- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Effects of Combined High-Intensity Inspiratory Muscle Training and Aerobic Exercise in Heart Failure Patients with Preserved and Non- Preserved Ejection Fraction: A Systematic Review Protocol of Randomized Control Trials
Maria Isakoglou1, Vaia Sapouna1, Maria Andriopoulou2, Evdokia Billis3, Gerasimos Filippatos4 and Eleni A Kortianou1*
1Physiotherapy Department, University of Thessaly, Greece
2Physiotherapy Department, Asklepieio General Hospital, Greece
3Physiotherapy Department, University of Patras, Greece
4Department of Cardiology, Attikon University Hospital, Greece
*Corresponding author:Eleni A Kortianou, Clinical Exercise Physiology & Rehabilitation Research Laboratory, Physiotherapy Department, School of Health Sciences, University of Thessaly, 3rd km Old National Road Lamia-Athens, Lamia 35100, Greece
Submission: November 25, 2024;Published: December 12, 2024

ISSN 2637-7934 Volume5 Issue2
Abstract
Background: Heart Failure (HF) is a high-prevalence heterogeneous syndrome with various clinical
symptoms. International clinical guidelines recommend that patients with chronic HF participate in
multidisciplinary tailored cardiac rehabilitation programs. This protocol aims to describe the methods for
a systematic review of the literature on the effects of the combination of High Inspiratory Muscle Training
(H-IMT) and aerobic exercise in patients with HF with preserved and non-preserved ejection fraction.
Methods: The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines
will be used to conduct and report this review. Five databases will be searched from inception until 31
December 2024: Medline (via EBSCOhost), PEDro, PubMed, Scopus, and Web of Science. Two reviewers
will independently evaluate articles (titles and abstracts). Methodological quality will be assessed using
the revised Cochrane Risk of Bias tool for randomized trials (RoB2). The Grading of Recommendations
Assessment, Development, and Evaluation (GRADE) approach will be used to assess the overall quality
of the evidence.
Conclusion: Evaluation of the quality of evidence apropos the effects of the combination of H-IMT and
aerobic exercise is essential for improving our knowledge in this field and providing better services for
patients with HF independently of the disease severity.
Trial registration: PROSPERO registration number is CRD42024568200.
Keywords:Aerobic training; Breathing exercises; Ejection fraction; Exercise; Heart failure; Inspiratory muscle training
Introduction
Heart Failure (HF) is a heterogeneous syndrome in which the heart is unable to cope with humans’ metabolic needs. Globally, it impacts 1-3% of the population with accelerating prevalence due to the population growth aging [1], and the high prevalence of comorbidities [2]. Fatigue and dyspnea are frequent clinical symptoms among patients with different severity of HF, mainly associated with exercise intolerance and poor Quality of Life (QoL) [3]. Peripheral muscle [4,5] and inspiratory muscle weakness are reported in patients with both reduced [6] and preserved ejection fraction [7]. Apropos the diaphragm, muscle biopsies showed structural and functional changes [8]. Importantly, the diaphragm excursion during quiet and deep breathing is highly correlated with VO2peak in patients with preserved ejection fraction, showing that inspiratory muscle function correlates with physical status even in less severe patients [9].
In the context of the non-pharmacological approach, published clinical guidelines about exercise in patients with HF highlight the multidisciplinary character of rehabilitation programs [10]. Exercise acts beneficially by reducing the oxidant amount and stimulating the antioxidant capacity in patients with HF [11,12]. European Society of Cardiology recommended aerobic exercise, Inspiratory Muscle Training (IMT), and resistance training for chronic HF patients [13]. IMT is considered an alternative way of exercise for severely deconditioned patients with HF, facilitating the transition to conventional exercise training programs [13].
