- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
The Application of Wearable Devices in Knee Injury and Prevention: Narrative Systematic Review
Na Cui#1,2, Tianyuan Liang#3, Ruiqin Dang1,2, Shuang Ren1* and Jianquan Wang*1
1Department of Sports Medicine, Peking University Third Hospital, Institute of Sports Medicine of Peking University, Beijing Key Laboratory of Sports Injuries, Engineering Research Center of Sports Trauma Treatment Technology and Devices, Ministry of Education, China
2Tianjin Key Laboratory of Exercise Physiology and Sports Medicine, Institute of Sport, Exercise & Health, Tianjin University of Sport, China
3Department of Chinese Medicine, Hebei North University, China
#Refers to First Author of the article
*Corresponding author:Shuang Ren and Jianquan Wang, Department of Sports Medicine, Peking University Third Hospital, Institute of Sports Medicine of Peking University, Beijing Key Laboratory of Sports Injuries, Engineering Research Center of Sports Trauma Treatment Technology and Devices, Ministry of Education, Beijing, 49 Huayuan North Road, Haidian District, Beijing, China
Submission: November 14, 2024;Published: November 21, 2024

ISSN 2637-7934 Volume5 Issue2
Abstract
In recent years, wearable devices have rapidly emerged in the medical field, offering simplicity of operation, low cost, and freedom from spatial constraints, holding broad prospects in orthopedic rehabilitation. This article analyzes the application of wearable devices in the prevention, assessment, and training of knee joint injuries, summarizing their current status in the prevention and treatment of knee injuries, and points out the current shortcomings. It also proposes future research prospects for wearable devices in the medical field, aiming to provide a reference for further application and research of wearable devices in knee joint injuries.
Keywords:Wearable devices; Knee joint; Telerehabilitation; Gait assessment; Injury prevention
Introduction
With the rise of internet healthcare and the in-depth development of sensor technology, countries are continuously advancing the regulation of digital health technologies, which has spurred rapid development of medical software, wearable devices, and new technologies for medical product research [1]. Among them, wearable devices have rapidly emerged in the medical field, playing a crucial role in promoting the development of interconnected healthcare [2-4], and hold broad prospects in orthopedic rehabilitation applications. Wearable devices are a collection of sensors that record physiological characteristics of the human body, mostly fixed on joints, heads, or clothing to measure various physiological indicators [5]. They typically come equipped with accelerometers, gyroscopes, heart rate and blood oxygen monitors, and Global Positioning Systems (GPS), and combine Inertial Measurement Units (IMU) and pressure sensors to collect and integrate human data [6]. Wearable devices come in various forms, providing a range of functions from communication and entertainment to health monitoring. In the field of medical health, wearable devices can be worn directly on the body in the form of portable medical or health electronic devices, maintaining health through perception, recording, analysis, adjustment, and intervention [7]. Clinically, these devices are mainly used for health and safety monitoring, chronic disease management, disease diagnosis, treatment, and rehabilitation [8-11]. The indicators that wearable devices can collect include kinematic dynamics and other musculoskeletal biomechanical indicators, as well as physiological indicators such as cardiopulmonary blood oxygen, etc. This review mainly introduces the application of motion analysis wearable devices based on IMU and plantar pressure insoles.
Compared with other methods of assessing knee joint motion such as three-dimensional motion capture, wearable devices have the advantages of being easy to operate, having short test times, and not being limited by space, which facilitates their widespread application. Currently, sensor-based wearable devices have gradually been applied to measure joint angles and temporal characteristics during knee motion, used to monitor gait mechanics and the range of motion of lower limb joints, and have achieved good results [12]. They can also be combined with remote rehabilitation systems to provide real-time feedback on patients’ rehabilitation training, helping clinicians adjust training plans and for postoperative gait assessment and retraining. Technology companies such as Microsoft, OPPO, and Amazon have all developed wearable devices for patients recovering from Total Knee Arthroplasty (TKA), such as Fitbit, Garmin, Misfit, etc. A study [13] introduced a wearable system for identifying knee joint angles through IMU sensors, which can sense changes in knee joint angles to recognize leg movements through an ESP32 microcontroller and an MPU-6050 sensor, achieving precise angle measurement with an average error of less than 0.6 degrees. The team also developed a matching mobile application interface that can respond immediately and successfully recognize executed movements. The convenience and motion monitoring capabilities of wearable devices not only provide timely feedback on patients’ conditions during the rehabilitation process, increasing training participation [14], but also apply to gait and joint angle assessments, and even prevent joint injuries caused by incorrect postures. They show great potential in applications related to knee joint injuries [15-17].
Objective
This article analyzes the application of wearable devices in the prevention, functional assessment, and rehabilitation training of knee joint injuries, summarizes their current status in knee joint injury applications, and points out the current shortcomings. It also proposes future research prospects for the application of wearable devices, aiming to provide a reference for further application and research of wearable devices in knee joint injuries.
