Chronic patients.
Introduction
Perhaps, comorbidity between mental disorders and physical sicknesses is the rule rather than the exception [1]. It is estimated that although 25% of the adult population have mental health illness, 68% of them suffer from comorbid medical disease [2]. While readmission rates in psychiatric patients are high and we still lack the understanding its likely predictors, physical co-morbidity could be one of important risk factors for psychiatric readmission [2]. On the other hand, while the term ‘comorbidity’ is well-acknowledged in research and clinical settings, the idea remains complicated and methodological approaches are different [3]. So, there is now no agreement about the definition of comorbidity, which can be defined in several different methods [3]. In general, the term comorbidity has three meanings:
- Indicating a medical sickness in a patient existing concurrently but independently with another condition.
- Representing a medical disease in a patient that causes, is caused by, or is otherwise related to another ailment in the same patient.
- Indicative of two or more medical sicknesses in a patient that exist at the same time,
regardless of their causative association [4]. In an inclusive trial of integrating different aspects of comorbidity, authors have combined different constructs and measures associated with the core concept of comorbidity. Hence, in this respect, four major distinctions were made according to the nature of the health condition, the relative importance of the co-occurring conditions, and the chronology of the conditions: comorbidity, multimorbidity, morbidity burden and patient’s complexity [5,6]. On the other hand, there is growing interest among physicians and scholars in the impact of comorbidity on a range of outcomes, such as mortality, health-related quality of life, patient's functioning, and health care utilization [7]. For instance, physical comorbidities, basic demographic data, and clinical variables have shown to much better foretell mortality than the risk of readmission [8]. Also, in patients with comorbidities, along with the higher risk of dying, a poorer functional status, quality of life, and a greater use of health services has been recounted [8]. These conclusions led to the inference that among patients with comorbidity, the focus of health care should not only be on one particular ailment, but, besides, on the pathology in other organs and on indicators for quality of care, such as complications of management, readmissions, treatment plans and compliance to generally accepted clinical recommendations [9,10]. Earlier studies on patients with serious mental ailment such as long-lasting schizophrenia, bipolar disorder, or protracted recurrent depression, have revealed that these patients have higher mortality rates than persons without serious mental disorder [11]. This variance is partially explained as being produced by increases in comorbid medical disorders in the mentally ill, frequently chronic diseases such as diabetes [12] and cardiovascular disease [13]. Alternatively, though there is an assumption that patients with serious mental sickness experience a shortened life expectancy due to increased mortality and few of these patients would survive until old age [14], there is now evidence that the numbers of these old mentally ill survivors is increasing [15,16]. As stated by a study, patients with serious mental disorder had significantly higher rates of medical emergency room visits and meaningfully longer lengths of medical hospitalizations than did the primary care control group [17], and for depressed aged persons with at least one chronic medical ailment, improvements in clinical management and harmonization of medical and mental health amenities could moderate the rate of utilization of services [18]. Furthermore, as said by another study on senior persons, readmission was most likely among persons with a primary diagnosis of schizophrenia, followed by bipolar disorder, depression, and substance abuse [19]. Likewise, comorbid severe mental illness in patients with diabetes is individually linked with greater risk of early medical or surgical re-hospitalization [20]. Besides, while health-risk behaviors (e.g., smoking, poor diet, and sedentary lifestyle) contribute to these poor outcomes, treatment with second generation antipsychotic drugs as well has been associated with poorer glycemic control among patients with diabetes [21]. Alternatively, patients with serious mental conditions appear to under-utilize primary care services [22] and consequently increase the risk of medical hospitalizations due to possibly avoidable complications [23]. Additionally, these patients may be at heightened risk of in-hospital adverse events, too, such as nosocomial infections and postoperative complications [24]. Nevertheless, another study had found no increased risk due to these comorbidities [25]. The aim of the present evaluation was to appraise the prevalence and physiognomies of medical comorbidities among a group of native elderly schizophrenic patients.