A systematic review and meta-analysis in patients with systolic
HF revealed that the combination of IMT and aerobic exercise
showed greater improvements in Maximal Inspiratory Pressure
(MIP) and QoL (measured by the Minnesota Living with Heart
Failure Questionnaire, MLwHFQ) compared to conventional exercise
training alone [14]. Additionally, data from a recent systematic
review and meta-analysis in patients with HF demonstrates greater
improvements in MIP when:
a) IMT training loads are high (60%-90% of MIP) compared to
lower training loads (up to 40% of MIP);
b) IMT training period is long (12 weeks compared to 6-8 weeks)
and
c) There is inspiratory muscle weakness (MIP<70% of the
predicted value) [15].
Overall, a systematic review of the effects of the combination of High-intensity Inspiratory Muscle Training (H-IMT) and aerobic exercise in patients with HF with preserved and non-preserved ejection fraction is lacking. Therefore, we aim to fill this gap in knowledge by conducting a systematic review of the contemporary literature that aims to collect and present the effects of H-IMT and aerobic exercise mainly on clinical outcomes in adult patients with HF with preserved and non-preserved ejection fraction. The research question of this review is formulated as follows: “Is the combination of H-IMT (≥60% MIP) and aerobic exercise an effective intervention for improving pulmonary function, cardiac function, exercise capacity, functional capacity, QoL, serum biomarkers, and anti-aging genes in adult patients with HF with preserved and non-preserved ejection fraction compared to low IMT, sham IMT, aerobic exercise, resistance training, or a combination of any aforementioned training, usual care (pharmacological therapy), education or no intervention?”.
Methods
This systematic review will be conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [16,17]. The protocol is registered with the International Prospective Register of Systematic Reviews (PROSPERO: CRD42024568200).
Inclusion criteria
This review will focus on studies evaluating the effectiveness of the combination of H-IMT (≥60% MIP) and aerobic exercise on pulmonary function, cardiac function, exercise capacity, functional capacity, QoL, serum biomarkers, and anti-aging genes. Studies for review will be selected according to the following eligibility criteria, categorized by population, type of intervention, comparisons, and outcomes (PICO) [18]. The setting is going to be in/outpatients (hospitalized or not hospitalized). Any studies excluded will be reported on the PRISMA flow chart [19].
Population
Adult patients (≥18 years) with HF with preserved and nonpreserved ejection fraction will be the population. If studies report on mixed samples, i.e., with different chronic diseases including HF, they will be included only if data for the aforementioned population is reported and presented separately. There will be no restrictions on characteristics such as gender or ethnicity.
Types of interventions
This review will include studies that use combined protocols of H-IMT (≥60% MIP) and aerobic exercise to promote clinical improvement in parameters affected by the disease such as pulmonary function, cardiac function, exercise capacity, functional capacity, QoL, serum biomarkers, and anti-aging genes. For this review, IMT will be defined as a respiratory training method in which muscles with inspiratory function, mainly the diaphragm, are exercised to enhance respiratory muscle strength [20] and endurance and to yield improvements in respiratory function [21]. Moreover, aerobic exercise will be defined as a rhythmic activity that uses large muscle groups to improve cardiovascular endurance [22]. The intervention will be delivered or monitored by rehabilitation staff (e.g., physiotherapists) either in-person or remotely (synchronous or asynchronous) at the hospital or at home.
Comparisons or controls
For the control or Comparator Group (CG), the type of approach can be any of the following: low IMT (25-40% MIP), sham IMT (0- 15% MIP), aerobic exercise, resistance training, or a combination of any aforementioned training, usual care, education or no intervention. Usual care can be defined as the pharmacological intervention that would normally be received by patients with HF as part of their treatment pathway.
Outcome measures
This review will include studies that focus mainly on clinical outcomes. Primary outcomes are any clinical outcome that refers to physical components related to disease progression such as pulmonary function, cardiac function, exercise and functional capacity, and QoL. Secondary outcomes, such as serum biomarkers of inflammation, myocardial stress, and anti-aging genes, will be included.