Methods Search Strategy
We conducted a comprehensive literature search on October 1, 2024. The following electronic databases were searched with the assistance of an information specialist at the medical library: Pubmed, Embase, Web of science. Searched literature published since the inception of the database. The searching strategy combined of “wearable devices”, “knee”, “telerehabilitation”. We conducted literature search using Medical Subject Headings (MeSH) or Emtree, and free text terms. In addition, the relevant literature was retrieved by the tracking literature method. A detailed search strategy is provided in the supplementary material.
Inclusion and exclusion criteria
Inclusion research criteria were
i. Trials that have proven the effectiveness of wearable
devices;
ii. Studies focusing on clinical applicability;
iii. Studies published in English;
iv. Studies describing completed research;
Exclusion criteria were theoretical papers, books, letters, reviews, perspectives and editorials.
Result
Literature screening process and results
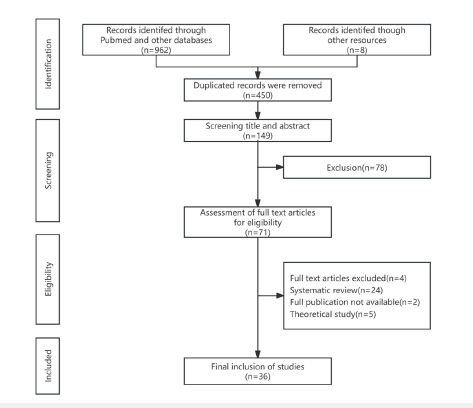
After reviewing the title and abstract, the search identified 450 potentially relevant documents. Among them, 36 papers met the inclusion criteria after full-text review (Figure 1).
Figure 1:Literature screening process.
Safety and effectiveness of wearable devices
For patients with knee joint injuries, regardless of whether conservative treatment or surgical intervention is chosen, improper rehabilitation exercises carry the risk of exacerbating knee joint damage. It is essential to adopt safe and effective methods to assist in training and monitor bodily movement signals during rehabilitation. Wearable devices are operationally safe, easy to wear, and capable of real-time monitoring of knee joint training movements. They can also be combined with remote rehabilitation platforms to provide immediate feedback and motivation, helping patients better adhere to training plans and ensuring the effectiveness of the training. A previous study [18] constructed a highly sensitive and broad-range stretchable flexible pressure sensor for knee joint rehabilitation, which achieved sensor-integrated dynamic deep learning for effective monitoring and active tracking of the user’s biophysical signals, accurately predicting knee joint postures, and is suitable for biophysical monitoring and deep learning-based knee joint rehabilitation training. Riffitts [19] used a smart instrumented knee brace system with wearable magnetic units and IMUs to estimate knee kinematics, allowing participants to complete a series of common knee rehabilitation exercises and exercise games, and compared the angles and velocities recorded by the knee brace with those of a reference optoelectronic system. The results showed good consistency between the knee brace system and the reference system for all exercises performed, and participants were able to quickly learn the exercise games and achieve good results. This further indicates that rehabilitation systems assisted by wearable devices have the potential to enable rehabilitation outside the clinic through remote monitoring and improve patient training compliance and outcomes by using exercise games, thereby effectively ensuring the safety and effectiveness of the rehabilitation training plan.
Rehabilitation training after knee joint injuries has stringent requirements for the standardization of movements and the variation in training angles. On one hand, non-standard knee movements often lead to compensatory postures, which not only fail to achieve the desired training effects but may also lead to a series of issues such as secondary joint injuries. On the other hand, accurate angle determination also helps physicians assess the current condition of patients and formulate subsequent treatment plans. Therefore, as a tool to assist in training, the measurement precision and reliability of wearable devices are fundamental to high-quality rehabilitation assessment and training.
Accuracy and reliability of wearable devices
Bell [20] developed a remote rehabilitation management system that combines wireless IMU, interactive mobile applications, and a web-based clinician portal (interACTION). Ten healthy subjects were asked to perform ten repetitions of three knee rehabilitation exercises using the interACTION application, with IMU motion tracking sensors and video-based motion tracking systems recording the exercises simultaneously to verify the accuracy of the IMU-based knee angle measurement system in common physical therapy exercises. The results showed moderate to good consistency between the two systems in all exercises, with accuracy within 3° and the program was well-received. In another study on accuracy and reliability [21], a wearable knee brace applying elastic sensors was designed as a new tool for continuous measurement of knee flexion angles. It was validated using the kinematic measurement gold standard Vicon. The validated tool showed good reproducibility and repeatability in testers (average measurement range=5.82°±1.93°), high precision (root mean square error <1.28°), and good reliability (intraclass correlation coefficient 0.80-0.91). Additionally, a study [22] assessed the kinematic parameters extracted by wearable IMUs and wearable magnetic measurement units using the gold standard optoelectronic system, also showing reasonable accuracy (RMSE <8°) and very strong correlation (correlation coefficient >0.86), effectively validating the precision and reliability of wearable devices. Oubre [23] designed a reliable, energy-efficient, and low-cost wearable system for longterm monitoring of joint kinematics in an outpatient setting, with 17 subjects wearing sensors to walk at three different self-selected speeds, estimating joint angles based on calibrated sensor values and their derivatives. The system’s estimated Root Mean Square Error (RMSE) for knee flexion/extension angles was 5.0°±1.0°, validating the wearable device’s ability to accurately estimate knee flexion/extension angles during motion at different walking speeds.