Methods
Razi psychiatric hospital in south of capital city of Tehran, as one of the largest and oldest public psychiatric hospitals in the Middle East, which has been established formally in 1917 and with a capacity around 1375 active beds, had been selected as the field of study in the present retrospective assessment. So, amongst its separate existent sections, chronic geriatric section of hospital with a capacity around 220 beds (110 for male and female aged patients, separately) had been designated as the specific field of investigation. Thus, for assessment, all chronic elderly schizophrenic patients (≥65 years old), as accessible sample, had been nominated and estimated with respect to registered checkups and comorbid medical conditions. Psychiatric diagnosis was principally based on ‘Diagnostic and Statistical Manual of Mental Disorders’, 5th edition (DSM-5) [26] and medical diagnosis was principally based on ‘International Statistical Classification of Diseases and Related Health Problems’, 10th Revision [27].
Statistical analysis
Descriptive statistics including means, standard deviations, and ranges for continuous variables and quantity or percent in each category for categorical variables were calculated for all characteristics. T-tests for continuous data and chi-square tests for categorical data were used to compare the necessary variables between genders or groups. Statistical significance, as well, had been defined as p value ≤0.05. MedCalc Statistical Software version 15.2 was used as statistical software tool for analysis.
Results
According to the findings, the current assessment of elderly schizophrenic patients had been performed on one hundred and sixty-eight patients, including one hundred and one males and sixtyseven females, who had been hospitalized in the chronic section of the hospital for long-life. Mean age (±SD) of the patients were around 69.12±8.93 and 74.69±6.54 for male and female patients, respectively, which was significantly shorter for male patients [t=-4.383, p<0.00, CI 95% =-8.08,-3.06]. As said by results, nearly 89% (n=151) of aged patients had some kind of registered nonpsychiatric co-morbidity, usually between one to four problems, that required specific care by a primary care physician or specialist, and so had received related standard cares, visits and treatments, on a regular basis (Table 1).
Table 1: Prevalence of medical co-morbidities among elderly schizophrenic patients.
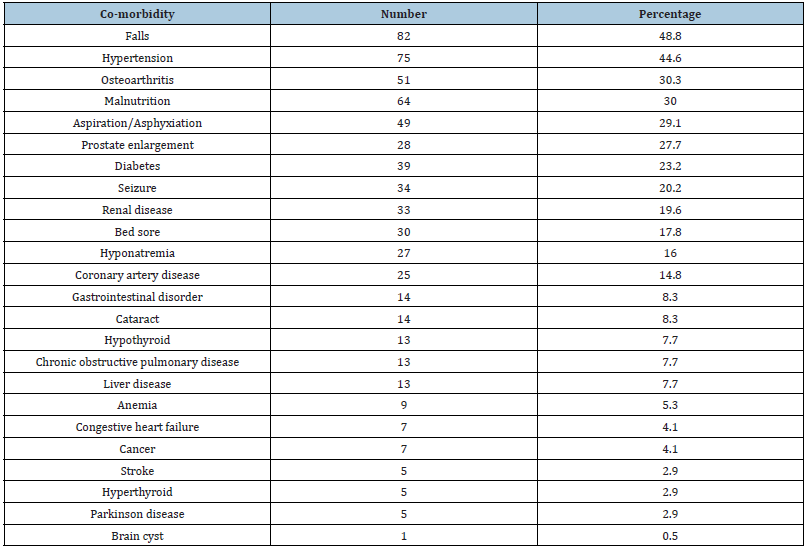
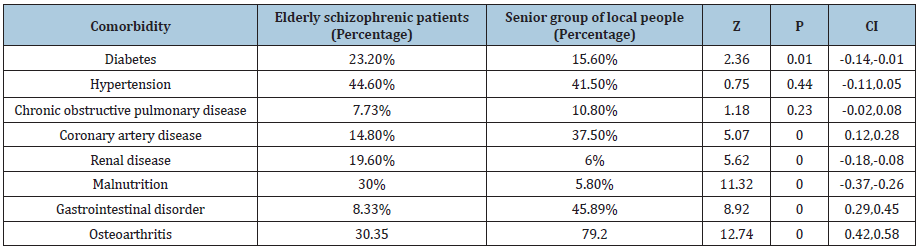
This amount of medical comorbidity was significantly higher in comparison with the local aged group of people with about 80% comorbidity (z= -3.2458, p<0.0012, CI 95%=-0.1761, -0.0435) [28]; (Table 2). Listed co-morbidities included diabetes, hypertension, falls, congestive heart failure, chronic obstructive pulmonary disease, osteoarthritis, cancer, coronary artery disease, liver disease, renal disease, stroke, thyroid disease, bed sore, aspiration/asphyxiation, seizure, hyponatremia, malnutrition, anemia, gastrointestinal bleeding, prostate enlargement, cataract, Parkinson disease and brain cyst (Table 1). Among them falls, hypertension and osteoarthritis were the most prevalent disorders with a percentage around 48.8%, 44.6% and 30.35%, respectively (Table 1).