Study Design
Randomized Controlled Trials (RCTs) that apply high training loads of IMT approaches in combination with aerobic exercise will be included. For mixed-method studies, only the quantitative data will be used for analysis. In case of homogeneity in study designs, study population, demographic characteristics, measurement tools, intervention types, and outcomes, a meta-analysis will be conducted.
Exclusion criteria
Studies that include participants <18 years, have patients other than those with HF, do not focus on the combination of H-IMT (≥60% MIP) and aerobic exercise, and are non-written in English will be excluded. Furthermore, non-randomized controlled trials, observational studies, systematic reviews, meta-analysis, narrative reviews, book reviews, book chapters, dissertations theses, commentaries, editorials and letters to the editor, grey literature, editorial or opinion articles, consensus statements, clinical practice guidelines, protocols, case reports, conference articles, data and results from abstracts of conference presentations will not be included. Nevertheless, relevant systematic reviews will be used for a hand-held search for the identification of potentially eligible studies for inclusion. No restrictions regarding the time of publication will be applied.
Information sources
Potential studies will be identified by searching systematically the following sources/databases: Medline (via EBSCOhost), PEDro, PubMed, Scopus, and Web of Science from the period of the inception until December 31, 2024. Up-to-date and comprehensive search strategies will be developed based on database suggestions to ensure search effectiveness.
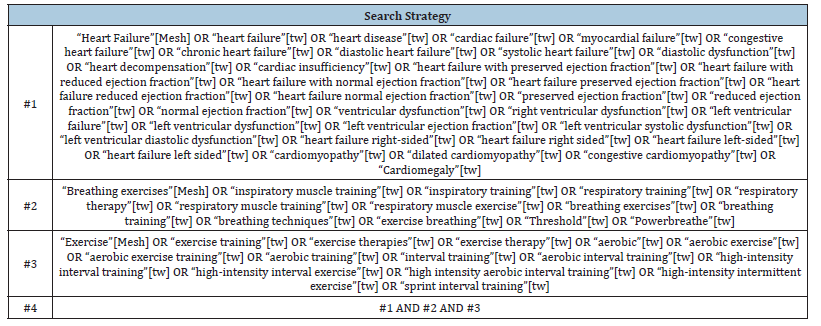
Search strategy
The initial search strategy will be developed in PubMed (Table 1). Key index terms will be determined through discussions between two researchers (MI and MA). The concepts and key index terms used in a preliminary search will later be adapted to the selected databases. Keywords will be in English and combined using Boolean logical operators (AND and OR).
Table 1:Search strategy for PubMed.
Study selection
We will use a multistage process for study selection. Initially, all retrieved studies will be imported into the Rayyan (Qatar Computing Research Institute) Web app, and duplicate studies will be automatically removed (https://www.rayyan.ai/). Two researchers (MI and VS) will independently screen all potential titles that generally appear to meet the inclusion/exclusion criteria. Then, the same researchers will independently evaluate all abstracts and identify studies for full-text review according to the inclusion and exclusion criteria. Discrepancies between the two reviewers, at any stage of study selection will be resolved by a third independent researcher (EK) until consensus is achieved. The excluded studies will be reported in the PRISMA flow chart.
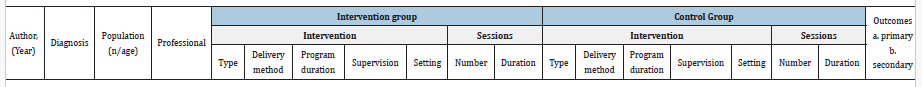
Data extraction process
After literature screening, two independent researchers (MI and VS) will extract data from eligible studies using a studyspecific data extraction form. Data extraction (selection and coding) will be performed on the relevant variables from the initial RCT and supplementary materials. The form will focus on the following domains: author, year, diagnosis, population (age, NYHA classification), professional, intervention group (type, delivery method, duration of the program, supervision, setting, number of sessions, duration of sessions), control group (type, delivery method, duration of the program, supervision, setting, number of sessions, duration of sessions), and outcome measures (before and after treatment differences) (Table 2). This form will be reviewed by the research team to ensure that it is capturing the information accurately. Data from eligible studies will be extracted independently by two reviewers (MI and VS) using the pre-designed data extraction form. In case of discrepancies, a third reviewer will be consulted (EK). For studies that are not fully available online or have incomplete data, additional communication with the authors will be sought. To ensure a timely delivery of this review the authors will have 2 weeks to answer our questions. Otherwise, the study will be described as “vague” and will be excluded from analysis thereafter.