The application of wearable devices in post-knee surgery rehabilitation
The knee joint bears most of the body’s weight and extremely high pressure loads during movement, making it very fragile and prone to Osteoarthritis (OA). Knee injuries account for up to 50% of musculoskeletal disorders and are among the most costly injuries in terms of economic impact [24,25], requiring expensive surgical interventions and postoperative rehabilitation. According to data from the World Health Organization (WHO) [26], there is a significant unmet need for rehabilitation services, with over half of the population in some low- and middle-income countries lacking access to the rehabilitation services they require. However, rehabilitation training after knee injury is crucial; on one hand, conservative treatment and rehabilitation training for patients are cost-effective and can avoid surgical trauma, which is of great importance. On the other hand, postoperative rehabilitation, such as after Anterior Cruciate Ligament Reconstruction (ACLR) or total knee replacement, often requires a long period of rehabilitation for patients to regain their previous level of function, making the importance of rehabilitation training even more undeniable. Scientific rehabilitation training aids in the recovery of knee joint function, enhancing muscle strength around the knee, relaxing the joint capsule, and improving knee flexibility. Improper rehabilitation movements not only fail to aid joint recovery but can also cause further joint damage.
Traditional rehabilitation models currently have some undeniable shortcomings, such as high costs, restrictions in time and location, and the tedious process leading to poor patient compliance, which severely affect the effectiveness of sports rehabilitation [27]. Therefore, home-based rehabilitation exercises, whether supervised or unsupervised, are considered the preferred choice for patients after discharge due to their convenience [28- 30]. Using remote rehabilitation systems to monitor the quality and accuracy of patients’ home-based rehabilitation exercises can play a significant role in their recovery training. Telemedicine primarily utilizes network communication technology, wearable devices, or various telemedicine platforms to establish a communication platform between orthopedic doctors and patients, providing more direct and specific guidance for patient rehabilitation. It can offer remote real-time feedback and guide the rehabilitation process, achieving effects unattainable by traditional follow-up methods [31,32], and ensuring the continuity of rehabilitation treatment from the hospital to the home [33].
Hoher [34] analyzed the raw data from 604 knee injury patients using Digital Medical Devices (DMDs) in a home setting, which included 10,311 measurements. Compared to the control group, DMD users showed significantly higher compliance with rehabilitation interventions (86% [77-91] vs. 74% [68-82], p<0.05). DMD users engaged in more intense exercises at home without reporting adverse events. This indicates that the use of novel digital medical devices with the potential to improve rehabilitation outcomes can enhance patient compliance, thereby achieving evidence-based remote rehabilitation. A team [35] developed a system using three wearable accelerometers as signal sources to extract time-domain features, frequency-domain features, and angle information, identifying exercise types and deviations from correct movements in the home rehabilitation setting for patients with knee OA, detecting improper rehabilitation movements, and providing remote monitoring for physicians to assess the accuracy of patient rehabilitation. The study results also showed that this method has a high level of motion detection accuracy, meeting the requirements of a rehabilitation motion assessment system.
Remote rehabilitation using wearable devices has shown significant effectiveness in postoperative recovery for patients who have undergone knee replacement surgery. A sensor-based home rehabilitation study involving 1,321TKA subjects [36] reflected that sensor-based home rehabilitation can effectively improve subjective and objective outcomes after TKA surgery. The study reported favorable outcomes in the Knee Injury and Osteoarthritis Outcome Score (KOOS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Knee Society Score (KSS) for patients post-surgery. Additionally, there was an increase in physical activity, and improvements in Range of Motion (ROM) and Timed Up-and-Go (TUG) outcomes after rehabilitation training.
Cooper [37] reported on the use of wearable sensors (BPM pathway; 270Vision) to remotely monitor participants’ rehabilitation progress and movement up to 9 weeks post-surgery during the COVID-19 pandemic. The device was found to track patients’ range of motion during the study period and reduced the need for face-to-face physical therapy by 35.7%. Over 80% of users indicated that the wearable device was easy to operate, had a good user experience, and increased their motivation to exercise. This further illustrates that remote monitoring of rehabilitation training using wearable devices is feasible and can alleviate the burden on outpatient physical therapy services.