Table 2: Prevalence of medical co-morbidities among elderly schizophrenic patients.
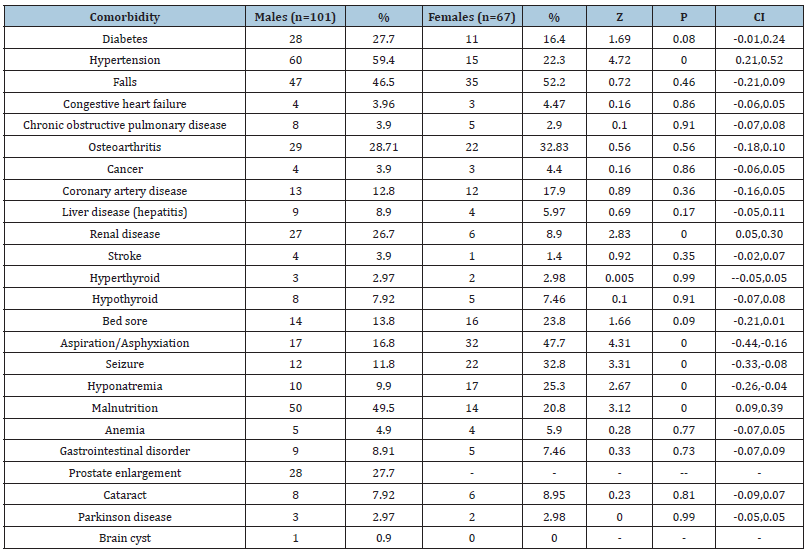
The next co-morbidities included malnutrition (30%), aspiration/asphyxiation (29.1%), prostate enlargement (27.7%), diabetes (23.2%), seizure (20.2%), renal disease (19.6%), bed sore (17.8%), hyponatremia (16%), coronary artery disease (14.8%), gastrointestinal disorder (8.33%), cataract (8.33%), liver disease (7.73%) and hypothyroidism (7.73%). The remaining comorbidities, including congestive heart failure, chronic obstructive pulmonary disease, cancer, stroke, anemia, Parkinson disease and brain cyst, were less than six percent, individually. As said by the findings, hypertension, renal disease and malnutrition were significantly more prevalent among male patients (p<0.0000, p<0.0045 and p< 0.0018, in turn) and hyponatremia, aspiration/ asphyxiation and seizure, were significantly more prevalent among female patients (p<0.0075, p<0.0000 and p<0.0009, one-to-one) (Table 3).
According to the findings and in comparison with the senior people of local people, while diabetes, renal diseases and malnutrition were significantly more frequent, coronary artery disease, gastrointestinal disorder and osteoarthritis were significantly less frequent among the present sample of chronic old schizophrenic patients (Table 3).
Table 3: Prevalence of medical co-morbidities among male and female elderly schizophrenics.
