- Submissions

Full Text
Developments in Clinical & Medical Pathology
Cognitive Impairment in Patients Operated for Non-traumatic Intracranial Hemorrhage
NE Ivanova1*, М Yu Efimova1,2, AO Makarov1, AE Tereshin1, DA Reshetnik1 and A Yu Ivanov3
1Nikolaev Hospital, Saint-Petersburg, Russia
2National Medical Research Center named after V.A. Almazov” Ministry of Health of the Russian Federation, Russia
3St. Petersburg State Pediatric Medical University, Ministry of Health of the Russian Federation, Russia
*Corresponding author: NE Ivanova, Nikolaev Hospital, Saint-Petersburg, Peterhof, Russia
Submission: August 12, 2019;Published: August 21, 2019
ISSN:2690-9731 Volume2 Issue1
Summary
The article is devoted to the peculiarities of cognitive status in patients operated for non-traumatic intracranial hemorrhages. An assessment of the severity of cognitive impairment was carried out in the observations of different etiology hemorrhages. An analysis of the relationship between the localization and the hematoma, and the severity of disorders of higher cortical functions was carried out. Understanding the cognitive deficiency patterns in neurosurgical patients is important for effective rehabilitation measures.
Keywords: Non-traumatic intracranial hemorrhage; Cognitive impairment; aneurysmal disease, MMSE
Topicality
BBlood stroke is the most important cause of disability occurrence in the population of developed countries. Non-traumatic intracranial hemorrhages compose 10 to 20% of cerebral circulation disorders [1]. Only 12% - 39% of patients can subsequently return to fullfledged life after a blood stroke [2]. One of the adverse effects of non-traumatic intracranial hemorrhage is the impairment of higher cortical functions. Post-stroke cognitive disorders are moderately pronounced in 37-71% of cases, and they reach the degree of dementia in 4-40% of cases [3]. At that, they are heterogeneous in a pathogenic and clinical way, which affects their curability and prognosis. This study objective is to assess the severity of cognitive impairment in patients operated for non-traumatic intracranial hemorrhages of different etiology and localization.
Material and Methods
The results of neuropsychological testing of 54 patients (18 men and 36 women, mean age of 47.56±13.54 years old) aimed at rehabilitation treatment after non-traumatic intracranial hemorrhage was analyzed. Among them, 16 patients underwent aneurysm clipping (29.63%), 9 ones (16.67%)-aneurysm embolization, 18 ones (33.33%)-hematoma removal at hypertensive hemorrhage, 1 patient (1.85%)-angioma removal, and 10 ones (18.52%) - embolization of arteriovenous malformation (AVM). The state evaluation of higher cortical functions was carried out by a neuropsychologist applying MMSE, FAB scales on the day of admission.
Results and Discussion
The MMSE scale testing revealed that patients scored from 28 to 30 points (normal variant) in 9 (16.67%) cases, from 24 to 27 points (predementing violations) in 23 (42.59%) cases, from 20 to 23 points (mild dementia) in 8 (14.81%) cases, and, finally, from 11 to 19 points (dementia of moderate severity) in 14 (25.93%) cases. The average MMSE score demonstrated 23.04±6.15 points. When assessing the degree of frontal dysfunction using the FAB scale, the following results were obtained: 21 (38.89%) subjects of the study scored from 16 to 18 points, which corresponded to the norm value, 19 (35.19%) subjects of the studied scored from 12 to 15 points, which corresponded to moderate frontal dysfunction, 14 (25.93%) subjects scored less than 12 points, which corresponded to severe frontal dysfunction. The average FAB score totaled 13.91±3.98 points.
Like for any focal brain lesion, in case of non-traumatic intracranial hemorrhage, the presence and localization of intracerebral hematoma plays an important role in the formation of cognitive deficiency. In this study, intracerebral hematoma occurred in 44 (81.48%) cases, and isolated subarachnoid hemorrhage occurred in 10 (18.52%) cases. Table 1 reflects the testing results for the patients with non-traumatic intracranial hemorrhage of different localization.
The Table 1 shows that the most pronounced cognitive impairment was observed in patients with thalamic and subcortical hemorrhages. Subcortical hemorrhages affect the tertiary zones of the cortical representation of higher brain functions, while thalamic ones, apparently, have a negative impact on cognitive functions, both due to the separation of cortical-subcortical structures, and due to the damage of specific thalamic nuclei [4]. Hemorrhages in the cerebellum were accompanied by the least cognitive impairment. The pathophysiological aspects of the cognitive deficiency formation in the event of cerebellum structure damage have not been studied to date. The literature describes the so-called “cerebellar cognitive affective syndrome” represented mainly by secondary impairment of executive functions [5]. However, disorders of higher brain functions reaching the degree of dementia have been described only at extensive pathological processes affecting, in addition to the cerebellum, other brain structures as well [6].
Table 1: The cognitive status of patients operated for non-traumatic intracranial hemorrhage, upon admission, depending on its location.