Wearable devices have also shown positive effects when applied to rehabilitation training after Anterior Cruciate Ligament Reconstruction (ACLR). A previous study [38] explored the application effects of smart wearable devices in the home rehabilitation of 60 ACLR patients. Patients were randomly divided into two groups: the control group received conventional rehabilitation training, while the observation group wore smart wearable devices for rehabilitation supervision and guidance alongside conventional rehabilitation. Postoperative assessments of knee range of motion, Lysholm knee score, thigh circumference difference, and rehabilitation exercise compliance were conducted for both groups. The results showed that the observation group had better scores and thigh circumference differences at various postoperative time points compared to the control group, further proving that smart wearable devices can effectively improve knee joint range of motion and function, promote muscle recovery, and increase patient compliance with rehabilitation exercises in the early stages after ACL reconstruction.
It is evident that the development of remote rehabilitation systems based on wearable devices saves patients the time and high costs associated with traditional face-to-face rehabilitation, providing them with rehabilitation resources in a low-cost and convenient manner while increasing their motivation to train. For clinical physicians, these systems not only save medical resources but also enable more precise monitoring of patients’ postoperative recovery, facilitating timely communication with patients to adjust rehabilitation plans, thus leading to better outcomes. Therefore, the potential of remote rehabilitation systems based on wearable devices in post-knee injury rehabilitation training warrants further exploration. Future studies should conduct specialized cost-benefit analyses to assess this approach and promote its widespread adoption in healthcare systems.
The application of wearable devices in gait assessment after knee surgery
Gait analysis plays a crucial role in diagnosing musculoskeletal and neurological disorders and in evaluating the effectiveness of various patient interventions [39]. Traditional three-dimensional motion analysis systems, long considered the gold standard for gait assessment, offer objective and quantitative insights into kinematics and spatiotemporal parameters [40]. These systems typically rely on three-dimensional motion capture technologies (such as VICON, Qualisys) paired with force plates. However, they are not without their shortcomings, including operational complexity, the requirement for highly skilled personnel, extended processing times, and spatial constraints. Wearable IMU, with their compact design and affordability, enable frequent, real-time patient monitoring and provide clinically significant objective biomechanical data [41], presenting a convenient approach to gait data collection for both research and clinical practice.
The potential of inertial sensors for the objective assessment of gait in OA patients is significant. Gait parameters obtained from inertial sensors can highlight deviations in knee OA patients’ gait compared to healthy controls, positioning these sensors as a viable means of detecting gait impairments in knee OA patients [42]. A comprehensive review by Kobsar [43] on the application of inertial sensor-based wearable devices in OA gait analysis reveals a rapid expansion in research and an increased application of biomechanical analysis for lower limb OA patients. Studies on the use of mobile apps and wearable devices in post-TKA rehabilitation have demonstrated their accuracy in patient monitoring and effectiveness in gait and motion analysis [44]. Despite this, the application of wearable devices in gait assessment for OA patients remains limited, and future longitudinal research is essential to advance the integration of wearable inertial sensors in the diagnosis and treatment of OA.
Sensor-derived gait parameters can also be applied to the assessment of gait following various knee surgeries. A study [45] reviewed the application of wearable IMU in gait analysis among adults after TKA, demonstrating the potential of using WIMU to remotely collect gait data from TKA patients in their daily lives. Boekestei [46] utilized inertial sensors to gather gait parameters and analyzed the recovery of gait after TKA and Total Hip Arthroplasty (THA), comparing the results with the recovery of self-reported function (PROM) and pain scores. The study found that gait parameters returned to the levels of a healthy control group after TKA and THA. Notably, the trajectory of improvement in gait parameters two months post-surgery did not align with the significant and early improvements found in PROMs. This study suggests that sensor-derived gait parameters can be applied to the assessment following TKA and THA and can provide an assessment of physical function that is not obtainable through self-reporting.
In addition to gait assessment, wearable devices can also assist in guiding gait training. Wang [47] conducted a study involving 71 patients with early-stage medial knee osteoarthritis, randomly assigning them to a walking exercise group and a gait retraining group. The gait retraining group underwent six weeks of gait retraining using wearable devices. The results showed that, compared to before training, the gait retraining group experienced a significant reduction of 16.5% (P<0.001) in Knee Adduction Moment (KAM) and 35.5% (P<0.001) in VAS scores, with a significant improvement in KOOS scores (p=0.004), while the walking exercise group did not show significant changes in these parameters. The aforementioned studies provide significant insights into the clinical application of wearable devices in gait assessment and training but are not without limitations. Due to the short duration of the studies and the lack of follow-up, further research is needed to validate the clinical application effects of real-time feedback-based gait training.