Discussion
While the co-occurrence of mental and physical conditions is very common in clinical settings, the exact nature of relationship between them is very complex and hitherto not well understood [29]. So far, very little work has been done on medical comorbid disorders among patients with mental illnesses since comorbidity was rarely the main objective of studies [5]. Additionally, while comorbidity is generally associated with mortality, consequences of specific disease combinations depend on many issues [11]. It is clear that in elderly people, each body system undergoes changes, which occur over many years and are considered normal among senior people [10] However, these changes often place the elderly persons at high risk for the development of various diseases [15]. So, it is very important to differentiate normal from pathological alterations in order to prevent wrongly treatment of normal changes and failing to treat those that result from ailments [29].
Back to our discussion and with respect to clinical profile of medical comorbidity among senior schizophrenic patients, almost most of patients had some kind of registered non-psychiatric comorbidity that demanded specific attention by a primary care physician or specialist. Thus, in comparison with senior group of local people [28] a significantly higher proportion of comorbidity was evident among the present sample. Such a finding was in harmony with the outcomes of Brown et al. [12], Andrés et al. [5] and Vigod et al. [7] who believed that psychiatric patients have been widely reported to be at an increased risk of morbidity and mortality due to physical disorders and comorbidity between medical and mental disorders is the rule rather than the exception. But it was not in harmony with the conclusions of Daumit et al. [25], who had found no significant increased risk of morbidity or mortality associated with the presence of these comorbidities in severe mental patients.
Besides, among the listed comorbidities in current assessment, falls, hypertension and osteoarthritis were the most prevalent medical complications. These outcomes are partially consistent with the findings of Hendrie et al. [17], who had found hypertension, osteoarthritis and diabetes as the most prevalent medical comorbidities among aged mental patients. But in contrary to him, in the present assessment there was not any significant difference regarding prevalence of hypertension between the present sample of schizophrenics and senior group of local people. Besides, while his claim regarding higher prevalence of falls in comparison with the primary care controls was not approvable here, due to deficiency of reliable native recording, falls was meaningfully higher among our patients, in comparison with other recorded items. Anyhow, the impact of demographic variances should not be ignored, since his samples included more females, a variety of ethnic groups and outpatients from primary care clients, while our samples included more males, single ethnic group (Persians), and only inpatients. Also with respect to other major co-morbidities in the present assessment, like malnutrition, diabetes, seizure, renal disease, coronary artery disease, gastrointestinal disorder and hypothyroidism , our findings were to some extent in harmony with reports of Zubenko et al. [30], Zgueb et al. [31], Räsänen et al. [32], Gausset et al. [33], Lim et al. [34], Hewer et al. [35], Tabbane et al. [36], Abiodun et al. [37] and Kamara et al. [38], who had found, as a general rule, infections, lung, gastrointestinal, urogenital and cardiovascular diseases as the most prevalent medical comorbidities among severe mental patients; Because they were comparable only with respect to urogenital and cardiovascular diseases. Our results regarding the remaining rarer co-morbidities, like congestive heart failure, chronic obstructive pulmonary disease, cancer and stroke, again, were not coherent with the outcomes of Hendrie et al. [17] and Tabbane et al. [36]. Furthermore, since medical problems like, bed sore, aspiration/asphyxiation, seizure, hyponatremia and malnutrition, had not been pointed out or surveyed in the parallel studies, further assessment becomes difficult.
On the other hand, as said by the conclusions of the current evaluation, hypertension, renal disease and malnutrition were significantly more prevalent among male patients and hyponaremia, aspiration/asphyxiation and seizure, were meaningfully more prevalent among female patients, which may display a gender-based difference in this regard. While such a difference could depend partly on the route of care, and somewhat on biological grounds, it may perhaps offer facts for future studies, too. Likewise, in comparison with the local senior persons, diabetes, renal diseases and malnutrition were significantly more frequent among the present sample of chronic elderly schizophrenic patients, a finding which was again, unharmonious with the findings of Hendrie et al. [17]. Anyhow, while the impact of physical comorbidity on psychiatric readmission is still unsatisfactorily investigated problem, there is a growing interest among specialists and academics in the impact of physical comorbidity on a variety of outcomes in mental disorders, such as mortality, health-related quality of life and health care spending, which is noticeably higher for patients with comorbid disorders [10]. The comorbidity of mental and physical disorders is on the increase and as pointed out by Sartorius this topic is becoming a main challenge to medicine in the 21st Century [14].
