- Submissions

Full Text
Experimental Techniques in Urology & Nephrology
Salmonella Pyelonephritis and Renocutaneous Fistula in a Renal Transplant Recipient
Connor Eichenwald1, Rebecca N Kumar2 and Talal Al Qaoud3*
1 Internal Medicine & Pediatrics, Medstar Georgetown University Hospital, USA
2 Division of Infectious Diseases, Medstar Georgetown University Hospital, USA
3 MedStar Georgetown Transplant Institution, Medstar Georgetown University Hospital, USA
*Corresponding author: Talal Al-Qaoud, MedStar Georgetown Transplant Institution, Medstar Georgetown University Hospital, 2nd Floor PHC Building, 3800 Reservoir Road NW, Washington, DC 20007, USA
Submission: September 30, 2025;Published: October 13, 2025

ISSN 2578-0395Volume3 Issue3
Abstract
Non-Typhoidal Salmonella (NTS) infection typically causes gastroenteritis. Rarely, it can lead to focal or invasive infections including pyelonephritis. Transplant recipients are at increased risk of infection with typical and atypical organisms. We present a case of NTS pyelonephritis with renocutaneous fistula formation in a renal transplant recipient. This case presents important surgical issues and a rare potential focus of infection in transplant recipients.
Keywords: Non-typhoidal salmonella infection; Solid organ transplant; Immunosuppression; Renocutaneous fistula; Transplant pyelonephritis
Abbreviations: NTS: Non-Typhoidal Salmonella; INTS: Invasive Non-Typhoidal Salmonella; UTI: Urinary Tract Infection; MMF: Mycophenolate Mofetil
Introduction
Salmonella enterica, a species of non-lactose fermenting, motile, gram-negative rods, encompasses several thousand serovars which invade a host through the gastrointestinal system. Non-typhoidal Salmonella (NTS) most commonly causes gastroenteritis [1]. However, bacteremia or focal infections can occur with specific non-S. Typhi serovars and patient comorbidity combinations. Invasive NTS (iNTS) infections, or those associated with bacteremia, have been described in aneurysms and vascular grafts [2,3], as the etiology of septic arthritis or osteomyelitis (especially in persons with sickle cell disease), as seeding focal soft tissue and renal infections [4-7]. Focal infections comprise an estimated 7-12% of all NTS infections and are highly associated with immunosuppression and underlying anatomic abnormalities [2]. These focal manifestations have been rarely reported in the literature and there are few that specifically discuss Salmonella transplant pyelonephritis. We present a case with two concurrent focal NTS infections, pyelonephritis and renocutaneous fistula, in a renal transplant recipient.
Case Description
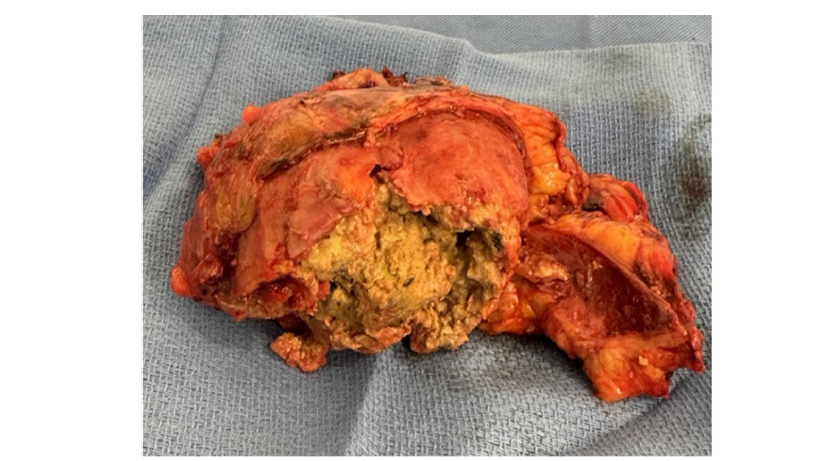
A 40-year-old female with two prior renal transplants presented for a second surgical opinion on a fistula from her failed renal transplant. A native of Liberia, she had moved to the US in 2001. Her end stage renal disease was secondary to longstanding hypertension and her medical history was notable for hyperlipidemia and chronic Hepatitis B infection. Her first renal transplant (right sided) was performed in 2004. This was complicated by rejection leading to graft failure and hemodialysis dependence from 2010 until 2023. In September 2023, she received a second deceased donor kidney transplant (left sided) without complications and with sustained excellent function on an immunosuppression regimen of Tacrolimus, Mycophenolate Mofetil and Prednisone. In December 2024, she developed a draining renocutaneous fistula with infection of her nonfunctioning (right sided) graft. Cultures performed from this drainage grew Salmonella enterica. Initial treatment was with Doxycycline and an attempt at graft nephrectomy that was aborted intra-operatively due to dense adhesions. By May of 2025, she was transitioned to Amoxicillin due to increased drainage despite ongoing suppressive therapy with Doxycycline. Repeat CT imaging performed at our center in June 2025 showed a heavily calcified graft with emphysematous pyelitis (Figure 1). As part of her workup, blood and stool cultures were negative and Strongyloides and Schistosoma serologies were negative. After informed