The application of wearable devices in muscle strength assessment after knee surgery
The principal objectives of post-injury or post-surgical rehabilitation exercises are to regain normal joint mobility, muscle strength, and endurance [48]. Consequently, the assessment of muscle strength is of paramount importance in the rehabilitation process following joint injuries. Methods currently employed in clinical settings, such as manual muscle testing and handheld dynamometry, are often unreliable, while Isokinetic Dynamometers (IKD), despite their reliability, are not portable [49,50]. Wearable devices, with their convenience and precision, are well-suited for the assessment of knee muscle strength. Myong [51] introduced a Portable Articulated Dynamometer System (PADS) that enables the evaluation of knee extension strength by affixing load cells to the limbs, without the need for any environmental setup or connections. This innovation streamlines the process of muscle strength measurement in terms of time and space. Park [52] developed a Wearable Dynamometer System (WDS) with a knee joint torque sensor, validating its accuracy and confirming the reliability of the measurements obtained from the wearable system. Researchers [53] have also suggested employing wearable devices to measure isometric muscle strength as an innovative quantitative metric for post-TKA assessment. Their study presented a wearable brace for the rehabilitation of TKA patients, which includes a force sensor for isometric muscle strength assessment and an active angle sensor for monitoring knee flexion, facilitating self-assessment of rehabilitation progress and demonstrating the system’s feasibility and significance through clinical trials. Significantly, this brace quantifies the rehabilitation journey of TKA patients in terms of muscle power deficiency and introduces a novel quantitative metric for evaluating TKA recovery: The Isometric Muscle Test Score (IMTS). It is clear that as technology advances, research into wearable devices is diversifying and maturing, with the potential to become a standard in knee muscle strength assessment in the future.
The application of wearable devices in knee injury prevention
Running stands out as a cost-effective and easily accessible physical activity that enhances health and is a widely practiced form of exercise. Yet, the risk of knee injuries associated with running is significant, underscoring the critical need for injury prevention strategies. Knee injuries are among the most common injuries in runners and are often linked to abnormal running postures. Patellofemoral Pain (PFP), in particular, is a primary cause of knee pain among runners. Noehren [54] performed an instrumented gait analysis on 400 healthy female runners, tracking injuries over a two-year period, and compared the initial running mechanics of those who sustained injuries with an equal number of uninjured runners. The findings revealed that women who developed PFP exhibited markedly greater hip adduction angles during running, indicating a potential link between hip adduction angles and patellar pain. Runners are also prone to lateral knee pain due to Iliotibial Band Syndrome (ITBS). A prospective study [55] compared the lower limb kinematics and kinetics between a group of female runners with ITBS and a healthy control group, observing that the ITBS group showed significantly greater hip adduction and knee internal rotation during the stance phase of running. This suggests that ITBS may be related to increased peak hip adduction and knee internal rotation, which could exacerbate strain on the iliotibial band, leading to compression against the lateral femoral condyle and consequent knee injury. Additionally, a study [56] assessed the ankle, knee, and hip kinematics, kinetics, and ground reaction force characteristics of injured and non-injured cross-country runners over a 14-week season, finding that injured runners had a higher peak Knee Adduction Moment (KAM). This implies that modifying lower limb gait to decrease KAM could be a crucial approach to preventing running-related injuries.
In running posture, the angle of knee flexion is equally important. During ground contact, knee flexion serves as a natural shock absorption mechanism, reducing the impact on the knee joint. An appropriate angle of knee flexion helps to disperse the ground reaction forces, lessening the impact on the knee and thereby lowering the risk of injury. Additionally, the correct flexion angle aids in more effectively transferring power during the advancing phase of the gait cycle, with the knee maintaining a slight bend at the moment of contact. Variations in knee flexion angles, either increases or decreases, reflect fatigue in the lower limbs or abnormalities in the lower extremity biomechanics. A proper knee flexion angle also contributes to improving running economy. If the knee flexion angle is too large, it may lead to excessive shear forces and pressure on the knee, increasing the risk of knee injury. A study on the impact of long-distance running on the ankle and knee [57] pointed out that knee flexion (p<0.001) gradually increases with running time. Similarly, Urbaczka [58] studied the effects of fatigue on the kinematics and kinetics of the ankle and knee in healthy nonrearfoot runners and demonstrated a group effect on knee flexion angle at initial contact. Panday [59] investigated the complexity of long-distance running and its relationship with joint movement, comparing elite runners with novice runners, and found that the knee extension angle of elite runners was significantly higher than that of novice runners. These studies suggest that adjusting knee flexion and extension angles in response to fatigue during running may be an effective measure to reduce the risk of injury.
Studies on running-related injuries have consistently indicated that improper joint angles during lower limb movements while running can lead to abnormal gait, which in turn may result in knee injuries. Wearable devices based on sensors are capable of monitoring changes in lower limb joint angles during exercise, and there is existing research [60] that has applied wearable devices to gait analysis during walking and running. In the future, it is anticipated that wearable devices will be used to monitor the kinematic data of lower limb joint movements in runners, providing early warning prompts for abnormal angles, thereby reducing the risk of injury during running and further preventing knee injuries.
