- Submissions

Full Text
Gerontology & Geriatrics Studies
An Interprofessional Geriatric Team Meeting
Tamatha Arms1*, Noell Rowan2, Sara Miller3 and Lorie Sigmon4
1Associate Professor of UNCW School of Nursing, USA
2Professor, UNCW School of Social Work, USA
3Lecturer, UNCW School of Recreational Therapy, USA
4Assistant Professor, UNCW School of Nursing, USA
*Corresponding author: Tamatha Arms, Associate Professor of UNCW School of Nursing, USA
Submission: September 30, 2019;Published: October 16, 2019

ISSN 2578-0093Volume5 Issue2
Abstract
The purpose of this study was to determine if student participants in an interprofessional geriatric team meeting self-reported increased knowledge in interprofessional team collaboration competency. A faculty developed simulated scenario that included standardized patients and student volunteers from nursing, social work, and recreational therapy was live streamed to a large classroom where the remaining students watched. 191 students participated and all three disciplines showed significant improvement on the Interprofessional Collaborative Competency (ICCAS) attainment survey. This innovative way of delivering a simulated experienced allowed almost 200 students to have this experience simultaneously.
Keywords:Geriatric; Interprofessional; Team; Collaboration
Introduction
Interprofessional clinical education provides an opportunity for students to gain realworld knowledge and experience of working in collaborative teams while learning to adapt to the changing needs of patients [1]. Typically, these respective disciplines are taught in silos among universities across the nation and internationally. However, there has been a push for increased interprofessional education among health care disciplines. The increasing complexities of skills required by the health care environment, along with recent moves towards population-based care, has made interprofessional team collaboration essential to practice. Educational and curricula interventions will have to keep pace to ensure delivery of safe and efficient care. Simulation instruction has been endorsed by the World Health Organization (WHO) as an effective method of assisting health and social professionals to learn how to effectively work in teams [2]. This study used an innovative approach in using simulation that allowed over 100 students to participate at one time. The study had student participants from nursing, advanced practice nursing, social work, and recreational therapy as members of an interprofessional collaborative team. The purpose of this study was to determine if student participants in an interprofessional geriatric team meeting self-reported increased knowledge in interprofessional team collaboration competency.
Background/ Significance
The landmark Institute of Medicine report To Err Is Human (1999) found that potentially 98,000 preventable deaths occurred in the United States annually due to medical error (Higginson & Lake, 2017). One of the key recommendations from this report was the need “to establish interdisciplinary team training programs, such as simulation, that incorporate proven methods of team management.” (Higginson & Lake, 2017). The complexities of patients in current health care settings can no longer be treated by individual experts. Delivering care to a patient requires a complex network of professionals, who are are semiautonomous and interdependent (Grethlein & Azar, 2017). Currently, the care of patients is multifaceted and requires many expert contributors to be successful. Unless the members of health care delivery system can function and relate to each other as a functional team, a patient will receive suboptimal care (Grethlein & Azar, 2017). Patients in acute and sub-acute care settings are more complex and fragile than ever before. The U.S. and the world continue to see an ever-increasing older adult population which requires specialized geriatric team focused care. As we near 2020, this is the first time in history that older adults (age 65 and older) outnumber children below the age of five [3].
Typically, these respective professions are taught in isolation within universities and internationally. The growing amount of knowledge required for students to become expert in their chosen profession has increased the emphasis for improved interprofessional education among health and social care disciplines. Interprofessional education (IPE) transcends unit-professional and siloed approaches to health professions education [4]. Interprofessional education is defined by the World Health Organization as “when students from two or more professions learn about, from, and with each other to enable effective collaboration and improve health outcomes” [5]. Health and education systems consists of all organizations, people, and actions whose primary intent is to promote, restore, or maintain health and facilitate learning [5]. Education and health organizations must work together to direct workforce approaches that model the increasingly collaborative environment students will work in.
Methods
Faculty from the school of nursing, social work, and recreational therapy came together during a workshop on use of interprofessional simulation activities. These faculty members co-created a simulated scenario based on the Interprofessional Education Competencies [6]. Two volunteers standardized patient’s role played a married heterosexual couple, and a volunteer undergraduate social work student enacted the role of their adoptive daughter who is Korean. The “actors” were prepared ahead of time with the written simulation scenario and verbatim words to use. They were not given a script but asked to use a few verbatim statements in the scenario.