consent regarding surgery and risks, she successfully underwent en bloc graft nephrectomy, appendectomy (due to adhesions) and tract excision. Intraoperative cultures from the resected renal parenchyma were positive for Salmonella spp, type D. Pathology revealed diffuse necrosis with abscess formation in the right transplanted kidney and fistula formation with necrosis and fibrosis (Figure 2). Initial antibiotic therapy at our center was with Ceftriaxone, then broadened to Meropenem based on susceptibilities. Finally, she completed a 14-day course of oral TMP/SMX prior to discharge. She had an uneventful post-operative course. After 6 weeks post-surgery, she was asymptomatic with a well healed wound.
Figure 1:Calcified failed right transplant kidney. calcified, non/hypo-enhancing right failed kidney parenchyma with surrounding fat stranding.

Figure 2:Explanted infected right kidney. photos taken during nephrectomy. visualized parenchyma with diffuse necrosis and abscess formation.
Discussion
Pyelonephritis is fairly common in renal transplant recipients, with an estimated incidence of 3.66 cases per 100 recipient-years.6 In most cases, transplant pyelonephritis is attributed to E. coli, Enterococci and Pseudomonas spp.6 NTS infections account for only an estimated 0.01 to 0.07% of urinary tract infections (UTIs) overall [8], with a paucity of published cases in kidney transplant recipients [4]. NTS has been reported as causing pyelonephritis in hematopoietic stem cell recipients and persons with advanced HIV disease [9-11]. More atypical is renocutaneous fistula formation in this setting, which to our knowledge has not been described in the literature as developing from NTS infection in a transplanted kidney. Renocutaneous fistula most commonly occurs with xanthogranulomatous pyelonephritis, tuberculosis, or postsurgically [12-14]. Often this is a post-obstructive complication, associated with severe inflammation, replacement of the renal parenchyma, or calculus disease. Increased risk of NTS infection has been associated with decreased CD4+ Th17 cells, defects in IL-12/IL-23 cytokine pathways, as well as with the underlying immune dysregulation in HIV and Chronic Granulomatous Disease [1,2]. Transplant recipients with pyelonephritis have 1.9 times greater odds of having been maintained on Mycophenolate mofetil (MMF) [6]. Overlapping or compounding mechanisms from immunosuppressive drugs, particularly the bone marrow suppression associated with MMF, likely contribute to increased susceptibility to UTI, pyelonephritis and NTS infection.
This case presents important surgical and epidemiologic issues for the transplant clinician to consider. The chronicity of the infection created a hostile operative field with dense scarring and adhesions. Initially, a lower midline intra-peritoneal approach was performed and aborted at the other center. We performed the surgery with a retroperitoneal intent initially, making a right Gibson incision to incorporate the fistula tract. Proximal and distal exposure and encircling of the iliac artery was pertinent before addressing the allograft. The appendix was excised en bloc with the allograft, as it was an amalgamated mass involving the appendix.
This patient’s origins in Liberia were important to consider. NTS infections are an emerging cause of bloodstream infection in sub-Saharan Africa and Asia, especially in areas with higher HIV prevalence [15,16] This patient denied any travel back to Liberia since moving to the US in 2001. There is a well-described association between Schistosomiasis and iNTS infection, as persistent helminthic infection can cause recurrent or persistent bacteremia [2]. In this case, despite theoretical risk based on national origin, Schistosoma serologies were negative. Strongyloides serologies were also checked, as there has been a similar association documented with gram negative bacteremia and abscess [17]. These serologies were negative, though both were drawn after several years of ongoing immunosuppression which may impact their reliability. Blood cultures were negative and the origin of this focal infection remains unclear.