Conclusion
Wearable devices, while offering numerous conveniences in healthcare services, still face certain challenges. For instance, there is variability in the precision of angle measurements across different devices, which can lead to significant errors in joint angle measurements and ultimately affect the effectiveness of assessments. Additionally, there are security concerns regarding information leaks during the process of remote rehabilitation systems collecting user data and consolidating it with service providers. These issues require further optimization to be resolved. Overall, the current application of wearable devices in the medical and health field has largely developed a safe, effective, and low-cost method for home-based remote rehabilitation. This has helped many patients with knee joint injuries receive scientific training guidance remotely, achieving high patient compliance and satisfaction during use, while also saving medical resources and alleviating the strain on rehabilitation resources. Wearable devices have also made it possible to collect gait data from patients in a simple manner for gait assessment and have the potential to be applied in gait training after knee surgery. Based on these advantages, wearable devices may also be used in the future for angle monitoring during movement to prevent knee injuries and reduce the risk of sports injuries. Although there are still shortcomings in the current application of wearable devices, with continuous improvements in computer technology and related algorithms, wearable devices are expected to have a broader development prospect and will inevitably play a greater role in the medical and health field in the near future.
Acknowledgement
Beijing Municipal Science & Technology Commission, Administrative Commission of Zhongguancun Science Park (Z221100003522018).
References
- Lu L, Zhang J, Xie Y, Fei Gao, Song Xu, et al. (2020) Wearable health devices in health care: Narrative systematic review. JMIR Mhealth Uhealth 8(11): e18907.
- Khan Y, Ostfeld A E, Lochner C M, Adrien Pierre, Ana C Arias (2016) Monitoring of vital signs with flexible and wearable medical devices. Adv Mater 28(22): 4373-4395.
- Jeong IC, Bychkov D, Searson PC (2019) Wearable devices for precision medicine and health state monitoring. IEEE Trans Biomed Eng 66(5): 1242-1258.
- Loncar-Turukalo T, Zdravevski E, Machado DSJ, Ioanna Chouvarda, Vladimir Trajkovik (2019) Literature on wearable technology for connected health: Scoping review of research trends, advances, and barriers. J Med Internet Res 21(9): e14017.
- Kang K, Geng Q, Xu H (2018) A new wearable device is used in clinical research on rehabilitation after total knee arthroplasty. Chinese Medical Journal 15(98): 1162-1165.
- Chen Q, Shi C, Xu J (2023) Advances in the use of wearable devices in total knee arthroplasty. Shanghai Nursing 23(1): 27-30.
- Haghi M, Thurow K, Stoll R (2017) Wearable devices in medical internet of things: Scientific research and commercially available devices. Healthc Inform Res 23(1): 4-15.
- Jo A, Coronel BD, Coakes CE, Arch G Mainous 3rd (2019) Is there a benefit to patients using wearable devices such as fitbit or health apps on mobiles? A systematic review. Am J Med 132(12): 1394-1400.
- Maddison R, Cartledge S, Rogerson M, Goedhart NS, Singh TR, et al. (2019) Usefulness of wearable cameras as a tool to enhance chronic disease self-management: Scoping review. JMIR Mhealth Uhealth 7(1): e10371.
- Ray PP, Dash D, De D (2017) A systematic review of wearable systems for cancer detection: Current State and challenges. J Med Syst 41(11): 180.
- Jayaraman C, Mummidisetty CK, Mannix-Slobig A, McGee Koch L, Arun Jayaraman (2018) Variables influencing wearable sensor outcome estimates in individuals with stroke and incomplete spinal cord injury: a pilot investigation validating two research grade sensors. J Neuroeng Rehabil15(1): 19.
- Zhou X, Liao X, He L (2021) Application of wearable inertial sensors for the evaluation of human knee joint function. Chinese Journal of Tissue Engineering Research 25(36): 5844-5850.
- Franco T, Sestrem L, Henriques PR, Paulo Alves, Pereira MJV, et al. (2022) Motion sensors for knee angle recognition in muscle rehabilitation solutions. Sensors (Basel) 22(19): 7605.
- Yang C, Shang L, Yao S, Jianbing Ma, Chao Xu, et al. (2023) Cost, time savings and effectiveness of wearable devices for remote monitoring of patient rehabilitation after total knee arthroplasty: Study protocol for a randomized controlled trial. J Orthop Surg Res 18(1): 461.
- Kurtz SM, Higgs GB, Chen Z, Koshut WJ, Tarazi JM, et al. (2023) Patient perceptions of wearable and smartphone technologies for remote outcome monitoring in total knee arthroplasties. J Knee Surg 36(12):1253-1258.
- Abdeen A, Monarrez R, Drew J M, Kennedy KF (2022) Use of a smart-phone mobile application is associated with improved compliance and reduced length of stay in patients undergoing primary total joint arthroplasty of the hip and knee. J Arthroplasty 37(8): 1534-1540.