Future research should address these topics with more indepth studies since new understandings in this field could lead to better prevention approaches to reduce psychiatric readmissions [15]. In this regard, teaching regarding the normal changes of aging should be the first intervention made with all aging adults to help them understand what is going on in their bodies. In addition, many interventions are available to compensate for these changes as well as to prevent the development of disease as a consequent of these interventions [29]. Short duration of assessment, small sample size, restriction of study to a single academic center and lack of parallel and concomitant control groups, were among the weaknesses of the present evaluation. Surely, further methodical research are needed to define proper care and interventions for this vulnerable group of patients.
Conclusion
While in comparison with senior group of local people the rate of medical co-morbidities, particularly diabetes, renal diseases and malnutrition, were significantly higher in chronic elderly schizophrenic patients, a significant difference, as well, was palpable regarding the interrelated items between male and female patients, which demands further methodical and gender-based studies to define proper care and interventions for this vulnerable group of patients.
References
- Šprah L, Zvezdana Dernovšek M, Wahlbeck K, Haaramo P (2017) Psychiatric readmissions and their association with physical comorbidity: A systematic literature review. BMC Psychiatry 17(1): 2.
- Cloninger RC (2002) Implications of comorbidity for the classification of mental disorders: the need for a psychobiology of coherence. In: Maj M, Gaebel W, et al. (Eds.), Psychiatric Diagnosis and Classification. West Sussex: Wiley, USA, pp. 79-106.
- AIHW (2007) Comorbidity of mental disorders and physical conditions, Cat. no. PHE 155. Canberra: AIHW, Australia.
- Egede LE (2007) Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry 29(5): 409-416.
- Andrés E, Campayo J, Magán P, Barredo E, Cordero A, et al. (2012) Psychiatric morbidity as a risk factor for hospital readmission for acute myocardial infarction: an 8-year follow-up study in Spain. Int J Psychiatry Med 44(1): 63-75.
- Jakovljević M, Ostojić L (2013) Comorbidity and multimorbidity in medicine today: Challenges and opportunities for bringing separated branches of medicine closer to each other. Psychiatr Danub 25(1): 18-28.
- Vigod SN, Taylor VH, Fung K, Kurdyak PA (2013) Within-hospital readmission: an indicator of readmission after discharge from psychiatric hospitalization. Can J Psychiatry 58(8): 476-481.
- Kessing LV, Nilsson FM, Siersma V, Andersen PK (2004) Increased risk of developing diabetes in depressive and bipolar disorders? J Psychiatr Res 38(4): 395-402.
- Howell NLM, Proctor EK, Blinne WR, Rubin EH, Saunders JA, et al. (2006) Post-acute dispositions of older adults hospitalized for depression. Aging & Mental Health 10(4): 352-361.
- Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1): 8-27.
- De Hert M, Cohen D, Bobes J, Bakmas M, Leucht S, et al. (2011) Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 10(2): 138-151.
- Brown S, Kim M, Mitchell C, Inskip H (2010) Twenty-five-year mortality of a community cohort with schizophrenia. Br J Psychiatry 196(2): 116-121.
- Laursen TM, Olsen T, Agerbo E, Gasse C, Mortensen PB (2009) Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch Gen Psychiatry 66: 713-720.
- Tosh G, Clifton A, Mala S, Bachner M (2010) Physical health care monitoring for people with serious mental illness. Cochrane Database Syst Rev CD008298.
- Harvey PD, Czaja SJ, Loewenstein DA (2012) Schizophrenia in later life. Am J Geriatr Psychiatry 20(1): 1-4.
- Dickens J, Boustani MA, Christopher CM, Purnell C, Munger S (2013) Comorbidity profile and health care utilization in elderly patients with Serious Mental Illnesses. Am J Geriatr Psychiatry 21(12): 1267-1276.