Conclusion
In conclusion, NTS infection can manifest as atypical focal infections or invasive disease, specifically in patient populations with an elevated risk profile (including solid organ or stem cell transplant recipients and advanced HIV). This case highlights the difficulty in managing NTS infections in transplant recipients, especially with the development of rare complications such as renocutaneous fistula.
References
- Fierer J (2022) Invasive non-typhoidal salmonella (INTS) infections. Clin Infect Dis 75(4): 732-738.
- Gordon MA (2008) Salmonella infections in immunocompromised adults. J Infect 56(6): 413-422.
- Skourtis G, Papacharalambous G, Makris S, Kasfikis F, Kastrisios g, et al. (2010) Primary aortoenteric fistula due to septic aortitis. Ann Vasc Surg 24(6): 825.e7-e11.
- Samra Y, Shaked Y, Maier MK (1986) Nontyphoid salmonellosis in renal transplant recipients: Report of five cases and review of the literature. Rev Infect Dis 8(3): 431-440.
- Ito K, Nishio H, Iwatani Y, Yamada R, Okawa T, et al. (2017) Kidney allograft pyelonephritis caused by salmonella enterica serovar schwarzengrund. J Infect Chemother 23(7): 481-484.
- Parasuraman R, Julian K (2013) Urinary tract infections in solid organ transplantation. Am J Transplant 13(s4): 327-336.
- Ramos JM, Aguado JM, García-Corbeira P, Alés JM, Soriano F (1996) Clinical spectrum of urinary tract infections due to nontyphoidal salmonella species. Clin Infect Dis 23(2): 388-390.
- Jehangir A, Poudel D, Fareedy SB, Salman A, Qureshi A, et al. (2015) Group D salmonella urinary tract infection in an immunocompetent male. Case Rep Infect Dis 2015: 608632.
- Dadwal SS, Tegtmeier B, Nakamura R, Kriengkauykiat J, Ito J, et al. (2011) Nontyphoidal salmonella infection among recipients of hematopoietic sct. Bone Marrow Transplant 46(6): 880-883
- Guerrero MLF, Ramos JM, Núñez A, Cuenca M, Górgolas MD, et al. (1997) Local infections due to non‐ typhi salmonella in patients with aids: Report of 10 cases and review. Clin Infect Dis 25(3): 690-697.
- Dejman A, Catoe H, Ramdial J, Kupin W (2017) Salmonella abscess in a failed transplanted kidney. Infect Non Infect Dis 3(1): 1-3.
- Caliskan S, Sungur M (2019) Nephrocutaneous fistula after percutaneous nephrolithotomy. J Endourol Case Rep 5(3):137-138.
- Alazab R, Ghawanmeh HM, Abushamma F, Ababneh O, Al-Karasneh AI (2017) Spontaneous nephrocutaneous fistula: Rare complication of xanthogranulomatous pyelonephritis. Urol Case Rep 11: 44-46.
- Weissman S, Ghaffar M, Safavian D, Rubal S, Khabut A, et al. (2018) Nephrocutaneous fistula due to xanthogranulomatous pyelonephritis. Cureus 10(10): e3467.
- Feasey NA, Dougan G, Kingsley RA, Heyderman RS, Gordon MA, et al. (2012) Invasive non-typhoidal salmonella disease: An emerging and neglected tropical disease in Africa. The Lancet 379(9835): 2489-2499.
- Lan NPH, Phuong TLT, Huu HN, Thuy L, Mather AE, et al. (2016) Invasive non-typhoidal salmonella infections in Asia: Clinical observations, disease outcome and dominant serovars from an infectious disease hospital in Vietnam. Plos Negl Trop Dis 10(8): e0004857.
- Ordaya EE, Misra A, Saleh OMA (2022) Strongyloidiasis complicated by gram-negative bacteremia and liver abscesses. Idcases 27: e01392.
© 2021 Talal Al Qaoud. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