- Christensen JC, Stanley EC, Oro EG, Carlson HB, Naveh YY, et al. (2022) The validity and reliability of the OneStep smartphone application under various gait conditions in healthy adults with feasibility in clinical practice. J Orthop Surg Res 17(1): 417.
- Xu H, Gao L, Zhao H, Huang H, Wang Y, et al. (2021) Stretchable and anti-impact iontronic pressure sensor with an ultrabroad linear range for biophysical monitoring and deep learning-aided knee rehabilitation. Microsyst Nanoeng 7.
- Riffitts M, Cook H, McClincy M, Bell K (2022) Evaluation of a smart knee brace for range of motion and velocity monitoring during rehabilitation exercises and an exergame. Sensors (Basel) 22(24): 9965.
- Bell KM, Onyeukwu C, McClincy MP, Allen M, Bechard L, et al. (2019) Verification of a portable motion tracking system for remote management of physical rehabilitation of the knee. Sensors (Basel), 19(5): 1021.
- Saggio G, Quitadamo LR, Albero L (2014) Development and evaluation of a novel low-cost sensor-based knee flexion angle measurement system. Knee 21(5): 896-901.
- El FM, Achmamad A, Jbari A, Jilbab A (2023) A convenient approach for knee kinematics assessment using wearable inertial sensors during home-based rehabilitation: Validation with an optoelectronic system. Sci Afr 20: e1676.
- Oubre B, Daneault JF, Boyer K, Kim JH, Jasim M, et al. (2020) A simple low-cost wearable sensor for long-term ambulatory monitoring of knee joint kinematics. IEEE Trans Biomed Eng 67(12): 3483-3490.
- Watson A, Sun M, Pendyal S, Zhou G (2020) TracKnee: Knee angle measurement using stretchable conductive fabric sensors. Smart Heal 15: 100092.
- Sultan KS, Abbosh AM (2022) Wearable dual polarized electromagnetic knee imaging system. IEEE Trans Biomed Circuits Syst 16(2): 296-311.
- World Health Organization, Rehabilitation.
- Xu J, Bao T, Lee UH, Kinnaird C, Carender W, et al. (2017) Configurable, wearable sensing and vibrotactile feedback system for real-time postural balance and gait training: proof-of-concept. J Neuroeng Rehabil 14(1): 102.
- DeMik DE, Carender CN, Glass NA, Callaghan JJ, Bedard NA (2021) Home discharge has increased after total hip arthroplasty, however rates vary between large databases. J Arthroplasty 36(2): 586-592.
- Martina K, Hunter DJ, Salmon LJ, Roe JP, Dowsey MM (2022) Surgery for osteoarthritis: Total joint arthroplasty, realistic expectations of rehabilitation and surgical outcomes: A narrative review. Clin Geriatr Med 38(2): 385-396.
- Hutchinson AG, Gooden B, Lyons MC, Roe JP, O'Sullivan MD, et al. (2018) Inpatient rehabilitation did not positively affect 6-month patient-reported outcomes after hip or knee arthroplasty. ANZ J Surg 88(10): 1056-1060.
- Fleischman AN, Crizer MP, Tarabichi M, Smith S, Rothman RH, et al. (2019) John N. Insall Award: Recovery of knee flexion with unsupervised home exercise is not inferior to outpatient physical therapy after TKA: A randomized trial. Clin Orthop Relat Res 477(1): 60-69.
- Davidovitch RI, Anoushiravani AA, Feng JE, Chen KK, Karia R, et al. (2018) Home health services are not required for select total hip arthroplasty candidates: Assessment and supplementation with an electronic recovery application. J Arthroplasty 33(7S): S49-S55.
- Agostini M, Moja L, Banzi R, Pistotti V, Tonin P, et al. (2015) Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare 21(4): 202-213.
- Hoher J, Lischke B, Petersen W, Mengis N, Niederer D, et al. (2023) Sensor-based telerehabilitation system increases patient adherence after knee surgery. PLOS Digit Health 2(2): e0000175.
- Chen KH, Chen PC, Liu KC, Chan C (2015) Wearable sensor-based rehabilitation exercise assessment for knee osteoarthritis. Sensors (Basel) 15(2): 4193-4211.
- Loo J H, Hai HH, Bin ARH (2022) Effectiveness of sensor-based rehabilitation in improving outcomes in patients undergoing total knee arthroplasty. Surg Technol Int 41: 301-314.
- Cooper DM, Bhuskute N, Walsh G (2022) Exploring the impact and acceptance of wearable sensor technology for pre- and postoperative rehabilitation in knee replacement patients: A U.K.-based pilot study. JB JS Open Access 7(2): e21.00154.