- Hendrie HC, Hay D, Lane KA, Gao S, Purnell C, et al. (2013) Comorbidity profile and health care utilization in elderly patients with serious mental illnesses. Am J Geriatr Psychiatry 21(12): 1267-1276.
- Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA (2004) Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care 42(6): 512-521.
- Prince JD, Akincigil A, Kalay E, Walkup JT, Hoover DR, et al. (2008) Psychiatric rehospitalization among elderly persons in the United States. Psychiatr Serv 59(9): 1038-1045.
- Chwastiak LA, Davydow DS, McKibbin CL, Schur E, Burley M, et al. (2014) The impact of serious mental illness on the risk of rehospitalization among patients with diabetes. Psychosomatics 55(2): 134-143.
- Bennett KJ, Probst JC, Vyavaharkar M, Glover S (2012) Missing the handoff: post-hospitalization follow- up care among rural Medicare beneficiaries with diabetes. Rural Remote Health 12: 2097.
- Garrison GM, Mansukhani MP, Bohn B (2013) Predictors of thirty-day readmission among hospitalized family medicine patients. J Am Board Fam Med 26(1): 71-77.
- King LC, Arnold D, Eubank KJ, Lo M, Yunyongying P, et al. (2013) Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med 28(2): 269-282.
- Himelhoch S, Leith J, Goldberg R, Kreyenbuhl J, Medoff D, et al. (2009) Care and management of cardiovascular risk factors among individuals with schizophrenia and type 2 diabetes who smoke. Gen Hosp Psychiatry 31(1): 30-32.
- Daumit GL, Pronovost PJ, Anthony CB, Guallar E, Steinwachs DM, et al. (2006) Adverse events during medical and surgical hospitalizations for persons with schizophrenia. Arch Gen Psychiatry 63(3): 267-272.
- American Psychiatric Association (APA) (2013) Diagnostic and statistical manual of mental disorders. In: (5th edn), American Psychiatric Association, Washington, USA.
- World Health Organization (2011) International statistical classification of diseases and related health problems, 10th World Health Organization, Geneva, Switzerland.
- Tootoonchi P (2004) Chronic diseases and senile changes in the elderly population. Payesh 3(3): 219-225.
- Wallace M (2008) Essentials of gerontological nursing. Springer Publishing Company, LLC, New York, USA, pp. 145-174.
- Zubenko GS, Mulsant BH, Sweet RA, Pasternak RE, Tu XM (1997) Mortality of elderly patients with psychiatric disorders. Am J Psychiatry 154(10): 1360-1368.
- Zgueb Y, Jomli R, Ouertani A, Hechmi S, Ouanes S, et al. (2014) Deaths in a Tunisian psychiatric hospital: an eleven-year retrospective study. Encephale 40(5): 416-422.
- Räsänen S, Hakko H, Viilo K, Meyer-Rochow VB, Moring J (2003) Excess mortality among long-stay psychiatric patients in Northern Finland. Soc Psychiatry Psychiatr Epidemiol 38(6): 297-304.
- Gausset MF, Casadebaig F, Guillaud-Bataille JM, Quemada N, Terra JL (1992) Mortality of mentally ill patients. Review of the literature. Encephale 18(1): 93-100.
- Lim LC, Sim LP, Chiam PC (1991) Mortality among psychiatric inpatients in Singapore. Singapore Med J 32(3): 130-132.
- Hewer W, Rössler W (1997) Mortality of patients with functional psychiatric illnesses during inpatient treatment. Fortschr Neurol Psychiatr 65(4): 171-181.
- Tabbane K, Joober R, Spadone C, Poirier MF, Olié JP (1993) Mortality and cause of death in schizophrenia. Review of the literature. Encephale 19(1): 23-28.
- Abiodun OA (1998) Mortality in a psychiatric population: a Nigerian psychiatric hospital experience. Acta Psychiatr Scand 77(6): 654-657.
- Kamara SG, Peterson PD, Dennis JL (1998) Prevalence of physical illness among psychiatric inpatients who die of natural causes. Psychiatr Serv 49(6): 788-793.
© 2020 Saeed Shoja Shafti. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