Table 2:Data extraction form.
Risk of bias assessment
The quality of studies will be assessed independently by two researchers (MI and EB), using the revised Cochrane Risk of Bias tool for randomized trials (RoB2). The RoB2 tool is used to assess and report the risk of bias for the following five domains: randomization, deviations from intended interventions, missing outcomes, measurement of the outcome, and selection of the reported results. Each domain item is rated as “low risk”, “high risk”, or “some concerns” and can be summarized with an overall risk-ofbias judgment [23]. The study has a high overall bias if it has a “high risk” in at least one direction. The overall bias is low if the study has “low risk” in all directions. Otherwise, it has a medium risk of bias (“some concerns”). A third researcher (GF) will intervene only in cases of discrepancies between the two independent researchers.
Synthesis of results
A narrative descriptive synthesis of the quantitative findings will be conducted for each study’s outcomes. Differences referred to methodological characteristics of the included studies will be investigated and discussed. The overall quality of the evidence will be assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach [24]. The GRADE approach includes the following domains of assessment: risk of bias, inconsistency, publication bias, indirectness of study results, and imprecision [25]. The quality of evidence is rated as “high”, “moderate”, “low” or “very low” based on the risk of bias, imprecision, inconsistency, indirectness, and publication bias.
Discussion
To our knowledge, this is the first systematic review that aims to investigate and present the effects of combining H-IMT and aerobic exercise in patients with HF. A recent systematic review and meta-analysis of 93 studies in patients with preserved (11 studies) and reduced ejection fraction (82 studies) indicated that exercise capacity and QoL are improved after exercise training programs (isolated or combined: aerobic exercise, IMT, resistance training, functional electrical stimulation, blood flow restriction, tai-chi) [26]. Apropos the respiratory muscle, a relevant systematic review (7 studies, 203 patients) revealed that training intensity at 60% of MIP (6 times per week) had notable effects on inspiratory muscle strength, and walking distance after 12 weeks of intervention [27]. Furthermore, a systematic review by Azambuja et al. [15] concluded that IMT could be an alternative type of training for severe patients with HF who cannot participate in a conventional exercise program mainly composed of aerobic training [15]. A previous metaanalysis of 5 RCTs (138 patients) reported that H-IMT is a useful strategy for improving exercise capacity and inspiratory muscle strength in patients with reduced ejection fraction [28]. For patients with preserved ejection fraction, apart from the presence of exercise intolerance [29], alterations in the diaphragm [9] and inspiratory muscle weakness [7] are mentioned in the literature. Relating to this group of patients, a recent meta-analysis (4 RCTs with 165 patients) revealed that even low (25-30% MIP) training loads had benefits on maximal and submaximal exercise capacity (cardiorespiratory fitness) after 12 weeks [30]. Considering that patients with preserved ejection fraction correspond to 50% of patients with HF [31], this highlights the need to investigate the effects of combined H-IMT and aerobic exercise on this population.
Our systematic review will include RCTs that combine H-IMT (≥60% MIP) and aerobic exercise in adult patients with HF with preserved and non-preserved ejection fraction. It is important to systematically review and analytically present the effects of combined H-IMT and aerobic exercise on outcomes that are evaluated (pulmonary function, cardiac function, exercise, and functional capacity, QoL, serum biomarkers, and anti-aging genes) to define the possible effects of including H-IMT in the conventional rehabilitation approaches for patients with different disease severity.