The simulated scenario portrays a farmer who is an older male that we will refer to as Mr. Jones. The farmer suffered a tractor accident while working that resulted in a below the knee leg amputation. The first responders noted alcohol on Mr. Jones’s breath and reported this to the ED personnel but, when asked, his wife denied him having “a drinking problem.” However, post-surgery, he develops delirium tremors (D.T.s) from alcohol withdrawal. Currently, his wife admits that he likes to drink “a few” beers every day but is not able to give a definitive amount. The wife makes several remarks and becomes adamant that “he is not an alcoholic!” The rest of his inpatient hospital stay was unremarkable. Mr. Jones is then transferred to an inpatient rehabilitation hospital setting, which is where the simulation takes place. The interprofessional geriatric team meeting surrounds his potential discharge from the rehabilitation hospital. The three faculty members created a complete profile and medical chart for Mr. Jones. He does not have any past medical conditions known and his wife states, “that’s because he never goes to the doctor!” Mr. Jones’s social history includes these aspects:
a) he was a combat war veteran in the Vietnam War and served two tours of duty,
b) he and his wife, married for 40 years, have one adult daughter who is adopted and a different ethnicity/race from themselves,
c) he has a high school diploma,
d) previous smoker but quit smoking 20 years ago. Medications that have been ordered for Mr. Jones while in rehabilitation are:
• aspirin 81mg daily,
• Neurontin 300mg three times daily and
• Elavil 25mg at bedtime.
Two student volunteers from each discipline of nursing, social work and recreational therapy, actively participate in the simulation. One nurse practitioner student is responsible for leading the team meeting. After an initial practice “run-through”, the actual simulated activity is live streamed by video into a large classroom where the remaining students are located. These students are in the same building and seated interprofessional to facilitate engagement with one another regarding roles and responsibilities of different disciplines. The students in the classroom have been given the scenario prior to the day of simulation and are also pre-briefed in the classroom. The pre-briefing focuses on the different roles and responsibilities of nursing, advanced nursing, social work and recreational therapy.
The actual simulated scenario has the volunteer students speaking with Mr. Jones and his wife individually, reporting off to each other and then coming together for a scheduled interprofessional team meeting. At this team meeting, the patient and his wife are present, but their adult daughter was unable to attend due to work obligations. As stated earlier, the nurse practitioner student’s role is to conduct the meeting. This student asks for a brief discipline specific report from the other students. Mr. Jones and his wife are then able to ask any questions they may have and voice concerns. The faculty member for each discipline has previously spoken to the respective students about the role and responsibility each have in this interprofessional team meeting. The nurse practitioner student summarizes all the reports and concerns and leads the development of a plan of care for discharge.
Students were expected to bring up several aspects of concern. For example, a social work student may offer counseling resources or connections to the nearest veterans of foreign wars (VFW). The nursing students go over multiple concerns including medication teaching. Recreational therapy students assist Mr. Jones in identifying enjoyable hobbies and adopting assistive devices so he can continue to participate in them. At the conclusion of the team meeting, Mr. Jones and his wife feel prepared for discharge and each discipline of students have a “to-do” list to accomplish this task. This entire scenario lasted approximately 30 minutes. After this, all the student volunteers and the standardized patients joined the classroom of students who watched the simulation via live stream. A debriefing process is then conducted by the three faculty members. All students are allowed and encouraged to ask questions. The Interprofessional Collaborative Competency (ICCAS) attainment survey was used as a pre/post tool to measure student’s self-reported competencies in the area of interprofessional collaboration. The ICCAS is a 20 question, seven point Likert type scale (1=strongly disagree, 2=moderately disagree, 3=slightly disagree, 4=neutral, 5=slightly agree, 6=moderately agree, and 7=strongly agree) with six subscales: communication, collaboration, roles and responsibilities, collaborative patient/family-centered approach, conflict management/resolution, and team functioning. Not applicable is also an option for every item on the scale. No items were reverse coded.
The ICCAS was validated in 1994 with a sample of 584 students (undergraduate and graduate) across 15 professions and clinicians attending professional development courses. Approximately 68% of the 250 participants who disclosed professions, identified themselves as healthcare providers. This scale was developed from the Interdisciplinary Education Perception Scale (IEPS), the Readiness for Interprofessional Learning Scale (RILS), and the Attitudes Toward Healthcare Teams Scale and reviewed by experts. Exploratory Factor Analysis (EFA) was conducted using Principal Axis Factoring (PAF) with oblique obliging rotation. The PAF was conducted on the pre and post scale separately to determine validity at separate times. Cronbach alpha was 0.961 and 0.941 respectively for Factor 1 and 2 loading in the pre assessment. The post assessment yielded a Cronbach alpha of 0.981 showing very good internal consistency [7]. Examples of survey questions are: use an interprofessional team approach with the patient to assess the health situation, include the patient and family in decisionmaking, develop an effective care plan with interprofessional team members, negotiate responsibilities within overlapping scopes of practice, and promote effective communication among members of an interprofessional team [8-10].