- Dong K, Guo J, Li J (2021) The application effect of smart wearable devices in the home rehabilitation of patients with anterior cruciate ligament reconstruction. Nursing Research 35(15): 2776-2780.
- Harvey A, Gorter JW (2011) Video gait analysis for ambulatory children with cerebral palsy: Why, when, where and how!. Gait Posture 33(3): 501-503.
- Daly JJ, Nethery J, McCabe JP, Brenner I, Rogers J, et al. (2009) Development and testing of the Gait Assessment and Intervention Tool (G.A.I.T.): a measure of coordinated gait components. J Neurosci Methods 178(2): 334-339.
- Ma C, Li W, Cao J, Juan Du, Qimeng Li, et al. (2020) Adaptive sliding window based activity recognition for assisted livings. Information Fusion 53: 55-56.
- Boekesteijn R, Smolders J, Busch V, Keijsers N, Geurts A, et al. (2022) Objective monitoring of functional recovery after total knee and hip arthroplasty using sensor-derived gait measures. Peer J 10: e14054.
- Kobsar D, Masood Z, Khan H, Khalil N, Yossri Kiwan M, et al. (2020) Wearable inertial sensors for gait analysis in adults with osteoarthritis-a scoping review. Sensors (Basel) 20(24): 7143.
- Hameed D, Sodhi N, Dubin J, Schneider A, Barrack RL, et al. (2024) Integrating smartphone applications and wearable devices for postoperative rehabilitation in total knee arthroplasty: A critical review. J Arthroplasty 39(8): 2028-2039.
- Feng Y, Liu Y, Zhou J (22023) Advances in the application of wearable inertial sensors in gait analysis after total knee arthroplasty. Leather Science & Engineering 33(6): 52-58.
- Boekesteijn RJ, Gerven J, Geurts ACH, Smulders K (2022) Objective gait assessment in individuals with knee osteoarthritis using inertial sensors: A systematic review and meta-analysis. Gait Posture 98:109-120.
- Wang S, Chan PPK, Lam B, Chan ZYS, Zhang JHW, et al. (2021) Sensor-based gait retraining lowers knee adduction moment and improves symptoms in patients with knee osteoarthritis: A randomized controlled trial. Sensors (Basel) 21(16): 5596.
- Shi B, Chen X, Yue Z, Yin S, Weng Q, et al. (2019) Wearable ankle robots in post-stroke rehabilitation of gait: A systematic review. Front Neurorobot 13: 63.
- Saygin D, Oddis CV, Moghadam-Kia S, Rockette-Wagner B, Neiman N, et al. (2021) Hand-held dynamometry for assessment of muscle strength in patients with inflammatory myopathies. Rheumatology (Oxford)60(5): 2146-2156.
- Deones VL, Wiley SC, Worrell T (1994) Assessment of quadriceps muscle performance by a hand-held dynamometer and an isokinetic dynamometer. J Orthop Sports Phys Ther 20(6): 296-301.
- Myong Y, Park S, Cho M, Cho SY, Lee WH, et al. (2023) Development and validation of a portable articulated dynamometry system to assess knee extensor muscle strength. Sci Rep 13(1): 11887.
- Park S, Myong Y, Cho M, Cho SY, Lee WH, et al. (2024) Design and validation of a wearable dynamometry system for knee extension-flexion torque measurement. Sci Rep 14(1):10428.
- Luo J, Li Y, He M, Wang Z, Li C, et al. (2022) Rehabilitation of total knee arthroplasty by integrating conjoint isometric myodynamia and real-time rotation sensing system. Adv Sci (Weinh) 9(8): e2105219.
- Noehren B, Hamill J, Davis I (2013) Prospective evidence for a hip etiology in patellofemoral pain. Med Sci Sports Exerc 45(6): 1120-1124.
- Noehren B, Davis I, Hamill J (2007) ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech (Bristol, Avon) 22(9): 951-956.
- Dudley RI, Pamukoff DN, Lynn SK, Kersey RD, Noffal GJ, et al. (2017) A prospective comparison of lower extremity kinematics and kinetics between injured and non-injured collegiate cross country runners. Hum Mov Sci 52: 197-202.
- Wilhoite S, Mutchler JA, Barry AM, Li LI (2021) Ankle-knee initial contact angle and latency to maximum angle are affected by prolonged run. Int J Exerc Sci 14(1):33-44.
- Urbaczka J, Silvernail JF, Jandacka D (2022) The effect of fatigue on the ankle and knee kinematics and kinetics in moderately and highly trained healthy non-rearfoot runners. Sports Biomech, pp. 1-15.
- Panday SB, Pathak P, Moon J, Koo D (2022) Complexity of running and its relationship with joint kinematics during a prolonged run. Int J Environ Res Public Health 19(15): 9656.
- Benson LC, Clermont CA, Bosnjak E, Ferber R (2018) The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture 63: 124-138.
© 2024 Jianquan Wang. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