Strengths and limitations
The prominent strengths of this systematic review are the inclusion of only RCTs, the use of the GRADE approach for the assessment of the methodological quality of evidence, and the RoB2 tool for the assessment of the risk of bias. The expected homogeneity in study designs, study population, demographic characteristics, measurement tools, and intervention types may lead to retrieval results for a meta-analysis. Furthermore, the combination of the types of exercise (H-IMT and aerobic exercise) in both preserved and non-preserved ejection fraction patients is pioneering. Despite the above-mentioned strengths of our study, this systematic review will face some limitations. Considering the poor number of studies referring to patients with preserved ejection fraction, our systematic review may bring to light a small number of RCTs about combined H-IMT and aerobic exercise. Additionally, we will include studies written only in the English language which may limit studies that could contribute to the evidence base.
Implications
This systematic review is expected to provide evidence referring to the combination of H-IMT and aerobic exercise. The results may support feasible rehabilitative interventions for patients with HF independently of the disease severity.
Conclusion
At present, the increasing rate of patients with HF judge the necessity of studying combined components of rehabilitation programs as an alternative way of approaching this patient population. Currently, there are important gaps in knowledge about the effectiveness of combined H-IMT and aerobic exercise in patients with HF. We expect that this systematic review will highlight the possible effects of combined H-IMT and aerobic exercise in patients with HF being an essential step for evidence-based clinical practice.
Ethics and Dissemination
Approval for the protocol and the systematic review is not required. Findings in the systematic literature review will be submitted to a peer-reviewed journal.
References
- Khan MS, Shahid I, Bennis A, Rakisheva A, Metra M, et al. (2024) Global epidemiology of heart failure. Nat Rev Cardiol 21(10): 717-734.
- McDonagh ST, Dalal H, Moore S, Clark CE, Dean SG, et al. (2023) Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev 10(10): CD007130.
- Del Buono MG, Arena R, Borlaug BA, Carbone S, Canada JM, et al. (2019) Exercise intolerance in patients with heart failure: JACC state-of-the-art review. J Am Coll Cardiol 73(17): 2209-2225.
- Tkaczyszyn M, Drozd M, Węgrzynowska-Teodorczyk K, Bojarczuk J, Majda J, et al. (2021) Iron status, catabolic/anabolic balance, and skeletal muscle performance in men with heart failure with reduced ejection fraction. Cardiol J 28(3): 391-401.
- Saw EL, Ramachandran S, Valero-Muñoz M, Sam F (2021) Skeletal muscle (dys)function in heart failure with preserved ejection fraction. Curr Opin Cardiol 36(2): 219-226.
- Palau P, Domínguez E, Ramón JM, López L, Briatore AE, et al. (2019) Home-based inspiratory muscle training for management of older patients with heart failure with preserved ejection fraction: Does baseline inspiratory muscle pressure matter? Eur J Cardiovasc Nurs 18(7): 621-627.
- Spiesshoefer J, Henke C, Kabitz HJ, Bengel P, Schütt K, et al. (2021) Heart failure results in inspiratory muscle dysfunction irrespective of left ventricular ejection fraction. Respiration 100(2): 96-108.
- Salah HM, Goldberg LR, Molinger J, Felker GM, Applefeld W, et al. (2022) Diaphragmatic function in cardiovascular disease: JACC review topic of the week. J Am Coll Cardiol 80(17): 1647-1659.
- Andriopoulou M, Dimaki N, Kallistratos MS, Chamodraka E, Jahaj E, et al. (2022) Skeletal muscle alterations and exercise intolerance in heart failure with preserved ejection fraction patients: Ultrasonography assessment of diaphragm and quadriceps. Eur J Heart Fail 24(4): 729-731.
- Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, et al. (2022) AHA/ACC/HFSA guideline for the management of heart failure: A report of the American college of Cardiology/American heart association joint committee on clinical practice guidelines. Circulation 145(18): e895-e1032.
- Martins IJ (2017) Single Gene inactivation with implications to diabetes and multiple organ dysfunction syndrome. J Clin Epigenet 3(3): 24.
- Corbi G, Conti V, Troisi J, Colucci A, Manzo V, et al. (2019) A cardiac rehabilitation increases SIRT1 activity and β-hydroxybutyrate levels and decreases oxidative stress in patients with HF with preserved ejection fraction. Oxid Med Cell Longev 2019: 7049237.
- Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, et al. (2021) 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J 42(1): 17-96.
- Gomes Neto MG, Martinez BP, Conceição CS, Silva PE, Carvalho VO (2016) Combined exercise and inspiratory muscle training in patients with heart failure: A systematic review and meta-analysis. J Cardiopulm Rehabil Prev 36(6): 395-401.
- Azambuja ACM, de Oliveira LZ, Sbruzzi G (2020) Inspiratory muscle training in patients with heart failure: What is new? Systematic review and meta-analysis. Phys Ther 100(12): 2099-2109.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, et al. (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1): 1.
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, et al. (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 350: g7647.
- Kloda LA, Boruff JT, Cavalcante AS (2020) A comparison of patient, intervention, comparison, outcome (PICO) to a new, alternative clinical question framework for search skills, search results, and self-efficacy: a randomized controlled trial. J Med Libr Assoc 108(2): 185-194.
- Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372: n160.
- Bissett BM, Leditschke IA, Neeman T, Boots R, Paratz J (2016) Inspiratory muscle training to enhance recovery from mechanical ventilation: A randomised trial. Thorax 71(9): 812-819.
- Li H, Tao L, Huang Y, Li Z, Zhao J (2022) Inspiratory muscle training in patients with heart failure: A systematic review and meta-analysis. Front Cardiovasc Med 9: 993846.
- Patel H, Alkhawam H, Madanieh R, Shah N, Kosmas CE, et al. (2017) Aerobic vs anaerobic exercise training effects on the cardiovascular system. World J Cardiol 9(2): 134-138.
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, et al. (2019) RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366: 4898.
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, et al. (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4) :401-406.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, et al. (2008) GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650): 924-926.
- Edwards JJ, O'Driscoll JM (2022) Exercise training in heart failure with preserved and reduced ejection fraction: A systematic review and meta-analysis. Sports Med Open 8(1): 76.
- Sadek Z, Salami A, Joumaa WH, Awada C, Ahmaidi S, et al. (2018) Best mode of inspiratory muscle training in heart failure patients: A systematic review and meta-analysis. Eur J Prev Cardiol 25(16): 1691-1701.
- Gomes Neto MG, Ferrari F, Helal L, Lopes AA, Carvalho VO, et al. (2018) The impact of high-intensity inspiratory muscle training on exercise capacity and inspiratory muscle strength in heart failure with reduced ejection fraction: A systematic review and meta-analysis. Clin Rehabil 32(11): 1482-1492.
- Upadhya B, Haykowsky MJ, Eggebeen J, Kitzman DW (2015) Exercise intolerance in heart failure with preserved ejection fraction: More than a heart problem. J Geriatr Cardiol 12(3): 294-304.
- Baral N, Changezi HU, Khan MR, Adhikari G, Adhikari P, et al. (2020) Inspiratory muscle training in patients with heart failure with preserved ejection fraction: A meta-analysis. Cureus 12(12): e12260.
- Palau P, Domínguez E, Núñez E, Schmid JP, Vergara P, et al. (2014) Effects of inspiratory muscle training in patients with heart failure with preserved ejection fraction. Eur J Prev Cardiol 21(12): 1465-1473.
© 2024 Eleni A Kortianou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