The core competencies for interprofessional collaborative practice consists of 38 items within 4 domains of values and ethics for interprofessional practice (VE), roles and responsibilities (RR), interprofessional communication (CC), and teams and teamwork (TT). Six of these competencies were chosen as student learning objectives for this interprofessional simulated activity. The two competencies within domain 1 (VE) were placing the interests of patients at the center and embracing the cultural diversity and individual differences that characterizes patients, and populations [11,12]. The two objectives from domain 2 (RR) were: communicate one’s roles and responsibilities clearly to patients, families, and other professionals, and explain the roles and responsibilities of other care providers and how the team works together to provide care. The last two objectives were from TT domain and state: engage other health professionals in shared patient-centered problem-solving, and reflect on individual and team performance for individual, as well as team performance [6].
Result
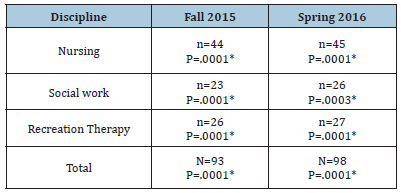
A total of 191 students participated in this simulated activity between two traditional university semesters see in Table 1. A total of 89 undergraduate pre-licensure nursing students, 49 undergraduate social work students and 51 undergraduate recreation therapy students participated. The one advanced practice nurse that participated did not complete the ICCAS survey. All 20 items on the ICCAS showed significant results from pre to post simulation in both semesters in all participants. Students were asked to write a reflective journal within 12 hours of attending the simulation. A couple of the qualitative remarks from the reflective process are:
Table 1:Demographics.
“I wish this would have been done for my family member last year when she was in the hospital…. this would have helped my family tremendously”
“The social workers explored what kind of support the parents needed from their daughter and ways that they could bond during the day without alcohol. The social workers educated the clients on how to access situation-appropriate resources and focused on client and family strengths. It was also helpful to see all the professions working on the behalf of the family.”
“It was nice to be able to watch the simulation through live stream because it allowed me to actually take in the bigger picture, I wasn’t worried or nervous like I usually get when I’m actually doing the simulation.”
Discussion/Clinical implications
Interprofessional education is essential in preparing nursing, social work, and recreation therapy students for the collaborative world of healthcare systems. The purpose of this study was to determine if student participants in an interprofessional geriatric team meeting self-reported increased knowledge in interprofessional team collaboration competency. The use of video live stream to a large classroom of students was a novel approach that allowed the scenario to unfold naturally. The simulation was not rushed as the faculty were not needing to get several students through the same simulation, as commonly occurs. The results of this study showed significant results in student’s self-reported knowledge and competency of interprofessional collaboration across all three disciplines. This simple faculty developed scenario is easily adaptable to meet objectives of various courses and programs. As our nation and world continues to age, similar experiential experiences will enhance student learning.
References
- Dow A, Thibault G (2017) Interprofessional education -- A foundation for a new approach to health care. N Engl J Med 377(9): 803-805.
- World Health Organization (2013) Transforming and scaling up health professionals’ education and training. World Health Organization Guidelines.
- Wan H, Goodkind D, Kowal P (2016) US Census Bureau. International Population Reports P95/16-1, An Aging World: 2015. US Government Publishing Office, Washington, USA.
- Rish EA, Kim S, Choe L, Varpio L, Malik E, et al. (2012) Current trends in interprofessional education of health sciences students: A literature review. Journal of Interprofessional Care 26(6): 444-451.
- World Health Organization (2010) A framework for action on interprofessional education and collaborative practice. World Health Organization, p. 64.
- IPEC (2011) Core competencies for interprofessional collaborative practice: Report of an expert panel. Interprofessional Education Collaborative, Washington, USA.
- Archibald D, Trumpower D, Donald C (2014) Validation of the interprofessional collaborative competency attainment survey (ICCAS). J Interprof Care 28(6): 553-558.
- Association of Rehabilitation Nurses (ARN) (2014) ARN competency model for professional rehabilitation nursing. Rehabilitation Nursing Journal.
- [CIHC] (2010) A national interprofessional competency framework. University of British Columbia, Vancouver, Canada.
- Family Caregiver Alliance (2015) Selected long-term care statistics.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, et al. (2010) Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 376(9756): 1923-1958.
- Skochelak SE, Hawkins RE (2017) AMA education consortium: Health systems science. Elsevier, St Louis, Missouri, USA.
© 2019 Tamatha Arms. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