Note: *** - reliability of statistical differences (p <0.05).
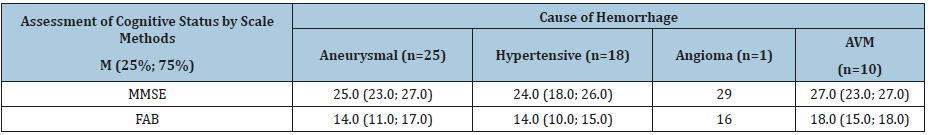
Table 2 shows the results of the cognitive status comparison of patients with different etiologies of non-traumatic intracranial hemorrhages. As can be seen from Table 2, the mildest cognitive deficiency was described in those who underwent hemorrhage from AVM. This is consistent with literature data, according to which a more favorable outcome for hemorrhages from AVM compared with those with aneurysmal and hypertensive disease can be explained by a slight pressure inside the vascular formation, the presence of factors contributing to thrombosis, and a low frequency of vasospasm [7]. The most pronounced cognitive impairment was accompanied by hypertensive hemorrhage. The severity and disabling consequences of hypertensive hemorrhage are largely due to the high incidence of dislocation syndrome. In addition, hypertension with poorly controlled high blood pressure numbers is an independent risk factor for cognitive deficiency. In patients with aneurysmal hemorrhages, moderate impairments of higher brain functions were found during the admission, corresponding, on average, to the level of predementing disorders.
Table 2: Cognitive status of patients with different etiologies of non-traumatic intracranial hemorrhages during admission.
The severity of the patient’s condition, as well as the incidence of dislocation syndrome in the presence of hematoma, is largely determined by its volume. According to the literature, hematoma volume in excess of 30 cm3 is an adverse prognostic factor [2]. Table 3 shows the results of the cognitive status comparison of subjects with intracerebral hematomas of different volume. As Table 3 demonstrates, there is a fairly clear relationship between hematoma volume and cognitive impairment severity. Hematomas of small volume were accompanied by a significantly less pronounced cognitive deficiency than hematomas with a volume of more than 50cm3. When comparing the volume of hematomas with the test indicators, a strong positive correlation was found: r =+ .83.
Table 3: Cognitive status of patients depending on intracerebral hematoma volume.

Note: * - reliability of statistical differences (p <0.01).
Conclusion
Thus, the formation and severity of cognitive impairment in non-traumatic intracranial hemorrhages are affected by a number of factors, including the etiology of hemorrhage, localization and size of hematoma.
References
- Liu S, Liu X, Chen S, Xiao Y, Zhuang W (2019) Neutrophil-lymphocyte ratio predicts the outcome of intracerebral hemorrhage: A meta-analysis. Medicine (Baltimore) 98(26): e16211.
- An SJ, Kim TJ, Yoon BW (2017) Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke 19(1): 3-10.
- Cai Z, Wang C, He W, Tu H, Tang Z, et al. (2015) Cerebral small vessel disease and Alzheimer’s disease. Clin. Intervt Aging 10: 1695-1704.
- Fisher CM (1959) The pathologic and clinical aspects of thalamic hemorrhage. Transaction Am neurol associate 84: 56-59.
- Ladurner G, Kaivach P, Moessler H (2005) Neuroprotective treatment with cerebrolysin in patients with acute stroke: a randomised controlled trial. J neural transmis 112(3): 415-428.
- Hier DB, Cummings JL (1990) Rare acquired and degenerative subcortical dementias. In: JL Cummings (Ed.), Subcortical dementia. Oxford University Press, New York, USA.
- Hartmann A, Mast H, Mohr JP (1998) Morbidity of intracranial hemorrhage in patients with cerebral arteriovenous malformation. Stroke 29(5): 931-934.
© 2018 NE Ivanova. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






